Supplemental Digital Content is available in the text.
Background:
Pediatric hand fractures are common and approximately 10% require surgery.
Methods:
This retrospective cohort study reports on hand fractures in a large pediatric population and identifies the characteristics and patterns of fractures that required surgical correction. A χ2 analysis was done to evaluate the association between individual fracture variables and surgery. The STROBE checklist was applied.
Results:
One thousand one-hundred seventy-three hand fractures were reviewed. Peak age was 16 years for boys and 14 years for girls. Most fractures were closed (96.0%) and nonrotated (91.3%), and had no concomitant soft tissue injury (72.7%). More than half (56.3%) were nonepiphyseal plate fractures; yet as a single diagnosis, Salter–Harris II fractures were most common (30.2%). The following variables were significantly associated with surgery: open fractures, rotational deformity, distal phalangeal fracture location, multiple fractures, oblique pattern, comminution, displacement >2 mm, intra-articular involvement, and angulation >15°. Most fractures required only immobilization and early range of motion (64.3%). Closed reduction was required in 22.7%. Minor surgery by the primary provider was performed in 3.2% of fractures. Surgery by a hand surgeon was performed in 9.8%. The most common patterns requiring surgery were proximal or middle phalanx head or neck fractures (38.2%) and metacarpal midshaft fractures (20.9%). The most common operation was open reduction internal fixation (52.2%).
Conclusions:
Pediatric hand fractures are common, but 90.2% do not require surgery and, as such, primary providers play a key role in management. Certain fracture variables and patterns are more likely to lead to surgery.
INTRODUCTION
Hand fractures are common pediatric injuries,1–7 but there are relatively few studies on their epidemiology.1,2,4–14 Although most do well with immobilization alone, there is a subset of approximately 10%4–9,15–17 that require surgical intervention. It is common to describe a fracture by physical examination findings (eg, rotated or nonrotated) or radiographic findings (eg, angulation on anterior–posterior radiograph of 20°), but it is rare that surgical treatment is dictated by any one individual finding. The purpose of this study is to report on hand fractures in a large pediatric cohort of patients, which were managed either nonsurgically or surgically, and to identify the characteristics and patterns of fractures that required surgical correction.
METHODS
The National Ambulatory Care Reporting System (NACRS) was used to determine the total number of pediatric hand fractures in the Calgary Zone from January 2013 to December 2014 (a 2-year period). NACRS contains all data for hospital-based and community-based ambulatory care and includes day surgery, outpatient and community-based clinics, and emergency departments in Alberta, Canada. Pediatric hand fractures (occurring in patients 17 years and younger) were identified using International Statistical Classification of Disease and Related Health Problems version 10 (ICD-10) codes S62.2 to S62.7 (representing fractures of the metacarpals or phalanges).
A retrospective cohort of consecutive pediatric patients referred with hand fractures to the Alberta Children’s Hospital (ACH) hand clinic over this 2-year period was also identified; this cohort was, therefore, a subset of all pediatric hand fractures in the Calgary zone. The ACH is a tertiary pediatric center that serves the city of Calgary as well as southern Alberta and cares for over 90,000 children per year. Five pediatric plastic surgeons, all hand surgeons, manage the pediatric hand fracture referrals to the center. Patients were identified using the Clinibase Regional Scheduler software (Logibec, Montreal, QC). The medical records (both electronic and paper) of any patient with a diagnosis of a hand injury were reviewed and those with a radiographically confirmed hand fracture were included in the present study. Patients were excluded if they had a soft tissue injury without an accompanying hand fracture or had incomplete chart information. Complete amputations were excluded. Partial amputations were included and recorded as open fractures.
