Abstract
As physicians specializing in rehabilitation medicine consider sequelae from the novel coronavirus pandemic that began in 2019, one issue that should be top of mind is the physiologic effect that large-scale social distancing had on the health of patients in general but, more specifically, on preoperative patients who had their surgeries delayed or will have newly scheduled procedures during the peripandemic period. Predictably, as the virus becomes less prevalent, there will be a tremendous motivation to move forward with scheduling operations from both patient care and institutional perspectives. However, one can anticipate a pandemic-related increase in surgical morbidity and mortality above prepandemic levels, particularly in older or medically frail patients even if they did not have a novel coronavirus (i.e., COVID-19) infection. Therefore, now is the time to consider for patients awaiting surgery a wider adoption of prehabilitation—physical and psychological assessments that establish a baseline functional level, identify impairments, and provide interventions that promote physical and psychological health to reduce the incidence and/or severity of future impairments.
Key Words: Rehabilitation, Prehabilitation, Physical and Rehabilitation Medicine, Perioperative Care, Preoperative Care, Preoperative Period, Pandemics
As physicians specializing in rehabilitation medicine consider sequelae from the novel coronavirus pandemic that began in 2019 and is referred to as COVID-19, one issue that should be top of mind is the physiologic effect that large-scale social distancing had on the health of patients in general but, more specifically, on preoperative patients who had their surgeries delayed. Operating rooms, which, for safety purposes, were shuttered or running at a fraction of their usual capacity, will likely swing their doors wide open as soon as possible to meet (1) patients’ pent-up demand for the surgical portion of their care and (2) hospital administrators’ need for help with recovery of their institutions’ financial standing. Although we can anticipate that patient care will proceed with the usual care and caution, we may also anticipate one crucial caveat—a pandemic-related increase in surgical morbidity and mortality above prepandemic levels, particularly in older or medically frail patients even if they did not have a novel coronavirus (i.e., COVID-19) infection. A theoretical and logical solution for this situation is to offer prehabilitation—a set of preoperative interventions that have been previously studied in a variety of populations with promising results1—to patients waiting for surgery.
REASSESSING SURGICAL RISK
Calculating surgical risk for any patient involves science combined with a surgeon’s experience and instinct. As operations begin to ramp up after the social distancing hiatus, it is conceivable to assume that some patients’ surgical risk changed (either increased or decreased, depending on a variety of factors) from baseline prepandemic levels (Fig. 1). The lowest risk patients are likely the relatively young, healthy individuals who were able to increase their physical activity level and positive health habits during the pandemic and either were not infected or did not have a significant enough infection to warrant bed rest or convalescence. On the other end of the spectrum are the highest-risk patients who were medically frail at baseline, survived a recent COVID-19 infection, experienced hospitalization and significant period of bed rest and/or convalescence, and may be affected by serious infection-related sequelae. Because of the global nature of the disease spread, the health status of a large proportion of the world’s population likely changed during the COVID-19 pandemic. Therefore, all patients who were assessed for surgery prepandemic should be reassessed before undergoing any peri- or postpandemic operation. Moreover, all new surgical patient evaluations should take into account pandemic-related variables that may have increased or decreased surgical risk, with particular caution warranted in elderly or medically frail patients.
FIGURE 1.
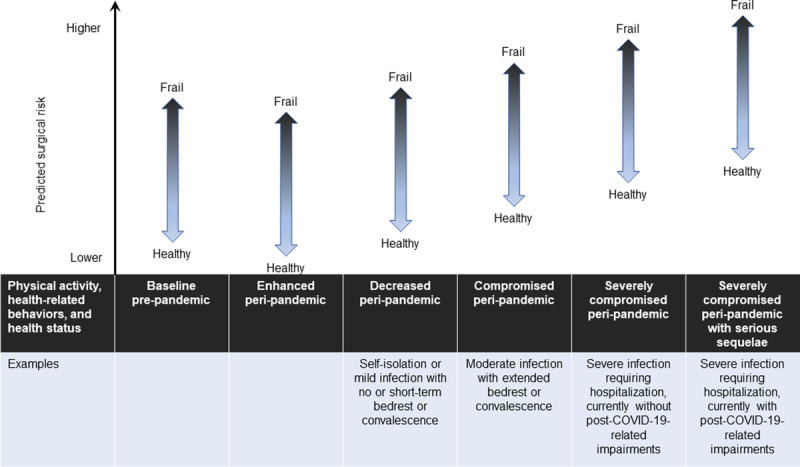
Changes in predicted surgical risk during the COVID-19 pandemic. Postpandemic surgical risk will likely be affected by peripandemic patient physical activity, health-related behaviors, and health status. Those able to enhance peripandemic physical activity and health-related behaviors may be able to improve surgical risk. However, those whose activity and behaviors are decreased because of self-isolation restrictions or mild infection may experience a worsening of risk. Those most likely to experience significant worsening of risk are those with severe infections who experience extended periods of bed rest or convalescence, hospitalization, and sequelae.
