Abstract
This article outlines a practical approach to quickly implementing virtual care for physiatrists. This skill is relevant not only during times of a pandemic, when face to face care is impossible, but is also valuable when caring for patients who have physical, financial, logistic, or other challenges to on-site care. Key themes covered in this article include selecting appropriate virtual care platforms, consenting patients for virtual care and conducting successful virtual visits. It also reviews strategies for performing virtual physical examinations and engaging learners in virtual care.
Key Words: Practice Management, Telemedicine, Pandemics, Physical and Rehabilitation Medicine
Virtual care is a broad term that encompasses all means of care delivery that occur outside of face to face clinical interaction; telephone calls, video visits, e-consultations (asynchronous provider to provider electronic communication), secure messaging and e-mail all fit within the definition. Although this article was written during the COVID-19 pandemic, virtual care offers one solution to providing care during future times of necessary physical distancing and reduction in non-essential clinical services.
Virtual care has many advantages and applications for inpatient and outpatient physical medicine and rehabilitation patients.1,2 Patients engaging in virtual care report decreased time and money spent traveling, more convenient care, and better care access.3,4 Patient populations with high disability burden, such as those in long-term care facilities, have been show to particularly benefit from virtual visits.5 Physicians using virtual care have reported improved care efficiency by seeing more patients per day and by recording fewer missed appointments.3 Economic evaluations of virtual care have demonstrated system-wide cost-effectiveness in many medical fields.6 There are minimal requirements for physical spaces, as entire clinics can run from the physician’s office or home. Platforms that offer e-consultation facilitate interspecialty communication and reduce delays to accessing specialist care.7 Inpatient consultations and visits can be done virtually as well to provide service to remote patients or to limit risk of patient/clinician infection transmission. Outside of pandemic times, virtual care can greatly improve care access for geographically remote and underserviced areas8 or for patients who have physical, financial, logistic, or other challenges to on-site care.
Several barriers to performing virtual care have been reported in the literature, although many of these can be overcome with sufficient planning. Technological glitches may introduce delays,2 and some patients may not have the necessary equipment to participate. Many physical medicine and rehabilitation patients have cognitive, hearing, and visual impairments or may have language barriers because of aphasia or different first languages. There may be associated costs with some virtual care platforms, as well as substantial technological work to install and test cameras and speakers. Furthermore, significant training of clinicians and administrators is typically required.2 There are also challenges with adding regional billing components for virtual care into existing billing software, which may also require inputting new visit or encounter types. Some virtual technologies are not approved for medical use, so there is the risk of confidentiality issues if the connection is unsecured.2 Complete physical examination cannot be performed, and there may be medico-legal concerns with conducting partial assessments.9 Finally, some physiatry practices include a variety of procedural care services (e.g., electrodiagnostic studies or injections) that cannot be performed virtually.
The barriers listed above may explain why virtual care uptake has been relatively slow, despite availability of adequate technology for several years. Cultural acceptance of telehealth services among providers has been challenging in general owing to the changes required for successful adoption.10 However, in the current pandemic environment, there is a greater need for ways to address patient needs without face to face visits. In this article, a practical approach that addresses many of these concerns is presented, in hopes of making virtual care a more accessible, complimentary tool for the physiatrist, in both times of pandemic and thereafter.
SELECTING AN APPROPRIATE VIRTUAL CARE PLATFORM
The most feasible way to begin practicing virtual care during times of systematic strain is simply through telephone. Audio-only care has become a billable clinical service in many regions because of the pandemic; general requirements for consent and documentation are detailed in the next section of this report. Most patients will have access to a telephone and will have provided at least one contact number during the process of referral or registration. The upside to telephone care is that it is a relatively secure means of contacting patients, and patients do not require any set up or training to participate. Up to 80% of the clinical impression is formed based on history,11 which can be readily obtained through telephone assessment. After connecting with patients on the telephone, the physiatrist can choose to schedule a follow-up video visit or arrange for an in-person visit if warranted. If the physiatrist ascertains the most likely diagnosis, they can start the patient on rehabilitation or other management strategies. Alternatively, they may have gathered enough information to proceed with investigations or referrals or arrange for needed services and equipment.
The major downside of a telephone-only encounter is the lack of visual input. Video greatly supports the diagnostic encounter by allowing limited physical examination and assists with building clinician-patient rapport. Many platforms exist for conducting video visits; some may be available only regionally, whereas others are global companies. There is a large range in cost and available services among the options. Consideration should be given to whether the software is locally approved for medical use, which typically includes encryption for protection of personal health information.