Data were collected and recorded for the following variables: patient demographics (age at time of injury, gender, and mechanism of injury), physical findings (closed or open injury, rotational deformity, and concomitant soft tissue injury), radiologic findings, and fracture management. No blinding procedures were performed. Age was categorized into 3 groups to reflect clinically relevant school ages. Open injuries were defined as soft tissue breakdown with exposure of the bone fracture. Radiographs (initial and postreduction) for all patients were reviewed on the hospital’s picture archiving and communication system, AGFA Impax 6 (AGFA HealthCare NV, 2009, Belgium). Fracture management, both by the referring physician and the hand surgeon, was recorded. Surgery was defined as any procedure done under general anesthetic, including closed reduction, Kirshner wire fixation, and internal fixation with plates and screws. Internal fixation performed under any other anesthesia was also considered surgery (eg, Kirshner wire fixation in an older child performed under local anesthesia). Notably, closed reduction under local anesthetic was not classified as surgery. Fracture outcomes were recorded up until the time of data collection (June 1, 2017). The data collection was not blinded.
χ2 analyses were performed to investigate the association between individual variables and the outcome “surgery,” with a P value <0.05 considered statistically significant. Missing data were handled with pairwise deletion. The Strengthening the Reporting of Observational Studies in Epidemiology statement was followed18 (see appendix, Supplemental Digital Content 1, which displays STROBE statement—checklist of items that should be included in reports of cohort studies, http://links.lww.com/PRSGO/B357). Further subgroup analysis of the fractures that required surgery was performed to identify specific patterns.
RESULTS
All Fractures
The total number of pediatric hand fractures for the years 2013–2014 was 2,783: of these, 2,162 were in the city of Calgary and 621 were in the surrounding, major referral centers (the cities of Airdrie, Cochrane, Okotoks, and Strathmore). Of this total, 1,410 hand fractures were referred to ACH hand surgeons, of which 230 were soft tissue injuries without concomitant fractures and were subsequently excluded. Another 7 fractures were excluded because of incomplete chart information (4 patients had no detailed electronic or paper medical record of the visit) or inaccessible radiographs. Thus, there were 1,173 fractures in 1,043 patients (Fig. 1). Therefore, the proportion of pediatric hand fractures referred in the Calgary Zone to the ACH hand surgeons, and reviewed in this study, was 42.1% (1,173/2,783).
Fig. 1.

Patient flow diagram and hand fracture management.
Of the referred hand fractures (n = 1,173), 92.5% occurred in children over the age of 5 (Table 1). Boys outnumbered girls in almost all age groups. The distribution was unimodal with a peak at 16 years for boys and 14 years for girls. Both distributions were skewed to the right, meaning there were a higher proportion of older children referred with hand fractures. The most common recorded mechanism of injury was participation in ball games (34.6%). Physical findings, location of the fracture, and radiologic findings are described in Table 1. There were 794 phalangeal fractures (67.7%) and 379 metacarpal fractures (32.3%). Most fractures were closed (96.0%) and nonrotated (91.3%), and had no concomitant soft tissue injury (72.7%). The most common fracture locations were the finger proximal phalanges (29.1%). Radiologically, 43.7% of fractures involved the growth plate: Salter Harris II fractures were the most common overall (30.2%). Salter–Harris III fractures accounted for 9.2% of all fractures; Salter–Harris I, IV, and V fractures combined, on the other hand, accounted for less than 5% of all fractures. Nonepiphyseal fractures were more common (56.3%), and the majority were described as transverse or oblique/spiral (20.9% and 19.5%, respectively). Condylar fractures, those that involve the articulating, rounded head of a phalangeal joint, were seen in 6.1% of cases. Only 3.0% of fractures were comminuted. More than one-half of the fractures were displaced at least 2 mm on radiograph (57.6%) and approximately one-quarter of the fractures were intra-articular (23.2%). Included in the category “intra-articular” were volar plate avulsion fractures which made up a large percentage of this description. About one-fifth of fractures displayed greater than 15° of angulation on at least one radiographic view (21.9%).
Table 1.