Indeed, for those patients in which social distancing recommendations or a COVID-19 infection resulted in less physical activity from their usual baseline, we can expect an increase in physiologic operative stress related to cardiopulmonary deconditioning or changes in other behaviors that are well documented to be associated with increased surgical risk, such as poor nutrition, increased tobacco use, or diminished glycemic control. Other contributing factors may include but are not limited to advanced immunocompromised status (e.g., oncology patients receiving neoadjuvant therapy for a longer period than anticipated secondary to alteration of protocols during the pandemic), an increase in smoking or alcohol or other substance use or abuse, and deterioration in mental health status. Higher than usual levels of physiologic stress alone will almost certainly translate into an increase in surgical morbidity and mortality statistics across all ages and premorbid health categories.
There is a large body of published research on surgical risk in patients who are deconditioned or otherwise medically compromised, and this literature should serve as a cautionary sign and encourage reassessment of surgical risk in all patients. To better understand surgical risk before the pandemic in medically frail patients, we can look to a recent study in which Shinall et al.2 analyzed a large cohort of patients in the Veterans Administration Surgical Quality Improvement Program using a novel operative stress score. This study involved 432,828 unique patients (401,453 males [92.8%]) with a mean age of 61.0 yrs who underwent noncardiac surgical procedures. The authors compared the mortality rates of patients who were deemed frail (n = 36,579 [8.5%]) or very frail (n = 9113 [2.1%]) with a commonly used metric that defines high risk surgery as a 30-day mortality rate of 1%.
The 30-day mortality rate among patients who were frail and underwent what the authors described as the lowest-stress surgical procedures (e.g., cystoscopy) was 1.5%. The 30-day mortality rate increased to 5.1% in patients who were frail and underwent moderate-stress procedures (e.g., laparoscopic cholecystectomy). Among the very frail group, 30-day mortality rates were 10.3% and 18.7% after surgeries categorized as lowest and moderate stress, respectively. Moreover, the researchers in this study found that patients who were frail and very frail had rising mortality rates at 90 and 180 days, reaching 43.0% for very frail patients at 180 days after moderate-stress surgical procedures. Shinall et al.2 concluded that “frailty screening should be applied universally because low- and moderate-stress procedures may be high risk among patients who are frail.”
At the time of this report, millions of people have already been infected with the novel coronavirus and many more will become infected in the future. The older people and those with more than one comorbidity are at a particularly high risk of death from COVID-19.3 Individuals who are severely affected and survive, regardless of age, may experience a wide variety of sequelae that involve the cardiopulmonary and neuromuscular systems.4 It is anticipated that people with prolonged hospitalizations, particularly in the intensive care unit, will initially be much frailer than they were before infection and will benefit from postacute rehabilitation care. Although data are limited at this time, some individuals will not return to their baseline health status and will live with permanent disability.
Given the improvements seen in patient status after use of prehabilitation protocols, it seems important to consider incorporating prehabilitation more widely into the surgical care continuum to prepare patients, particularly medically frail individuals, who have been affected by COVID-19–related concerns, whether they have had an infection or not.
HISTORICAL AND MODERN DAY PREHABILITATION
By definition, prehabilitation is focused on preparing people for an upcoming physiologic stressor. The British Medical Journal published an early report on a prehabilitation program that included a cohort of approximately 12,000 men preparing for World War II.5 The soldiers lived in centers for an average of 2 mos during which they participated in a regular exercise regimen, had access to nutritious food, and developed a sense of community. The report stated that health status was raised no less than 85% and that this was an “astonishingly easy accomplishment.”
