Summary:
Telemedicine is an application of modern technology that allows for the remote delivery of healthcare services to diagnose and treat patients. The potential patient benefits of such a program include added convenience, lowered costs, and improved access. From a practical standpoint, establishing a telemedicine program may seem daunting to the plastic surgeon; success requires not only patient and provider adoption, but also integration of new technology. Despite these challenges, breast reconstruction patients are among those who stand to benefit most from telemedicine technology, as this patient population remains vulnerable to limitations to access following an emotion-provoking breast cancer diagnosis. Geographical limitation, especially in rural areas, represents a major barrier to access. To date, the application of telemedicine in caring for breast reconstruction patients has not been described in the literature. In this article, we describe the protocol developed and implemented by our academic plastic surgery group to care for new breast reconstruction candidates and discuss the role of telemedicine in improved access to breast reconstruction care.
INTRODUCTION TO TELEMEDICINE
Telemedicine is an application of modern technology that allows for the remote delivery of healthcare services to diagnose and treat patients. It has seen use in health screening, chronic disease management, and postoperative care.1–3 In plastic surgery, telemedicine usage has been described for veterans hospitals,4 rural areas, aesthetic practice, and academic demonstrations.1,4 Clinical applications have included skin lesions, carpal tunnel candidates, free flap monitoring, wound management, trauma, burns, and cleft lip/palate repair.1,4,5 Nevertheless, telemedicine has faced barriers to adoption, including reimbursement, medical licensure, confidentiality, and concerns regarding standard of care.6 Benefits include flexibility and ease of access with decreased travel time and cost. With the ever-increasing ownership of mobile technologies, telemedicine has the potential to become more geographically available, creating an opportunity for physicians to increase patient access to specialized healthcare in a cost-effective manner.5,7
THE NEED FOR AND ROLE OF TELEMEDICINE IN BREAST RECONSTRUCTION CARE
Despite implementation of the Women’s Health and Cancer Rights Act, up to 80% of women do not undergo reconstruction after breast cancer treatment.8 Patients without access to plastic surgery consultation are not adequately informed of potential reconstructive options. These include oncoplastic strategies during breast-conserving surgery, and total breast reconstruction, in immediate and delayed settings. The barriers to breast reconstruction remain multifactorial; they include rural location, financial burden, poor reimbursement, unfavorable physician attitudes regarding reconstruction in the setting of certain patient and tumor characteristics, and lack of patient awareness.9
Breast cancer care is multidisciplinary, and access to plastic surgeons remains paramount in allowing for shared decision-making regarding reconstruction. Research demonstrates that ablative surgeons with high referral propensity to plastic surgeons are more likely to be women, have high clinical breast volume, and work in cancer centers.8 Most cancer centers and high-volume ablative surgeons are located in dense population centers. A plastic surgery telemedicine consultation provides an opportunity to screen potential candidate patients for breast reconstruction, and provide them with subsequent options for care.
ESTABLISHING A TELEMEDICINE PLATFORM TO CARE FOR BREAST RECONSTRUCTION PATIENTS
Practice Integration
Our choice telemedicine platform, Zoom (San Jose, Calif.), is a cloud-based video and web conference technology that allows for secure communication among providers and patients. Its encrypted content and communications, including all transmitted protected health information, are managed in compliance with the Health Information Portability and Accountability Act, following the establishment of a business associate agreement with the protected health entity. Users, including all participating members of the practice, need to comply with the terms of the agreement and undergo appropriate training. Accessible using computer, tablet, and smartphone interfaces, the platform requires a subscription fee with varying levels of support and storage capacity depending upon the scale of the enterprise. The application also has capacity for integration into prevalent electronic medical record (EMR) systems.
In addition to staff training, the office should establish a sound-insulated, well-lit, dedicated space for videoconferencing sessions. A neutral background that notes the affiliated healthcare center is helpful to eliminate distractors. A 30-minute consultation slot is typically scheduled.