Fracture Characteristics
| Variable | Total (N = 1,173) | Required Surgery (N = 115) | P | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Demographics | |||||
| Age | |||||
| Preschool (0–5 y) | 88 | 7.5 | 10 | 8.7 | |
| Primary school (6–11 y) | 351 | 29.9 | 18 | 15.7 | |
| Secondary school (12–18 y) | 734 | 62.6 | 87 | 75.7 | |
| Gender | |||||
| Male | 822 | 70.1 | 88 | 76.5 | |
| Side of hand injured | |||||
| Right | 538 | 45.7 | 63 | 54.8 | |
| Mechanism of injury | |||||
| Ball games | 406 | 34.6 | 32 | 27.8 | |
| Fall | 202 | 17.2 | 13 | 11.3 | |
| Punch | 132 | 11.3 | 12 | 10.4 | |
| Winter sport | 107 | 9.1 | 12 | 10.4 | |
| Crush | 106 | 9.0 | 18 | 15.7 | |
| Other | 203 | 17.3 | 26 | 22.6 | |
| Missing | 17 | 1.5 | 2 | 1.7 | |
| Physical findings | |||||
| Open | 47 | 4.0 | 26 | 22.6 | <0.001 |
| Malrotation | 102 | 8.7 | 32 | 27.8 | <0.001 |
| Concomitant soft tissue injury | |||||
| None | 853 | 72.7 | 70 | 60.9 | |
| Ligament | 107 | 9.1 | 6 | 5.2 | 0.1 |
| Tendon | 59 | 5.0 | 9 | 7.8 | 0.1 |
| Nail bed | 37 | 3.2 | 3 | 2.6 | 0.4 |
| Dislocation/subluxation | 33 | 2.8 | 6 | 5.2 | 0.1 |
| Laceration | 19 | 1.6 | 4 | 3.5 | 0.07 |
| Missing | 65 | 5.5 | 3 | 2.6 | |
| Location | |||||
| Thumb metacarpal | 81 | 6.9 | 9 | 7.8 | 0.7 |
| Finger metacarpals | 298 | 25.4 | 25 | 21.7 | 0.3 |
| Thumb proximal phalanx | 127 | 10.8 | 7 | 0.6 | 0.09 |
| Finger proximal phalanges | 341 | 29.1 | 39 | 33.9 | 0.2 |
| Finger middle phalanges | 169 | 14.4 | 12 | 10.4 | 0.2 |
| Digit distal phalanges | 157 | 13.4 | 23 | 20.0 | 0.03 |
| Multiple fractures | 167 | 14.2 | 24 | 20.9 | 0.04 |
| Radiographic characteristics | |||||
| Epiphyseal | |||||
| Salter–Harris I | 24 | 2.0 | 0 | 0 | 0.1 |
| Salter–Harris II | 346 | 29.5 | 6 | 5.2 | <0.001* |
| Salter–Harris III | 117 | 10.0 | 6 | 5.2 | 0.07 |
| Salter–Harris IV | 21 | 1.8 | 1 | 0.9 | 0.4 |
| Salter–Harris V | 5 | 0.4 | 1 | 0.9 | 0.4 |
| Nonepiphyseal (more than one descriptor per fracture possible) | |||||
| Transverse | 245 | 20.9 | 32 | 27.8 | 0.09 |
| Oblique/spiral | 228 | 19.4 | 45 | 39.1 | <0.001 |
| Avulsion | 107 | 9.1 | 8 | 7.0 | 0.4 |
| Tuft | 45 | 3.8 | 6 | 5.2 | 0.4 |
| Comminuted | 35 | 3.0 | 11 | 9.6 | <0.001 |
| Intraarticular | 272 | 23.2 | 51 | 44.3 | <0.001 |
| Condylar | 72 | 6.1 | 33 | 28.7 | <0.001 |
| Displacement | 676 | 57.6 | 77 | 70.0 | <0.001 |
| Angulation >15° on x-ray | 257 | 21.9 | 47 | 40.9 | <0.001 |
| Angulation >15° on AP x-ray | 141 | 12.0 | 21 | 18.3 | 0.031 |
| Angulation >15° on lateral x-ray | 193 | 16.5 | 38 | 33.0 | <0.001 |
*Significant for a decreased risk of surgery.