Some digital platforms can integrate into electronic medical record systems. Integration may support functions such as scheduling or sending reminders to patients and provides a smooth end-user experience for the provider. Some platforms require patients to download apps or other software, whereas others simply require patients to click a link and enter the visit through a web browser. There may be the option to offer messaging with patients through a secure portal, which can either supplement the synchronous telephone or video visit or replace it altogether (in the case of a simple follow-up request, for example). Integration of virtual care with electronic medical record and patient portals offers several additional benefits: the patient can access provider documentation, radiology, and laboratory test results and can use integrated medical history questionnaires. The patient can also upload photos or advanced imaging for provider review. Consideration may also be given to integration of staff workflow tools and questionnaires such as those used for screening, history, and medication review. Such tools can be used for regional quality improvement work that traditional requires on-site data collection.
Some virtual care platforms have functions that extend beyond direct patient care. Many offer videoconferencing, which can be used for administrative purposes. This is helpful not only in times of physical distancing but also for multisite organizations or for places where large spaces are restricted. Videoconferencing functions are also very useful for conducting continuing education sessions or as part of trainee education programs. Multidisciplinary assessments and rehabilitation treatment interventions may also be performed using videoconferencing.1
The factors listed above are some of the considerations when selecting the digital platform that will best serve individual providers and their patients. In general, one can start off with simple systems that most patients have access to, before purchasing more complex systems. Friends and family members are helpful resources for trying new technology before the patient visit. To mitigate the technological challenges raised, it is helpful to have strong involvement from information technology specialists and clinical informaticists, who can design appropriate workflows and troubleshoot issues as needed. Training for end users can be achieved through provider-facing e-learning videos with workflow demonstration; it is also helpful to have tip sheets available for quick reference. Similarly, patients can be prepared through calls ahead of time with support staff or through patient-facing education videos that detail equipment set up and use.
PREPARING FOR THE VIRTUAL VISIT
Just as with face to face care, administrative support is vital to a successfully managed virtual care practice. To eliminate the need for paper faxing, clinics can create e-mail referral accounts to send and receive referrals, use online electronic fax (e-fax), or see whether their electronic medical record has e-fax capabilities. Administrators should collect patients’ pharmacy information in advance of the appointment to allow for prescribing after the visit, which can be done via phone, secure e-mail, or e-fax. Administrators should also instruct patients to either submit their medication list in advance or have it on hand for the visit. Patients should be available at least 15 mins before their appointment to “check in” to the virtual waiting room. They should be prepared to wait at least 30 mins after their scheduled appointment time, recognizing that virtual clinics may run behind schedule, similar to in-person clinics. Providers should receive instructions for blocking their personal phone number for security, and patients should be notified that their appointment call may come from a blocked number. Reminders should be provided to patients about their upcoming virtual visits in the same way as for in-person visits.
If conducting video visits with a patient at home, they will need to have Internet access and a device capable of making video calls. Some platforms also require an e-mail address, which is used to initiate the visit. It is advised that the patient conduct a test of their equipment in advance of the appointment, to reduce time spent in the appointment troubleshooting. Patients should be provided with technology support contact numbers and information whenever possible. In the event that technology fails during the visit, having a telephone number for the patient is important as a back-up means of connecting with the patient to start the assessment or assist with video connection success.
Some physical medicine and rehabilitation patients will not have the ability to participate in video visits at home, for technological reasons or owing to burden of disability. In that event, telehealth centers exist in many regions to support patients. Visits can be scheduled in conjunction with the telehealth center, and the patient physically presents to the center for check-in. Administrative support is available on site, and the visit will be set up for the patient, eliminating the need for technological knowledge. Telehealth centers may also have personnel available to assist with the physical examination.
Patients and providers may be hesitant to try virtual care if they have never used it before. Information framing12 can be used as a way of encouraging eligible participants, which is especially important during pandemic times when other options may not be available. For example, rather than offering the patient a choice of virtual or in-person care, they can be notified that their visit will take place virtually on the prearranged date; however, they may choose telephone or video for the initial encounter. Bulk messaging of patients rostered to patient portals can also be used as a means of providing education about virtual care and encouraging its use. The major caveat is that virtual visits may not be possible for patients with severe cognitive, hearing, or visual impairments without a caregiver present.
