Abstract
This report introduces a new closure technique for the management of intraoperative cerebrospinal fluid (CSF) leakage during endoscopic endonasal surgery. The procedure is based on the combination of a traditional autologous tissue flap with a heterologous fibrin graft (TachoSil). We performed a retrospective analysis on 121 patients with pituitary adenomas treated in our center by the senior neurosurgeon (author V.R.B) in the previous 4 years. Only one patient (0.8%) developed a CSF leakage and no adverse events were found related to the use of TachoSil. Compared with other techniques used previously, sellar diaphragm reconstruction with TachoSil seems to be an effective and inexpensive alternative.
Keywords: CSF leakage, sellar diaphragm, endoscopic endonasal surgery, pituitary adenomas
Introduction
In the past few decades, endoscopic endonasal surgery has become the first treatment option in the management of a great variety of skull base pathologies. The possibility of approaching the anterior, middle, and posterior cranial fossae in a minimally invasive way, together with the improved visualization offered by modern endoscopes, has reduced postoperative complications without compromising the extent of tumor resection compared with transcranial approaches. However, the endoscopic endonasal approach is not risk free. The formation of a cerebrospinal fluid (CSF) fistula is one of the most frequent and severe complications and, although the use of a nasoseptal flap has reduced it significantly, it continues to be a worrisome complication for both neurosurgeons and skull base rhinologists. 1 2
Here, we describe our experience with a simple technique based on a fibrin sponge used to reconstruct the sellar diaphragm anatomically before autologous tissue flap placement. This approach was used in treating 121 consecutive patients with pituitary adenomas.
Methods
Every surgical procedure was performed by the same neurosurgeon (author V.R.B) in collaboration with a rhinology team. In all procedures, before opening the rostrum sphenoidale, the rhinologist takes down a free middle turbinate mucosa flap or a pedicled nasoseptal rescue flap based on the posterior septal artery. We design every flap according to case-specific requirements, basing the decision on pituitary adenoma size and extension.
Once tumor resection is ended, if an intraoperative CSF fistula is not seen, we simply fill the resection cavity with absorbable hemostatic material (oxidized cellulose, Surgicel, Ethicon Inc., a Johnson & Johnson company; Somerville, NJ) and we cover the dural opening with free middle turbinate mucosa. On the other hand, when a diaphragmatic defect with an intraoperative CSF fistula is noted, we aim to make a meticulous multilayer closure. First, we identify and isolate the defect ( Fig. 1A ). Then we introduce a heterologous patch comprising fibrinogen and thrombin (TachoSil, Baxter Healthcare Corp., Deerfield, IL, United States), cut to size for covering the defect but exceeding it by a few mm ( Fig. 1B ), and press on it for 2 minutes with a wet cottonoid. Then we induce Valsalva's maneuvers to check that the closure is tight and after that we fill the sella turcica with Surgicel to keep the patch on the diaphragm. Posteriorly, an autologous flap is placed over the cranial base defect that was previously denuded of mucosa to prevent the formation of a mucocoele. We normally use a free graft except in those cases where we anticipate a high risk of CSF fistula (leaks grade 2 and 3, communication with the suprasellar cisterns, elevated body mass index). 3 4 In such cases, a pedicled nasoseptal flap is placed over the cranial base ( Fig. 1C ). Finally, we place an absorbable material layer, usually made of small Surgicel packages. This is intended to separate the flap from the nonabsorbable tampon-type packing sponges used at the end of the procedure.
Fig. 1.