Values in boldface are statistically significant.
Fractures Requiring Surgery
Fracture characteristics, detectable on either the physical examination or x-ray, that were associated with a statistically significant increased risk for needing surgery were open fractures, rotated fractures, fractures of the distal phalanges, multiple fractures, oblique or spiral fracture patterns, comminution, displacement, intra-articular involvement, condylar involvement, and angulation greater than 15 degrees on radiograph (Table 1).
Aside from the individual general fracture characteristics listed above, certain fracture patterns were found to be more likely to need surgical intervention (Table 2; Fig. 2). In general, 81/794 (10.2%) phalangeal and 34/379 (9.0%) metacarpal fractures required surgery. Among phalangeal fractures, those most likely to require surgery were head and neck fractures of the proximal and middle phalanges (33.6% required surgery, accounting for 38.2% of all operative cases) and fractures of the middle part of the proximal or middle phalanx (20.7% required surgery, accounting for 5.2% of operative cases). Only 3.2% (18/562) of fractures of the base of the phalanx required surgery; yet this location still accounts for 15.7% (18/115) of all pediatric hand fractures requiring surgery, mainly because this fracture location is so common (562/1,173 of all fractures). These fractures included large avulsion fragments involving the distal phalanx (mallet deformity) or proximal phalanx of the thumb in the vicinity of the insertion of the metacarpophalangeal joint ulnar collateral ligament. Included in this location are the Salter–Harris II and III epiphyseal fractures, which were very common overall, but few required surgery (12/463, 2.6%). Crush injuries of the distal phalanx, most common in very young children and usually related to the tip of the digits being crushed in a door frame, required surgical intervention in 20.3% of cases (accounting for 11.3% of all operative cases). These injuries were often open and required minor debridement and repair of the nail bed.
Table 2.
Clinically Relevant Fracture Patterns of Fractures Requiring Surgery
| Fracture Pattern | No. Fractures (N = 1,173) | No. Fractures Requiring Surgery (%) | Percentage of All Fractures Requiring Surgery (N = 115) |
|---|---|---|---|
| Phalangeal | 794 | 81 (10.2) | (70.4) |
| Head* and neck† of proximal and middle phalanges | 131 | 44 (33.6) | (38.2) |
| Base of any phalanx‡ | 562 | 18 (3.2) | (15.7) |
| Distal phalanx crush (including nail bed repair) | 64 | 13 (20.3) | (11.3) |
| Middle part of proximal or middle phalanx | 29 | 6 (20.7) | (5.2) |
| Metacarpal | 379 | 34 (9.0) | (29.6) |
| Midshaft of metacarpal | 92 | 19 (20.7) | (16.5) |
| Base of metacarpal§ | 137 | 13 (9.5) | (11.3) |
| Distal metacarpal | 150 | 2 (1.3) | (1.7) |
*Head of phalanx was defined as unicondylar or bicondylar fractures.
†Neck of phalanx fractures included transverse or oblique fractures.
‡Included fracture dislocations, bony mallet fractures, bony UCL thumb fractures, Seymour fractures, and other Salter–Harris II fractures.
§Included Bennet’s fracture, Baby Bennet’s fractures, and non-Bennet’s base of first metacarpal fracture.
UCL, ulnar collateral ligament.
Fig. 2.