CONDUCTING THE VIRTUAL VISIT
The virtual visit should begin with identity verification by the provider or by administrative staff; options include stating date of birth or showing a photo identification card. An alternative to this is to use identity verification software through a patient portal; some institutions have contracts with third-party resources to accomplish this in advance of the appointment. The next step is a structured consent process2; for specific legal issues, the clinician should consult with their local licensing authority; however, general principles will be reviewed. If using telephone, e-mail, or secure messaging, it is important to make the patient aware that a physical examination will not be completed, whereas it would have occurred in person. Although video visits include a limited physical examination, clinicians should still explicitly state that this technology cannot replace the need for in-person physical examination or assessment of some disorders. Clinicians should state that in the event of urgent conditions, patients must seek care in an emergency department as necessary. Finally, patients should be notified of the risks related to unauthorized disclosure or interception of personal health information2 and should be provided with strategies to mitigate this risk when possible.
When conducting the virtual visit, clinicians should ensure that their space is private and protected for the duration of the visit.13 If at home or office space with others, one strategy is to place a sign on the door signifying that “an appointment is in progress.” If using a camera, the position should frame the clinician’s head and shoulders, with good lighting that minimizes glare and shadows.13 Ideally, a solid background should be used and neutral outfit worn to minimize distractions.13 It may be helpful to have a set-up that includes two monitors, so that one screen can be used for the video visit, and the other can be used for documentation or chart review. The clinician can reduce the risk of technical difficulties by testing Internet speed in advance of the appointment and by closing any programs not in use to preserve bandwidth.
After the encounter, the documentation process is similar to that which follows in-person visits. There should be an additional paragraph dedicated to documenting the virtual consent process as outlined above. If the patient requests to record the visit and has the capability to do so, the clinician can make an individual determination based on his/her comfort level. If a recording is to be made, everyone in the recording on both sides of the screen should consent in advance. Secure storage of the video must be ensured, and all parties should be aware of the risk of improper dissemination. Recordings must not be used for nonclinical purposes such as social media posts, conference presentations, or hospital presentations unless explicit consent has been given to distribute in such a manner. Additional guidelines around recording visits and storing recordings may be available from local licensing authorities.
THE VIRTUAL PHYSICAL EXAMINATION
A study by Ansary et al.14 analyzed the various components of physical examination and assigned a confidence-level rating based on a low, medium, and high feasibility to perform virtually. These authors reported that the virtual musculoskeletal examination is largely limited to inspection and range of motion.14 Although palpation and special tests are highly dependent on clinician administration, patients can attempt self-palpation under physician direction, and caregivers or spouses can provide resistance for strength testing. Substituting weights for clinician-applied resistance may also serve as a standardized means of conducting strength testing if these are available in the patient’s home. Functional strength testing such as getting the patient to attempt a sit-to-stand transfer or lift off a chair using triceps may also be useful in a virtual visit environment.
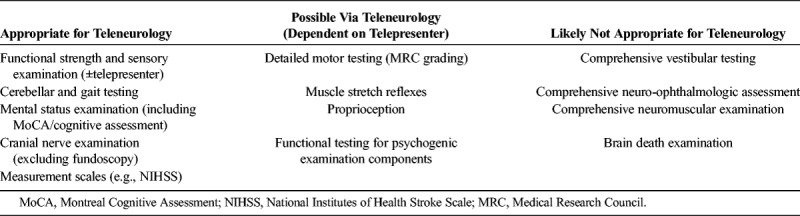
Many elements of the neurologic examination are reported as highly feasible to perform virtually in the literature (Table 1).15 These components include mental status, functional strength and sensory examination, cerebellar function,16 gait, cranial nerves III to XII, and tremor assessment.14,15 Other elements, such as detailed motor testing using Medical Research Council grading, muscle stretch reflexes, or proprioception, can be accomplished using trained telepresenters at regional telehealth centers.8,14,15 A telemedicine clinic for amputee patients used a trained coordinator to position the camera and the patient’s residual limb for inspection; the coordinator also performed palpation of the residual limb.4 Using this model, the clinic demonstrated reliable assessment as well as high patient satisfaction with the quality of care received.4 In pandemic times or when patients are unable to have a trained coordinator, caregivers or family members may also be able to assist in some aspects of the physical examination with the patient’s consent.
TABLE 1.