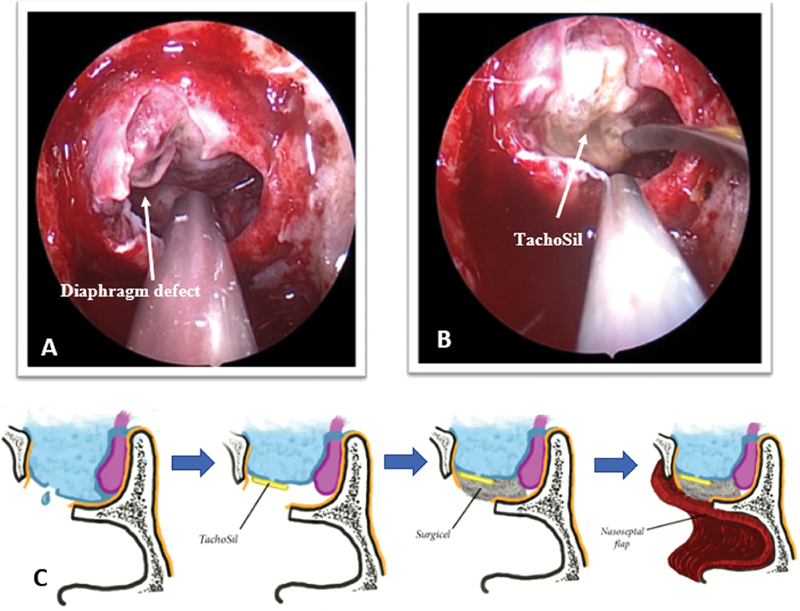
( A ) When we noted an intraoperative CSF fistula, the first step is to identify and isolate the diaphragm defect. ( B ) Then, we introduce a heterologous patch of collagen coated with fibrinogen and thrombin (TachoSil), cut to size for covering the defect. ( C ) Schematic representation of our reconstruction technique of the sellar diaphragm using a multilayer closure with TachoSil combined with pedicled flap.
In no case was lumbar drainage used for prevention or treatment of CSF leaks. After surgery, patients retained the nasal tampon-type packing for 48 hours, and at the postoperative day 3 (prior to discharge), and at 2 weeks after surgery, the rhinology team used fibroscopy to confirm the correct flap position and the absence of CSF leakage.
Here, we assess the effectiveness of this reconstruction method retrospectively by analyzing the results in a series of patients with pituitary adenomas treated in the past 4 years. We have used the development of postoperative CSF leakage or other related complications (meningitis and tension pneumoencephalos) as primary endpoints.
Results
From 2014 to 2017, 121 patients with pituitary adenomas (22 microadenomas, 86 macroadenomas, and 13 giant adenomas) were operated on using our endoscopic technique described above. During the surgical procedures, the sellar diaphragm was disrupted in 24 patients and we performed a closure with fibrinogen and thrombin patches (TachoSil) in all of them followed by an autologous flap (free flap or pedicled flap), as we have mentioned before.
We did not record any cases of CSF leakage in those patients in which the sellar diaphragm stayed intact. Of the 24 patients with breakage of the sellar diaphragm, one developed CSF leakage (4.2%) despite multilayer closure with TachoSil. It must be emphasized that patients with intraoperative CSF leakage had a pituitary adenoma larger than 1 cm (mean size 2.60 cm), whereas the only patient with postoperative CSF leakage had been operated on for a giant adenoma with ventricular growth ( Fig. 2 ) ( Table 1 ). Every patient of our series was followed-up at least 1 year after hospital discharge, with a median follow-up time of 34 months (range: 12–59 months). Likewise, those with intraoperative CSF leaks had a median follow-up time of 31 months (range: 15–52 months). During this time, no cases of meningitis or tension pneumoencephalos were recorded.
Fig. 2.