A modern day definition for prehabilitation includes “physical and psychological assessments that establish a baseline functional level, identify impairments, and provide interventions that promote physical and psychological health to reduce the incidence and/or severity of future impairments.”6 Prehabilitation has been used sporadically in medicine, particularly in preparing people for an upcoming surgery. However, the evidence base has grown exponentially during the past few years, although the terms used to describe this type of intervention vary. For example, a PubMed search done in March 2013 revealed 57 publications for “prehabilitation” and 4502 for “preoperative rehabilitation.”7 When these same search terms were used in PubMed approximately 7 yrs later (April 2020), 551 (10 times more) and 9852 (2 times more) publications were identified, respectively. Despite this growth and the literature containing many reports with experts supporting clinical adoption, there is still a need for more prehabilitation research.1,5–11 Notably, the clinical application of prehabilitation is seemingly outpacing the accumulation of scientific evidence for efficacy due to a combination of factors including that (1) prehabilitation does not typically involve medications or other interventions that are regulated by governmental organizations (e.g., registered clinical trials) and (2) it just makes sense to encourage people to adopt the healthy lifestyle components used in prehabilitation protocols (Fig. 2).
FIGURE 2.
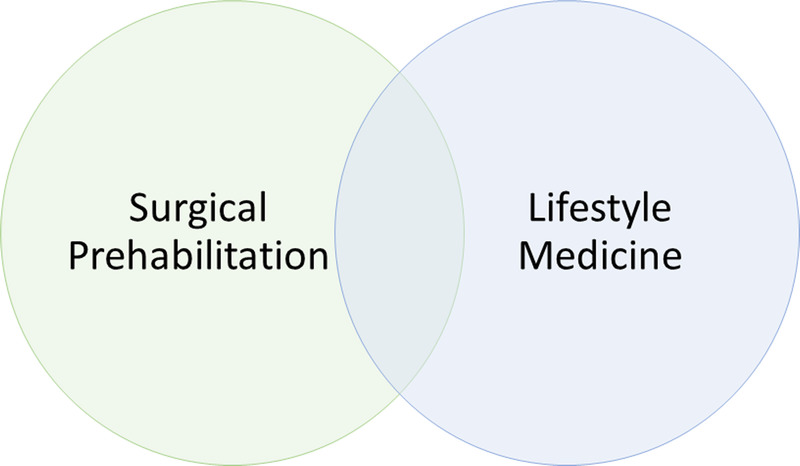
Similarities and differences between surgical prehabilitation and lifestyle medicine. Some elements of surgical prehabilitation and lifestyle medicine overlap, such as nutrition, exercise, stress resilience, and substance use/abuse intervention. However, each also has elements that are unique. For example, gratitude, journaling, and finding purpose are frequently part of lifestyle medicine but not surgical prehabilitation protocols. Similarly, targeted exercise for shoulder range of motion before breast cancer surgery or feeding tube placement education before gastrointestinal surgery would be part of surgical prehabilitation but not lifestyle medicine.
Much of the published research on prehabilitation has focused on a single modality—usually either exercise or nutrition—and these studies have generally shown benefit.12,13 For example, an elegant nutrition-only study conducted by Kabata et al.13 in a cohort of cancer patients who were not nutritionally deficient at screening revealed that a prehabilitation intervention including increased protein supplementation improved surgical outcomes. In this prospective randomized controlled trial, patients in the intervention group (n = 54) received two bottles of hypercaloric formula with 20 grams of protein in each bottle for 14 days before surgery while the control group (n = 48) ate their regular diet. Participants’ nutritional status was assessed twice—at qualification using weight loss in the previous 6 mos and laboratory parameters (albumin, total protein, transferrin, and total lymphocyte count) and 1 day before surgery using changes in body weight and laboratory parameters. After their surgeries, patients were followed for 30 days to assess postoperative complications. The researchers found that patients in the control group had a significantly higher number of serious complications compared with the intervention group. In addition, levels of all laboratory parameters declined significantly in the control group while remaining stable (albumin and total protein) or improving (transferrin and total lymphocyte count) in the intervention group.