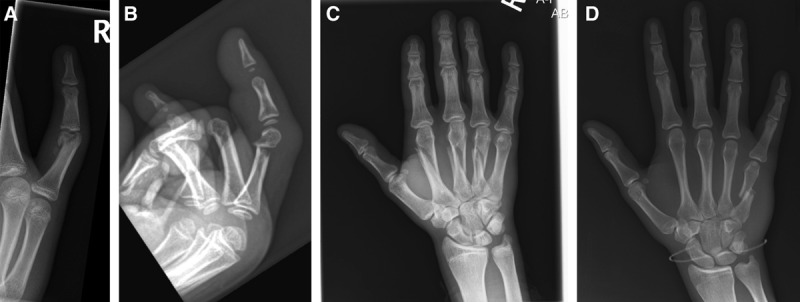
Example radiographs of common surgical fractures. A, Unicondylar proximal phalanx fracture. B, Proximal phalangeal neck fracture. C, Multiple oblique midshaft metacarpal fractures. D, Transverse midshaft metacarpal fracture.
For metacarpal fractures, two patterns were associated with an increased need for surgical intervention. First, 20.7% of midshaft fractures, either an oblique or transverse, required operative fixation (accounting for 16.5% of all operative cases). Second, 9.5% of fractures of the metacarpal base required surgical intervention (accounting for 11.3% of operative cases); these fractures most commonly involved the first metacarpal (Bennet’s or non-Bennet’s fracture at the base of first metacarpal) or the fifth metacarpal (baby Bennet’s fracture). Fractures of the neck of the metacarpal (ie, Boxer’s fractures) were the least likely to require surgery (1.3% required surgery, accounting for 1.7% of operative cases).
Fracture Management by Referring Physicians
Fracture management is summarized in Table 3. The most common initial management by a referring physician was immobilization alone (included buddy taping, splinting or casting) (69.3%). Approximately, one-fifth of fractures received a closed reduction (21.8%). The proportion of attempted closed reductions done by primary providers that were successful was 84.7%, where success was defined as only requiring further evaluation and immobilization by a hand surgeon. Of the 39 unsuccessful attempts, 13 required repeat closed reduction and 26 went on to require surgery. Of the 255 fractures that had a closed reduction by the primary provider, the most common type of fracture was Salter–Harris II fracture (120/255) and was successful 86.7% (104/120) of the time. The second most common type of fracture reduced was a transverse fracture of the neck of either the fourth or fifth metacarpals (66/255), and was successful 81.8% (54/66) of the time. Minor surgery by a primary care physician was performed in 45 fractures (3.8% of all fractures); these were crush injuries of the fingertip (distal phalanx) and minor surgery involved combinations of debridement, nail bed repair, and reduction of the fracture. This minor surgery was successful 82.2% of the time with only 8 patients requiring repeat surgery by the hand surgeon.
Table 3.
Management of Pediatric Hand Fractures
| Management | Total (%) N = 1,173 | Subsequently Required Surgery (N = 115) |
|---|---|---|
| By referring physician | ||
| Evaluation only | 60 (5.1) | 14 |
| Immobilization | 813 (69.3) | 67 |
| Closed reduction and immobilization | 255 (21.8) | 26 |
| Minor surgery ± immobilization | 45 (3.8) | 8 |
| By hand surgeon | ||
| Evaluation ± range of motion | 34 (2.9) | |
| Immobilization ± range of motion | 973 (82.9) | |
| Repeat closed reduction and immobilization | 13 (1.1) | |
| Initial closed reduction and immobilization | 38 (3.2) | |
| Surgery and immobilization | 115 (9.8) | |
| Surgical details | N = 115 | |
| Anesthesia | ||
| General anesthesia, conscious sedation or regional block | 102 (88.7) | |
| Local anesthesia | 13 (11.3) | |
| Surgical procedures | ||
| Open reduction, debridement, no internal fixation required. | 16 (13.9) | |
| Closed reduction internal fixation | 39 (33.9) | |
| Open reduction internal fixation | 60 (52.2) | |
Fracture Management by Hand Surgeons
The most common management after assessment by a hand surgeon was immobilization alone, followed eventually by range of motion exercises (973/1,173 fractures, 82.9%). Specific range of motion protocols varied by the surgeon and type of fracture, and the data were not available for analysis. This number included the 216 patients who previously had a closed reduction performed by the primary care provider (18.4% of all fractures). Hand surgeons performed 51 closed reductions (4.3% of all referred fractures) in the clinic; of these, 37 were first-time closed reductions (3.2% of all referred fractures) and 13 were repeat closed reductions (1.1% of all referred fractures).