Patient Recruitment and Preconsultation Preparation
Breast surgeons from affiliated or geographically amenable settings must be knowledgeable about the service. A packet with necessary documents should be made available to newly diagnosed patients at the ablative surgeon’s office. These should include basic patient education on breast reconstruction, an assessment questionnaire that includes the standard medical history questions as well as targeted questions such as history of abdominal, back and/or breast surgery, and confidentiality agreements and other legal documentation necessary to participate in telemedical care. All such records should be uploaded to the EMR before the encounter.
Patient Consultation
Once patients are deemed appropriate candidates, they can participate in an initial consultation video conference with the plastic surgeon. A telemedicine encounter consists of the sequential steps as depicted in Figure 1.10 Should the patient choose to proceed surgically, a coordinated, in-person meeting with all involved specialties including breast surgery, plastic surgery, and anesthesia is scheduled. Postoperative follow-up may also be facilitated via telemedicine, as it is more commonly described in the literature (Fig. 1).
Fig. 1.
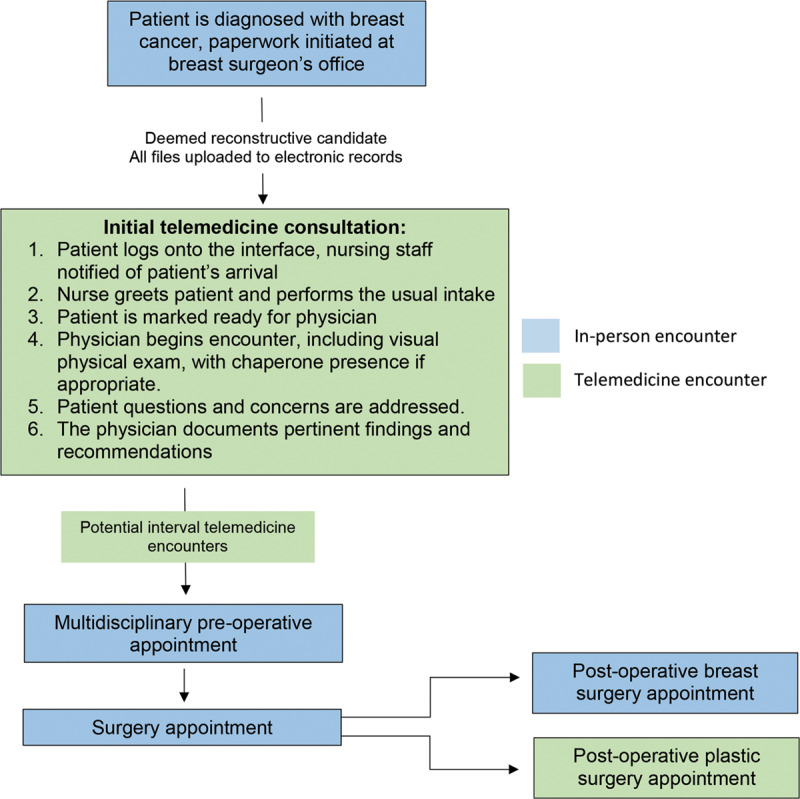
Teleconsultation model for breast reconstruction patients.
Special Considerations and Future Directions
As telemedicine continues to evolve, practices need to consider medicolegal ramifications. The ability to conduct cross-state consultation varies given heterogenous medical licensing governance. Recent legislative efforts have attempted to reduce the geographic barriers to cross-state telemedicine, including the TELE-MED Act (2013), Telehealth Promotion Act (2015), and VETS Act (2017). Most significantly, the Interstate Medical Licensure Compact now provides an expedited pathway to licensure for qualified physicians to practice in multiple participating states. To date, 29 states have entered or passed the associated legislation and have either completed or are in the process of implementation. Clarification of specific state regulations should be made with the appropriate medical licensure board.