Despite the benefits that a single modality may confer, there is a trend toward implementing multimodal prehabilitation as a combination of interventions may be superior.1,14,15 A systematic review and meta-analysis focused on outcomes in patients who underwent colorectal surgery included nine studies assessing the benefits of nutritional prehabilitation with and without exercise.12 This review revealed that nutritional prehabilitation alone or in combination with exercise significantly decreased hospital length of stay by 2 days. However, there was some evidence that multimodal prehabilitation accelerated the return to presurgical functional activity levels.
Individual research studies have also revealed that multimodal approaches have been used in surgical settings with considerable success. For example, perioperative early recovery programs, which generally include the 48–72 hrs before, during, and immediately after surgery, have been extensively studied and implemented.1 The multimodal approach of these programs is based on a concept often referred to as the “sum of small gains,” whereby each component on its own does not produce as much of an effect as the collection of interventions. Notably, prehabilitation, using single or multimodal interventions, complements or even augments early recovery programs and postoperative rehabilitation when incorporated into the treatment plan at least a couple of weeks before planned surgery (Fig. 3).
FIGURE 3.
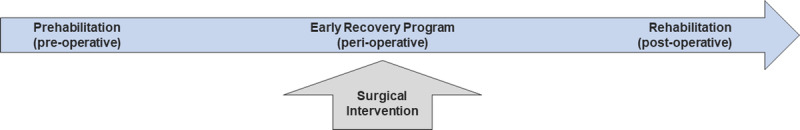
Combined surgical-rehabilitation care continuum. Surgical prehabilitation typically begins at least a couple of weeks before surgery. Early recovery programs are implemented during the perioperative period (48–72 hrs just before, during, and after surgery), which often include physical therapy referrals for early mobilization. Rehabilitation, when appropriate, is generally prescribed after surgery or at discharge from the acute care hospital.
PREHABILITATION AND COVID-19
Physiatrists should be aware that the concept of the sum of small gains that inform multimodal early recovery programs would likely hold for prehabilitation protocols; however, in clinical practice, there are important differences. Early recovery programs are perioperative and the multiple modalities are implemented in a controlled hospital setting for a short period (e.g., 48–72 hrs). In prehabilitation, the setting is less controlled and the timeframe is much longer. Therefore, if patients are given too much information or too many options, they may feel overwhelmed. In this confusing time during which patients awaiting surgery are likely already anxious, confused, and distracted, it is probably best to home in on a small set of prehabilitation interventions that are most likely to have the greatest benefit. The evidence base suggests that these would include exercise, nutritional supplementation with protein, glycemic control in patients with diabetes, smoking cessation, and psychological stress reduction (Fig. 4).
FIGURE 4.
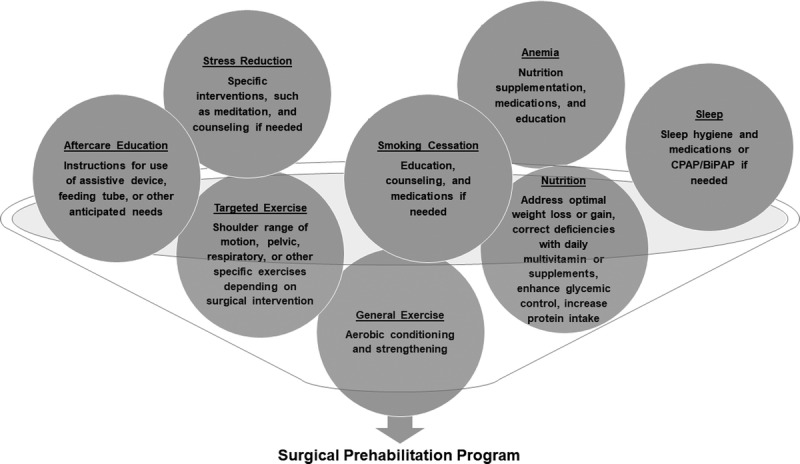
Common interventions in a surgical prehabilitation protocol. Surgical prehabilitation protocols may contain a variety of different interventions. Core elements that have been studied include general and targeted exercise, nutrition, psychological stress reduction, and smoking cessation. Other interventions that may be helpful include correcting anemia, treating obstructive sleep apnea, and providing aftercare education about common feeding tube problems, etc.