Surgery was performed in 115/1173 (9.8%) fractures. Of these, 102 were done with an anesthesiologist present: 100 under general anesthetic, 1 with conscious sedation, and 1 with regional axillary block. The remaining 13 procedures were performed under local anesthetic, without the presence of an anesthesiologist. The most common operation was open reduction, internal fixation with either miniplate(s), lag screws or K-wires (52.2%), followed by closed reduction and internal fixation with K-wires (33.9%), and open reduction and debridement without internal fixation (13.9%).
Summarizing the ultimate treatment of all the fractures, 64.3% was managed with immobilization only followed by early range of motion programs; 22.7% was managed with closed reduction, immobilization, and eventually range of motion programs; 3.2% underwent successful minor surgery by a primary care provider and 9.8% required surgery by the hand surgeon.
DISCUSSION
This study reports on the epidemiology of pediatric hand fractures using a large Canadian sample. The findings confirm and extend observations from other studies in first world countries. Most fractures occurred in males, and fracture rates peaked later in males than females.1–3,7,9,14,19 Nonepiphyseal fractures were slightly more common (56.3%) than those involving the growth plate. As a single entity, Salter–Harris II fractures were the most common fracture.5,7,19 Most of the observed fracture characteristics were similar to the literature: they were closed (96.0%) and nonrotated (91.3%), and had no concomitant soft tissue injury (72.7%). However, over half of the observed fractures in this study were displaced which is higher than previously reported,2,7,9 possibly due to the relatively broad definition of displacement (>2 mm). Approximately, one-fourth of fractures were intra-articular (23.2%), which is higher than the rates of 5%–17% reported by others.6,7 This study included avulsion fractures (n = 107) as intra-articular fractures which may account for this increased proportion. Despite the higher number of fractures that were displaced or intra-articular in this study, the majority of fractures remain nonoperative and can be managed with immobilization alone, which is consistent with the literature.2,4,5,7,8,15,17
The authors of this study have previously performed a scoping review of the literature looking at primary care physicians’ referring practices for pediatric hand fractures and found a considerable variation in reported referral rates..20 In particular, primary care physicians reported referring rates to hand surgeons of 6.5%–82.6%8,21–23 and hand surgeons reported referring rates from primary care physicians of 35%–100%.4,7,14,24–26 In this current study, the proportion of pediatric hand fractures referred by primary care providers at its major referral centers to the ACH hand surgeons was 42.1%.
An important finding from this study was the role that primary providers play in the management of pediatric hand fractures. It was worthwhile for primary care providers to treat hand fractures with closed reduction or minor surgery when indicated. Fractures displaced >2 mm or angulated >15 degrees were successfully reduced by the primary provider 84.7% of the time. This accounted for 18.4% of all fractures and these were mainly Salter–Harris II fractures of the proximal phalanx and Boxer’s fractures of the fourth and fifth metacarpals. Also, primary care providers were successful with their minor surgical procedures 82.2% of the time in distal phalanx fractures with nail bed injuries. Of course, it is still worthwhile for fractures that have been reduced to be evaluated by hand specialists to ensure proper reduction: 5.1% required repeat reduction and 10.2% required surgery.