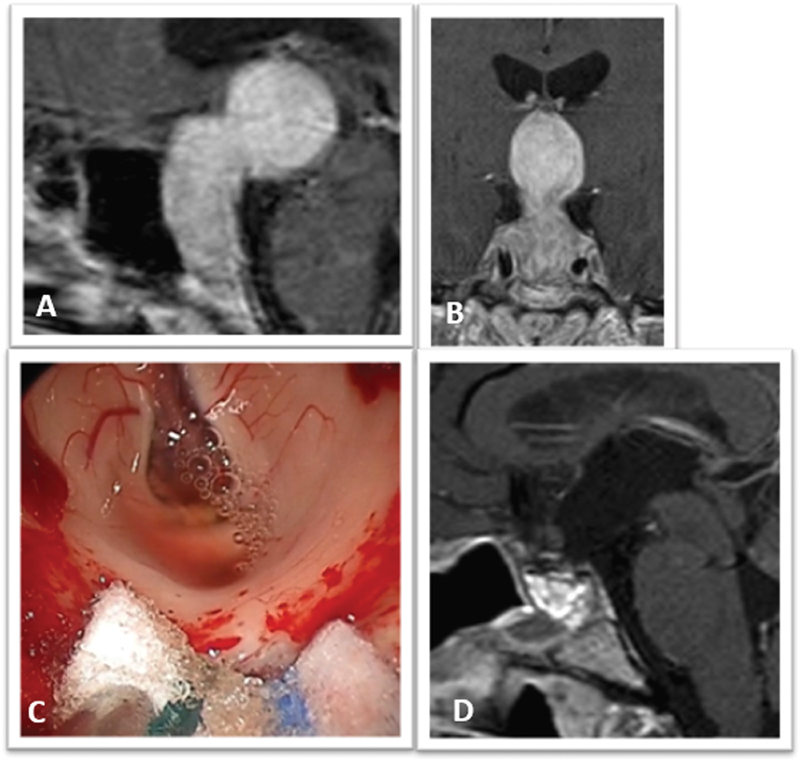
Clinical images of the only case of our series with postoperative CSF leakage. ( A ) Preoperative sagittal and ( B ) coronal contrast-enhanced T1-weighted MRI showing a giant pituitary adenoma (maximum diameter: 5.25 cm) with third ventricular growth. ( C ) Endoscopic view of the third ventricle after adenoma resection. ( D ) Postoperative sagittal contrast-enhanced T1-weight MRI showing complete resection of the tumor. CSF, cerebrospinal fluid; MRI, magnetic resonance imaging.
Table 1. Pituitary adenomas operated from 2014 to 2017 ( n = 121) .
| Cases | Intraoperative CSF leakage | Postoperative complications | |
|---|---|---|---|
| Microadenomas | 22 | 0 | 0 |
| Macroadenomas | 86 | 22 | 0 |
| Giant adenomas | 13 | 2 | 1 |
| Total | 121 | 24 (mean Ø: 2.6 cm) | 1 (max Ø: 5.25 cm) |
Abbreviation: Ø, diameter; CSF, cerebrospinal fluid.
Note: multilayer closure with TachoSil was performed in 24 patients. Only one developed postoperative CSF leakage; no cases of meningitis or tension pneumoencephalos were recorded.
In the only case with a postoperative CSF leakage, we decided to reoperate using again endonasal endoscopic technique. During surgery, a cranial base defect involving incomplete sealing was noted, so we proceeded to repair it with a fascia lata graft. Three days after this procedure, the patient was discharged with no evidence of CSF leakage in the long-term follow-up.
None of our patients had an adverse event that could be linked to the intracranial use of TachoSil.
Discussion
Endoscopic endonasal surgery has revolutionized the management of cranial base pathology. Increased surgical experience together with technological advances in endoscopic equipment have given us the opportunity to expand the surgical indications for this technique. However, CSF leakages are the main problems facing neurosurgeons and rhinologists.
The greatest breakthrough in treating cranial base defects with endoscopic closure has been the development of pedicled flaps, in particular the nasoseptal flap. 5 Today, these allow us to achieve a CSF leakage rate of around 5%, similar to those obtained with open surgery. 1 2 Nevertheless, the use of a flap for preventing CSF leakage is not enough. 6 This is because there are many factors that can precipitate closure failure, such as flap mobilization when we encounter massive CSF leakages, one-way valve formation with the posterior development of air pressure-related pneumoencephalos, or flap necrosis arising from accidental pedicle damage. For these reasons, most centers use a multilayer closure in which, before placing an autologous flap, they place a heterologous collagen patch (Duragen, Integra Sciences, Plainsboro, NJ, United States; Duramatrix Onlay, Stryker, Kalamazoo, MI, United States). 7 8 Our study represents the first work in which a collagen patch covered with fibrinogen and thrombin (TachoSil) is placed before forming an autologous flap, free or pedicled, to achieve anatomical sellar diaphragm reconstruction.