Rehabilitation professionals have deep knowledge of the myriad and profoundly deleterious health effects of bed rest, convalescence, and other reductions in physical activity levels.16 Notably, people who are symptomatic with COVID-19 infections may have a period of bed rest and convalescence even if they are not hospitalized. For those who are hospitalized and require mechanical ventilation or other interventions, bed rest and convalescence will likely be much longer and therefore deconditioning more profound. The literature demonstrates that healthy individuals who are on bed rest, even for a very short period, experience a myriad of deleterious physiologic effects.16 Loss of total skeletal muscle mass averages approximately 0.5%–6% daily, conservatively.16 Atrophy is more pronounced in the first few days and slows over time. People with advanced age tend to experience more loss. A decline in strength of approximately 1% per day is associated with muscle loss, although there is variability depending on the method of measurement.17
A similar pattern is seen regarding the cardiovascular effects of bed rest—with declines typically occurring quickly and then decreasing in rate over time. Studies suggest an approximate 1% per day decline in VO2max.16 Bed rest decreases blood volume, and because red cell mass does not decline at the same rate, people may have an increase in their blood viscosity leading to a propensity for thromboembolism. COVID-19 infection may also result in a hypercoagulable state associated with increased morbidity.18,19 One report found a 31% incidence of thrombotic complications in intensive care unit patients with COVID-19.19
Importantly, physiologic declines related to bed rest and convalescence that take days to occur, usually take far longer to revert back to baseline, and may only reach premorbid levels with rehabilitation. Moreover, the short- and long-term effects of COVID-19 infections are being actively studied and will have an important impact on the field of PM&R going forward. Without intervention, it is reasonable to theorize that the aftereffects of bed rest or convalescence will also increase individual surgeons’ and institutions’ complication rates (e.g., surgical site wound infections) and other metrics such as hospital length of stay and 30-day unanticipated readmissions. Theoretically, prehabilitation may be helpful in reducing morbidity and mortality in individuals who were infected with COVID-19, especially because it is known to have a predilection for cardiopulmonary sequelae.3,4,20 Moreover, the older people and those with comorbidities tend to be more severely affected. However, there is still much to learn about this virus, and it is clear that even young, healthy individuals may get severe infections. Therefore, encouraging people to maintain at least their minimum prepandemic baseline level of activity is worthwhile.20,21
In summary, clinical prehabilitation programs should (1) home in on the modalities that are most likely to prevent or reduce the incidence of known surgical complications in a particular population from a specific type of surgery (in accordance with the current published evidence); (2) align with surgical as well as rehabilitation outcome metrics; (3) take into account practical aspects of care delivered outside of the confines of a research protocol or controlled hospital setting so that patients are more likely to adhere to the most crucial recommendations for the appropriate length of time; and (4) not be confused with general lifestyle medicine recommendations, despite some overlap.
CONCLUSIONS
During and after the novel coronavirus pandemic, many surgeries will be delayed. Predictably, as the virus becomes less prevalent, there will be a tremendous motivation to move forward with scheduling operations from both patient care and institutional perspectives. Therefore, now is the time to consider wider adoption of prehabilitation for patients awaiting surgery. Even after the pandemic fades, the benefits of prehabilitation as part of the surgical care continuum should be evaluated as the current research suggests implementation may improve surgical outcomes in many populations. Certainly, there is always a need for more research to better understand which components and what doses may be most effective.
ACKNOWLEDGMENT
The author thank Julie A. Poorman, PhD, for her assistance with suggested edits and manuscript preparation.