This study also highlights for primary providers that certain variables were more likely to lead to surgery, and thereby, should necessitate a referral to a hand surgeon. Clinical and radiologic characteristics found in this study to statistically predict for the need for surgery and which are also corroborated in the literature include open fractures,4,5,8,27 rotation deformity,4,5 distal phalanx fractures with nail bed laceration,8 multiple fractures, oblique or spiral fractures, comminution,4 displacement,4,8,27 intraarticular involvement,4,26,27 condylar involvement,26,28 and significant angulation.15
Although identification of individual fracture characteristics may make the description of fractures by primary care providers more complete, there are certain patterns of fractures that are recognized by the hand surgeon as at higher risk for needing surgery or at least in need of close follow-up. In many cases, it is not the specific fracture characteristic that is important to the hand surgeon but rather the fracture pattern. For example, the characteristic “intraarticular” can refer to both a small minimally displaced volar avulsion fragment from the base of the middle phalanx with no loss of joint stability (not in need of surgical intervention), and to unicondylar or bicondylar proximal phalangeal fractures also involving the proximal interphalangeal joint (requiring close follow-up and in many cases surgery). It would be useful to develop tools which would allow primary care providers to determine which pediatric hand fractures need to be referred to hand surgeons.
Limitations of this study include the retrospective study design. Also, because this is a referred population, the hand fractures in this study may be more severe than all-comer hand fractures. In addition, fracture management was reported, but outcomes were not available for reporting.
In conclusion, although pediatric hand fractures are very common, approximately 90% do not require surgical intervention, and conversely the primary provider can potentially play a key role in the management of this nonsurgical group. Certain fracture variables and specific fracture patterns can potentially predict which fractures are in need of either surgery or close observation by a hand surgeon. Future efforts in this area will focus on the development and validation of a prediction rule to aid primary care providers in management decisions, including identification of the subset of children who should be referred to a hand surgeon.
ACKNOWLEDGMENTS
This project was approved by the University of Calgary Conjoint Health Research Ethics Boards (REB14-1846). Dr Hartley had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors meet ICMJE authorship criteria. R.H., C.T.-O., A.R.H., and F.O.G.F. were involved in concept, design, and critical revision of the manuscript for important intellectual content. R.H., J.L., C.K., K.H., C.T.-O., A.R.H., and F.O.G.F. were involved in acquisition, analysis, or interpretation of data. R.H., J.L., A.R.H., and F.O.G.F. were involved in drafting the manuscript. R.H. and F.O.G.F. were involved in statistical analysis.
Supplementary Material
Footnotes
Published online 24 March 2020.
Preliminary results from this work were presented at the American Association for Hand Surgery Annual Meeting in 2017.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Cooper C, Dennison EM, Leufkens HG, et al. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res. 2004;19:1976–1981. [DOI] [PubMed] [Google Scholar]
- 2.Hastings H, II, Simmons BP. Hand fractures in children. Clin Orthop Relat Res. 1984;188:120–130. [PubMed] [Google Scholar]
- 3.Landin LA. Fracture patterns in children. Acta Orthopaedica Scandinavica. 198354suppl 2023–109. [PubMed] [Google Scholar]
- 4.Liu EH, Alqahtani S, Alsaaran RN, et al. A prospective study of pediatric hand fractures and review of the literature. Pediatr Emerg Care. 2014;30:299–304. [DOI] [PubMed] [Google Scholar]