Similarly, implications of telemedicine consultation and associated liability need to be discussed with individual malpractice insurance carriers to ensure compliance. Appropriate consents and waivers should be generated after consultation with legal counsel. Patients should be made aware of the limitations of videoconference consultation, as telemedicine interactions do not allow for the same tactile feedback of examining a patient and better understanding their particular tissue quality. Thus, final treatment plans may change pending in-person evaluation. Although all audio, video, and screen sharing data are protected and encrypted, there is always the risk of accidental or malicious breaches. Individual state regulations should be verified.
Given the resource requirements for establishment of telemedicine, reimbursement is a pertinent issue that remains variable due to differing payor policies and state law. Although Medicare provides reimbursement for patients from underserved areas, beneficiaries are required to present to designated originating sites for a qualifying telemedicine encounter.8 Heterogenous coverage policies exist among private carriers. Comprehensive discussion of state regulations surrounding telehealth reimbursement exceeds the scope of this article, but the Center for Connected Health Policy (https://www.cchpca.org) is an excellent resource for up-to-date state legislation, regulation, and policy on these issues.
CONCLUSIONS
Telemedicine provides a key avenue for overcoming access barriers that are well recognized in breast cancer reconstruction, especially in underserved and rural areas. Although logistical and medicolegal challenges remain, plastic surgeons should recognize the potential of telemedicine in improving delivery of quality care and actively adopt this technology, especially as state/professional regulatory bodies have recently demonstrated commitment to growth of the telehealth arena.
Footnotes
Published online 19 March 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Due to the nature of the research project, which does not include any patient photographs or identifiable information, no IRB approval was required.
REFERENCES
- 1.Vyas KS, Hambrick HR, Shakir A, et al. A systematic review of the use of telemedicine in plastic and reconstructive surgery and dermatology. Ann Plast Surg. 2017;78:736–768. 10.1097/SAP.0000000000001044 [DOI] [PubMed] [Google Scholar]
- 2.Chasan JE, Delaune B, Maa AY, et al. Effect of a teleretinal screening program on eye care use and resources. JAMA Ophthalmol. 2014;132:1045–1051. 10.1001/jamaophthalmol.2014.1051 [DOI] [PubMed] [Google Scholar]
- 3.Flodgren G, Rachas A, Farmer AJ, et al. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015CD002098 10.1002/14651858.CD002098.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Douglas S, Geiger E, McGregor A, et al. Telehealth in plastic surgery: a Veterans Affairs hospital perspective. Plast Reconstr Surg Glob Open. 2018;6:e1840 10.1097/GOX.0000000000001840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gardiner S, Hartzell TL. Telemedicine and plastic surgery: a review of its applications, limitations and legal pitfalls. J Plast Reconstr Aesthet Surg. 2012;65:e47–e53. 10.1016/j.bjps.2011.11.048 [DOI] [PubMed] [Google Scholar]
- 6.Lee B. Mercer National Health Survey: Employers finding new ways to hold the line on health benefit cost growth. 2017. Mount Laurel, N.J.: Marsh & McLennan Companies; Available at https://www.mercer.com/newsroom/mercer-national-health-survey-employers-finding-new-ways-to-hold-the-line-on-health-benefit-cost-growth.html. Accessed June 21, 2019. [Google Scholar]
- 7.Perednia DA, Allen A. Telemedicine technology and clinical applications. JAMA. 1995;273:483–488. [PubMed] [Google Scholar]
- 8.Alderman AK, Hawley ST, Waljee J, et al. Correlates of referral practices of general surgeons to plastic surgeons for mastectomy reconstruction. Cancer. 2007;109:1715–1720. 10.1002/cncr.22598 [DOI] [PubMed] [Google Scholar]
- 9.Retrouvey H, Solaja O, Gagliardi AR, et al. Barriers of access to breast reconstruction: a systematic review. Plast Recon Surg. 2018;143:465e–476e. 10.1097/PRS.0000000000005313 [DOI] [PubMed] [Google Scholar]
- 10.Jalalabadi F, Izaddoost SA, Guillen DE, et al. Deploying your telehealth platform. Semin Plast Surg. 2018;32:172–175. 10.1055/s-0038-167215 [DOI] [PMC free article] [PubMed] [Google Scholar]