Examination components suitable for teleneurology15
ENGAGING LEARNERS IN VIRTUAL CARE
As outlined in this article, virtual care has many principles that take practice to integrate into daily care. As such, learners may benefit from developing these skills during their training, with dedicated knowledge and practical components.15 Some digital platforms permit trainees to join from separate locations as observers or assessors, which is beneficial if physical distancing is required. Senior trainees can conduct initial telephone or video assessments and can conference their supervisor into the encounter after reviewing, or review cases on the phone similar to on-call models. Many educational institutions are shifting toward Competency Based Medical Education, which requires trainees to produce a greater proportion of observed clinical encounters. Virtual care is well suited to this model of education, as supervisors can observe video encounters remotely, and can also provide direct, integrated feedback.
CONCLUSION
Virtual care is particularly important during the COVID-19 pandemic but is also a valuable supplemental clinical tool for the physiatrist outside of pandemic times. Virtual care may be the solution to care inequalities that exist for remote populations, or those with barriers to on-site care for other reasons. This article outlines a practical approach to providing virtual care for the physical medicine and rehabilitation patient population and addresses some of the challenges previously reported in the literature.
ACKNOWLEDGMENTS
The authors thank Dr Ilana Halperin, Dr Alexandra Rendely, and Dr Paul Winston for their valuable contributions to discussions about virtual care.
Footnotes
All authors contributed significantly to the paper and confirmed the final version.
McKyla McIntyre is in training.
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
REFERENCES
- 1.Tenforde AS, Hefner JE, Kodish-Wachs JE, et al. : Telehealth in physical medicine and rehabilitation: A narrative review. PM R 2017;9(5s):S51–8 [DOI] [PubMed] [Google Scholar]
- 2.Gregory P, Alexander J, Satinsky J: Clinical telerehabilitation: Applications for physiatrists. PM R 2011;3:647–56 quiz 656 [DOI] [PubMed] [Google Scholar]
- 3.Women’s College Hospital Institute for Health Systems Solutions and Virtual Care (WIHV). Enhanced access to primary care: Project evaluation final report. Available at: https://otn.ca/wp-content/uploads/2019/08/eapc-evaluation-report.pdf. Accessed April 1, 2020
- 4.Linassi AG, Li Pi Shan R: User satisfaction with a telemedicine amputee clinic in Saskatchewan. J Telemed Telecare 2005;11:414–8 [DOI] [PubMed] [Google Scholar]
- 5.Edirippulige S, Martin-Khan M, Beattie E, et al. : A systematic review of telemedicine services for residents in long term care facilities. J Telemed Telecare 2013;19:127–32 [DOI] [PubMed] [Google Scholar]
- 6.Delgoshaei B, Mobinizadeh M, Mojdekar R, et al. : Telemedicine: A systematic review of economic evaluations. Med J Islam Repub Iran 2017;31:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liddy C, Moroz I, Mihan A, et al. : A systematic review of asynchronous, provider-to-provider, electronic consultation services to improve access to specialty care available worldwide. Telemed J E Health 2019;25:184–98 [DOI] [PubMed] [Google Scholar]
- 8.Wechsler LR: Advantages and limitations of teleneurology. JAMA Neurol 2015;72:349–54 [DOI] [PubMed] [Google Scholar]
- 9.Wechsler LR, Tsao JW, Levine SR, et al. : Teleneurology applications: Report of the Telemedicine Work Group of the American Academy of Neurology. Neurology 2013;80:670–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harst L, Lantzsch H, Scheibe M: Theories predicting end-user acceptance of telemedicine use: Systematic review. J Med Internet Res 2019;21:e13117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hampton JR, Harrison MJ, Mitchell JR, et al. : Relative contributions of history-taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients. Br Med J 1975;2:486–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moxey A, O’Connell D, McGettigan P, et al. : Describing treatment effects to patients. J Gen Intern Med 2003;18:948–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ontario Telemedicine Network: Videoconferencing best practices. Available at: https://support.otn.ca/sites/default/files/videoconferencing_best_practices.pdf. Accessed April 2, 2020
- 14.Ansary AM, Martinez JN, Scott JD: The virtual physical exam in the 21st century. J Telemed Telecare 2019;1357633x19878330. [DOI] [PubMed] [Google Scholar]
- 15.Govindarajan R, Anderson ER, Hesselbrock RR, et al. : Developing an outline for teleneurology curriculum: AAN Telemedicine Work Group recommendations. Neurology 2017;89:951–9 [DOI] [PubMed] [Google Scholar]
- 16.McIntyre M: The virtual physical exam—cerebellar screen video. 2020. Available at: https://youtu.be/pQO-uYmWu-Y. Accessed April 3, 2020