- 5.Mahabir RC, Kazemi AR, Cannon WG, et al. Pediatric hand fractures: a review. Pediatr Emerg Care. 2001;17:153–156. [DOI] [PubMed] [Google Scholar]
- 6.Stanton JS, Dias JJ, Burke FD. Fractures of the tubular bones of the hand. J Hand Surg Eur Vol. 2007;32:626–636. [DOI] [PubMed] [Google Scholar]
- 7.Young K, Greenwood A, MacQuillan A, et al. Paediatric hand fractures. J Hand Surg Eur Vol. 2013;38:898–902. [DOI] [PubMed] [Google Scholar]
- 8.Bhende MS, Dandrea LA, Davis HW. Hand injuries in children presenting to a pediatric emergency department. Ann Emerg Med. 1993;22:1519–1523. [DOI] [PubMed] [Google Scholar]
- 9.Worlock PH, Stower J. The incidence and pattern of hand fractures in children. J Hand Surg. 1985198–200. [DOI] [PubMed] [Google Scholar]
- 10.Al-Jasser FS, Mandil AM, Al-Nafissi AM, et al. Epidemiology of pediatric hand fractures presenting to a university hospital in central Saudi Arabia. Saudi Med J. 2015;36:587–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fetter-Zarzeka A, Joseph MM. Hand and fingertip injuries in children. Pediatr Emerg Care. 2002;18:341–345. [DOI] [PubMed] [Google Scholar]
- 12.Mirdad T. Pattern of hand injuries in children and adolescents in a teaching hospital in Abha, Saudi Arabia. J R Soc Promot Health. 2001;121:47–49. [DOI] [PubMed] [Google Scholar]
- 13.Rajesh A, Basu AK, Vaidhyanath R, et al. Hand fractures: a study of their site and type in childhood. Clin Radiol. 2001;56:667–669. [DOI] [PubMed] [Google Scholar]
- 14.Vadivelu R, Dias JJ, Burke FD, et al. Hand injuries in children: a prospective study. J Pediatr Orthop. 2006;26:29–35. [DOI] [PubMed] [Google Scholar]
- 15.Leonard MH, Dubravcik P. Management of fractured fingers in the child. Clin Orthop Relat Res. 1970;73:160–168. [PubMed] [Google Scholar]
- 16.Lindley SG, Rulewicz G. Hand fractures and dislocations in the developing skeleton. Hand Clin. 2006;22:253–268. [DOI] [PubMed] [Google Scholar]
- 17.Valencia JS, Leyva F, Gomez-Bajo GJ. Pediatric hand trauma. Clin Orthop Relat Res. 200577–86. [DOI] [PubMed] [Google Scholar]
- 18.von Elm E, Altman DG, Egger M, et al. ; STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. [DOI] [PubMed] [Google Scholar]
- 19.Chew EM, Chong AK. Hand fractures in children: epidemiology and misdiagnosis in a tertiary referral hospital. J Hand Surg Am. 2012;37:1684–1688. [DOI] [PubMed] [Google Scholar]
- 20.Hartley RL, Todd AR, Harrop AR, et al. Pediatric hand fracture referring practices: a scoping review. Plast Surg (Oakv). 2019;27:340–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill C, Riaz M, Mozzam A, et al. A regional audit of hand and wrist injuries: a study of 4873 injuries. J Hand Surg. 1998;23:196–200. [DOI] [PubMed] [Google Scholar]
- 22.Larsen CF, Mulder S, Johansen AM, et al. The epidemiology of hand injuries in the Netherlands and Denmark. Eur J Epidemiol. 2004;19:323–327. [DOI] [PubMed] [Google Scholar]
- 23.Usal H, Beattie TF. An audit of hand injuries in a paediatric accident and emergency department. Health Bull (Edinb). 1992;50:285–287. [PubMed] [Google Scholar]
- 24.Anzarut A, Singh P, Cook G, et al. Continuing medical education in emergency plastic surgery for referring physicians: a prospective assessment of educational needs. Plast Reconstr Surg. 2007;119:1933–1939discussion 1940. [DOI] [PubMed] [Google Scholar]
- 25.Davis TR, Stothard J. Why all finger fractures should be referred to a hand surgery service: a prospective study of primary management. J Hand Surg Br. 1990;15:299–302. [DOI] [PubMed] [Google Scholar]
- 26.Weber DM, Kellenberger CJ, Meuli M. Conservative treatment of stable volar plate injuries of the proximal interphalangeal joint in children and adolescents. Pediatr Emer Care. 2009;25:547–549. [DOI] [PubMed] [Google Scholar]
- 27.Ablove RH, Moy OJ, Peimer CA. Pediatric hand disease. Diagnosis and treatment. Pediatr Clin North Am. 1998;45:1507–24, ix. [DOI] [PubMed] [Google Scholar]
- 28.Al-Qattan MM, Al-Qattan AM. A review of phalangeal neck fractures in children. Injury. 2015;46:935–944. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