TachoSil is a sponge made of equine collagen coated with human thrombin (2 UI/cm 2 ) and fibrinogen (5.5 mg/cm 2 ). In contact with fluids, it develops a chemical reaction corresponding to the last phase in the blood coagulation cascade, enabling a strong union between the collagen sponge and a wound surface. Originally, the Food and Drug Administration approved it to use as a hemostatic agent and tissue sealant in cardiothoracic and vascular surgery. However, since 2017, it has been approved for using as a dural sealant, after a multicenter study had evidence of CSF leakage rates similar to those of other techniques used previously. 9
When searching the literature, we found three papers that used TachoSil for wound closure after a transsphenoidal microsurgical approach. 10 11 12 However, until now, the experience with this technique in pure endoscopic endonasal surgery and its use with autologous flaps has not been published.
Compared with other collagen patches used previously, TachoSil theoretically offers a greater sealing capacity because fibrin is able to create a firm and stable network based on covalent bonds that close tightly to fix dural defects. In our series, we have observed a postoperative CSF leakage rate of 1/121 (0,8%), lower to other published series of endoscopic pituitary surgery. 13 14 15 Furthermore, we have not registered any case of allergic or adverse reaction following the use of this heterologous matrix.
One of the main disadvantages of using TachoSil in endoscopic surgery is its natural tendency to adhere to wet surfaces, so its introduction through narrow nostrils can be laborious. For that reason, it requires a certain degree of expertise with its management. The surgeons must consider the product's general recommendations, such as to avoid wetting it before introduction and to carefully dry every surgical instrument that will be used. From our experience, we also recommend folding TachoSil to close its active surface before introducing it. We only try to unfold it, once we have reached the sellar diaphragm defect, avoiding adherence to the nostrils. Then, at the level of the sellar diaphragm, we extend it with the aid of a dissector keeping the active surface against the defect, and finally apply pressure with a wet cottonoid for 2 minutes.
We have not noted any increase in surgical duration with this technique and, although we have not done a direct comparative analysis in terms of cost, reconstructive techniques using TachoSil could be significantly cheaper than other methods used previously ( Table 2 ).
Table 2. Comparative cost analysis between collagen patch (Duragen) and collagen patch covered with fibrinogen and thrombin (TachoSil).
| Patch (size in cm) | Price (€) | Area (cm 2 ) | Price/cm 2 (€) |
|---|---|---|---|
| Duragen (5 × 5) | 255 | 25 | 10.20 |
| TachoSil (9.5 × 4.8) | 286 | 45.6 | 6.27 |
The limitations of our study were the retrospective design and the few cases in comparison with other published endoscopy series. Moreover, given that it is a product whose indication for cranial surgery has been approved only recently, it needs more follow-up time to evaluate its long-term security.
Conclusion
This new method for reconstructing the sellar diaphragm employing a collagen sponge coated with fibrinogen and thrombin, combined with autologous flap placement, is effective and safe for preventing CSF leakages during and after endoscopic surgery for patients with pituitary adenomas.
Footnotes
Conflict of Interest The authors have no conflicts of interest to disclose.