Footnotes
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
REFERENCES
- 1.Carli F, Silver JK, Feldman LS, et al. : Surgical prehabilitation in patients with cancer: state-of-the-science and recommendations for future research from a panel of subject matter experts. Phys Med Rehabil Clin N Am 2017;28:49–64 [DOI] [PubMed] [Google Scholar]
- 2.Shinall MC, Jr., Arya S, Youk A, et al. : Association of preoperative patient frailty and operative stress with postoperative mortality. JAMA Surg 2019;e194620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Onder G, Rezza G, Brusaferro S: Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020. doi: 10.1001/jama.2020.4683. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Khan F, Amatya B: Medical rehabilitation in pandemics: towards a new perspective. J Rehabil Med 2020. doi: 10.2340/16501977-2676. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Prehabilitation, rehabilitation, and revocation in the army. Br Med J 1946;1:192–7 [PubMed] [Google Scholar]
- 6.Silver JK, Baima J, Mayer RS: Impairment-driven cancer rehabilitation: an essential component of quality care and survivorship. CA Cancer J Clin 2013;63:295–317 [DOI] [PubMed] [Google Scholar]
- 7.Silver JK, Baima J: Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am J Phys Med Rehabil 2013;92:715–27 [DOI] [PubMed] [Google Scholar]
- 8.Stout NL, Silver JK, Raj VS, et al. : Toward a national initiative in cancer rehabilitation: recommendations from a subject matter expert group. Arch Phys Med Rehabil 2016;97:2006–15 [DOI] [PubMed] [Google Scholar]
- 9.Li MH, Bolshinsky V, Ismail H, et al. : A cross-sectional survey of Australian anesthetists’ and surgeons’ perceptions of preoperative risk stratification and prehabilitation. Can J Anaesth 2019;66:388–405 [DOI] [PubMed] [Google Scholar]
- 10.Vasta S, Papalia R, Torre G, et al. : The influence of preoperative physical activity on postoperative outcomes of knee and hip arthroplasty surgery in the elderly: a systematic review. J Clin Med 2020;9:E969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santa Mina D, Brahmbhatt P, Lopez C, et al. : The case for prehabilitation prior to breast cancer treatment. PM R 2017;9(9S2):S305–16 [DOI] [PubMed] [Google Scholar]
- 12.Bolshinsky V, Li MH, Ismail H, et al. : Multimodal prehabilitation programs as a bundle of care in gastrointestinal cancer surgery: a systematic review. Dis Colon Rectum 2018;61:124–38 [DOI] [PubMed] [Google Scholar]
- 13.Kabata P, Jastrzebski T, Kakol M, et al. : Preoperative nutritional support in cancer patients with no clinical signs of malnutrition-prospective randomized controlled trial. Support Care Cancer 2015;23:365–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Minnella EM, Awasthi R, Gillis C, et al. : Patients with poor baseline walking capacity are most likely to improve their functional status with multimodal prehabilitation. Surgery 2016;160:1070–9 [DOI] [PubMed] [Google Scholar]
- 15.Gillis C, Buhler K, Bresee L, et al. : Effects of nutritional prehabilitation, with and without exercise, on outcomes of patients who undergo colorectal surgery: a systematic review and meta-analysis. Gastroenterology 2018;155:391–410 e394 [DOI] [PubMed] [Google Scholar]
- 16.Kortebein P: Physical inactivity: physiologic impairments and related clinical conditions, in: Frontera WR, DeLisa JA, Basford JR, et al.: (eds): Delisa’s Physical Medicine and Rehabilitation: Principles and Practice. Philadelphia, PA, Lippincott Williams & Wilkins, 2019 [Google Scholar]
- 17.Kilroe SP, Fulford J, Jackman SR, et al. : Temporal muscle-specific disuse atrophy during one week of leg immobilization. Med Sci Sports Exerc 2020;52:944–54 [DOI] [PubMed] [Google Scholar]
- 18.Wang H, Luo S, Shen Y, et al. : Multiple enzyme release, inflammation storm and hypercoagulability are prominent indicators for disease progression in COVID-19: a multi-centered, correlation study with CT imaging score. Lancet. Available at: https://ssrn.com/abstract=3544837. Published 2020. Accessed April 9, 2020 [Google Scholar]
- 19.Klok FA, Kruip MJHA, van der Meer NJM, et al. : Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020. doi: 10.1016/j.thromres.2020.04.013. [Epub ahead of print]. Available at: https://www.ncbi.nlm.nih.gov/pubmed/32291094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silver JK: Prehabilitation could save lives in a pandemic. Br Med J 2020;369:m1386. [DOI] [PubMed] [Google Scholar]
- 21.Silver JK, Tan E: Build strength during the coronavirus outbreak with ‘prehabilitation’. AARP. Available at: https://www.aarp.org/health/conditions-treatments/info-2020/prehab-during-coronavirus.html. Published 2020. Accessed April 9, 2020 [Google Scholar]