References
- 1.Sigler A C, D'Anza B, Lobo B C, Woodard T D, Recinos P F, Sindwani R. Endoscopic skull base reconstruction: an evolution of materials and methods. Otolaryngol Clin North Am. 2017;50(03):643–653. doi: 10.1016/j.otc.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 2.Zanation A M, Thorp B D, Parmar P, Harvey R J. Reconstructive options for endoscopic skull base surgery. Otolaryngol Clin North Am. 2011;44(05):1201–1222. doi: 10.1016/j.otc.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Dlouhy B J, Madhavan K, Clinger J D et al. Elevated body mass index and risk of postoperative CSF leak following transsphenoidal surgery. J Neurosurg. 2012;116(06):1311–1317. doi: 10.3171/2012.2.JNS111837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Esposito F, Dusick J R, Fatemi N, Kelly D F.Graded repair of cranial base defects and cerebrospinal fluid leaks in transsphenoidal surgery Neurosurgery 2007600402295–303., discussion 303–304 [DOI] [PubMed] [Google Scholar]
- 5.Hadad G, Bassagasteguy L, Carrau R L et al. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116(10):1882–1886. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- 6.McCoul E D, Anand V K, Singh A, Nyquist G G, Schaberg M R, Schwartz T H. Long-term effectiveness of a reconstructive protocol using the nasoseptal flap after endoscopic skull base surgery. World Neurosurg. 2014;81(01):136–143. doi: 10.1016/j.wneu.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Jean W C, Felbaum D R, Anaizi A, DeKlotz T R. Endoscopic endonasal approach for transclival resection of a petroclival meningioma: a technical note. Cureus. 2016;8(06):e641. doi: 10.7759/cureus.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarkiss C A, Lee J, Papin J A et al. Pilot study on early postoperative discharge in pituitary adenoma patients: effect of socioeconomic factors and benefit of specialized pituitary centers. J Neurol Surg B Skull Base. 2015;76(04):323–330. doi: 10.1055/s-0035-1549004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.George B, Matula C, Kihlström L, Ferrer E, Tetens V. Safety and efficacy of TachoSil (absorbable fibrin sealant patch) compared with current practice for the prevention of cerebrospinal fluid leaks in patients undergoing skull base surgery: a randomized controlled trial. Neurosurgery. 2017;80(06):847–853. doi: 10.1093/neuros/nyx024. [DOI] [PubMed] [Google Scholar]
- 10.Hong C K, Kim Y B, Hong J B, Lee K S. Sealing of cerebrospinal fluid leakage during conventional transsphenoidal surgery using a fibrin-coated collagen fleece. J Clin Neurosci. 2015;22(04):696–699. doi: 10.1016/j.jocn.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 11.So J, Park H, Sung K-S, Lee K S, Hong C-K. Sandwich technique using fibrin-coated collagen fleece for sellar reconstruction in large dural defects during transsphenoidal surgery. J Clin Neurosci. 2017;43:256–260. doi: 10.1016/j.jocn.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 12.Tamasauskas A, Sinkūnas K, Draf W et al. Management of cerebrospinal fluid leak after surgical removal of pituitary adenomas. Medicina (Kaunas) 2008;44(04):302–307. [PubMed] [Google Scholar]
- 13.Berker M, Hazer D B, Yücel T et al. Complications of endoscopic surgery of the pituitary adenomas: analysis of 570 patients and review of the literature. Pituitary. 2012;15(03):288–300. doi: 10.1007/s11102-011-0368-2. [DOI] [PubMed] [Google Scholar]
- 14.Enseñat J, Quesada J L, Aparicio Jet al. [Prospective comparative study on 50 patients between microsurgical sublabial transsphenoidal approach and endoscopic endonasal transsphenoidal approach] Neurocirugia (Astur) 20092004335–344., discussion 344–345 [PubMed] [Google Scholar]
- 15.Strickland B A, Lucas J, Harris B et al. Identification and repair of intraoperative cerebrospinal fluid leaks in endonasal transsphenoidal pituitary surgery: surgical experience in a series of 1002 patients. J Neurosurg. 2018;129(02):425–429. doi: 10.3171/2017.4.JNS162451. [DOI] [PubMed] [Google Scholar]


