Abstract
Background and Purpose
Cervicocephalic artery dissection is an important cause of stroke. The clinical presentation of dissection can resemble that of benign neurological conditions leading to delayed or missed diagnosis.
Methods
We performed a retrospective cohort study using state-wide administrative claims data from all Emergency Department (ED) visits and admissions at nonfederal hospitals in Florida from 2005–2015 and New York from 2006–2015. Using validated ICD-9-CM codes, we identified adult patients hospitalized for cervicocephalic artery dissection. We defined probable misdiagnosis of dissection as having an ED treat-and-release visit for symptoms or signs of dissection including headache, neck pain, and focal neurological deficits in the 14 days before dissection diagnosis. Multivariable logistic regression was used to compare adverse clinical outcomes in patients with and without probable misdiagnosis.
Results
Among 7,090 patients diagnosed with a dissection (mean age 52.7 years, 44.9% women), 218 (3.1%; 95% CI, 2.7–3.5%) had a preceding probable ED misdiagnosis. After adjustment for demographics and vascular risk factors, there were no differences in rates of stroke (OR 0.82; 95% CI, 0.62–1.09) or in-hospital death (OR 0.26; 95% CI, 0.07–1.08) between dissection patients with and without a probable misdiagnosis at index hospitalization.
Conclusion
We found that approximately 1 in 30 dissection patients were probably misdiagnosed in the 2 weeks before their diagnosis.
Keywords: Cervicocephalic Dissection, Diagnostic Error
Subject terms: Ischemic stroke, Carotid Artery Dissection, Vertebral Artery Dissection
Cervicocephalic artery dissection is uncommon in the general population but a frequent cause of stroke in the young.1–3 While many patients with cervicocephalic artery dissection present with cerebral ischemia, symptoms can be non-specific including isolated headache and cervical pain.4–6
Rates of cervicocephalic artery dissection misdiagnosis in the ED have not been systematically evaluated despite the fact that early identification of dissection represents an important opportunity for stroke prevention.7 We therefore sought to measure the rate of cervicocephalic artery dissection misdiagnosis in the ED using a large, heterogeneous cohort. We also evaluate the effect of probable ED misdiagnosis on the clinical outcomes of dissection patients.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Design
We conducted a retrospective cohort study using statewide administrative claims data collected by the Florida Agency for Health Care Administration and the New York Statewide Planning and Research Cooperative System (Supplemental Methods). The Weill Cornell Medicine institutional review board approved this study and granted a waiver of informed consent.
Subjects
We identified all patients >18 years of age with an index hospitalization for cervicocephalic artery dissection using previously validated International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes (Supplemental Methods).
Measurements
We defined a probable ED misdiagnosis as having had an ED treat-and-release visit for signs and symptoms related to dissection in the 14 days before dissection hospitalization. ED visits for these signs and symptoms were identified using the primary ICD-9-CM discharge diagnosis codes detailed in Supplemental Table I.
We evaluated whether demographics, concomitant head or neck trauma, and stroke risk factors were predictors of probable dissection misdiagnosis. To assess whether probable ED misdiagnosis of cervicocephalic artery dissection was associated with adverse clinical outcomes, we evaluated rates of stroke (ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage) as well as death during hospitalization for dissection using previously validated ICD-9-CM codes (Supplemental Methods).
Statistical Analysis
We calculated proportions with 95% confidence intervals using the exact method. We compared characteristics between groups using the t test for continuous variables and χ2 test for categorical variables. We used multivariable logistic regression to evaluate characteristics associated with increased odds of having a probable ED misdiagnosis and to compare rates of adverse clinical outcomes at the time of dissection hospitalization. Analyses were performed using Stata/MP, version 15 (StataCorp, TX). We used an alpha error of 0.05.
Results
We identified 7,090 patients with a diagnosis of cervicocephalic artery dissection. Mean age was 52.7 years (SD, 16.3) and 3,181 (44.9%) were women. There were 218 (3.1%; 95% CI, 2.7–3.5%) patients with a probable misdiagnosis as evidenced by having an ED treat-and-release visit for symptoms or signs of dissection in the 14 days before dissection diagnosis. Among patients with a probable misdiagnosis, most had an ED visit for headache (n=194/218; 89.0%).
Patients with a probable ED misdiagnosis were younger (43.4 years [SD, 11.0] versus 53.0 years [SD, 16.4]; P<0.001) and more often women (61.9% versus 44.3%; P<0.001; Table 1). In multivariable logistic regression analysis, age (OR: 0.97; 95% CI, 0.96–0.98) was associated with decreased odds of probable dissection misdiagnosis, while female sex (OR 1.76; 95% CI, 1.33–2.34) was associated with higher odds of probable misdiagnosis (Supplemental Table II).
Table 1.
Patient Characteristics, Stratified by Probable Emergency Department Misdiagnosis of Cervicocephalic Artery Dissection
| No Misdiagnosis (N = 6872) | Probable Misdiagnosis (N = 218) | |
|---|---|---|
| Age, mean (SD), y | 53.0 (16.4) | 43.3 (11.0) |
| Female | 3046 (44.3) | 135 (61.9) |
| Race | ||
| White | 4651 (67.7) | 148 (67.9) |
| Black | 797 (11.6) | 22 (10.1) |
| Other | 1424 (20.7) | 48 (22.0) |
| Clinical Features | ||
| Hypertension | 3655 (53.2) | 86 (39.5) |
| Tobacco Use | 632 (9.2) | 17 (7.8) |
| Alcohol Abuse | 1352 (19.7) | 32 (14.7) |
| Payment source | ||
| Medicaid | 900 (13.1) | 23 (10.6) |
| Private Insurance | 3523 (51.3) | 165 (75.7) |
| Self-pay | 377(5.5) | 11 (5.1) |
| Other | 2072 (30.1) | 19 (8.6) |
Data are presented as number (%) unless otherwise specified.
Rates of ED treat-and-release visits steadily increased from 2 weeks before cervicocephalic artery dissection hospitalization to 1 day before dissection hospitalization (0.07% versus 0.54%; P <0.001; Figure 1).
Figure 1. Histogram of Emergency Department Visits before Dissection Diagnosis.
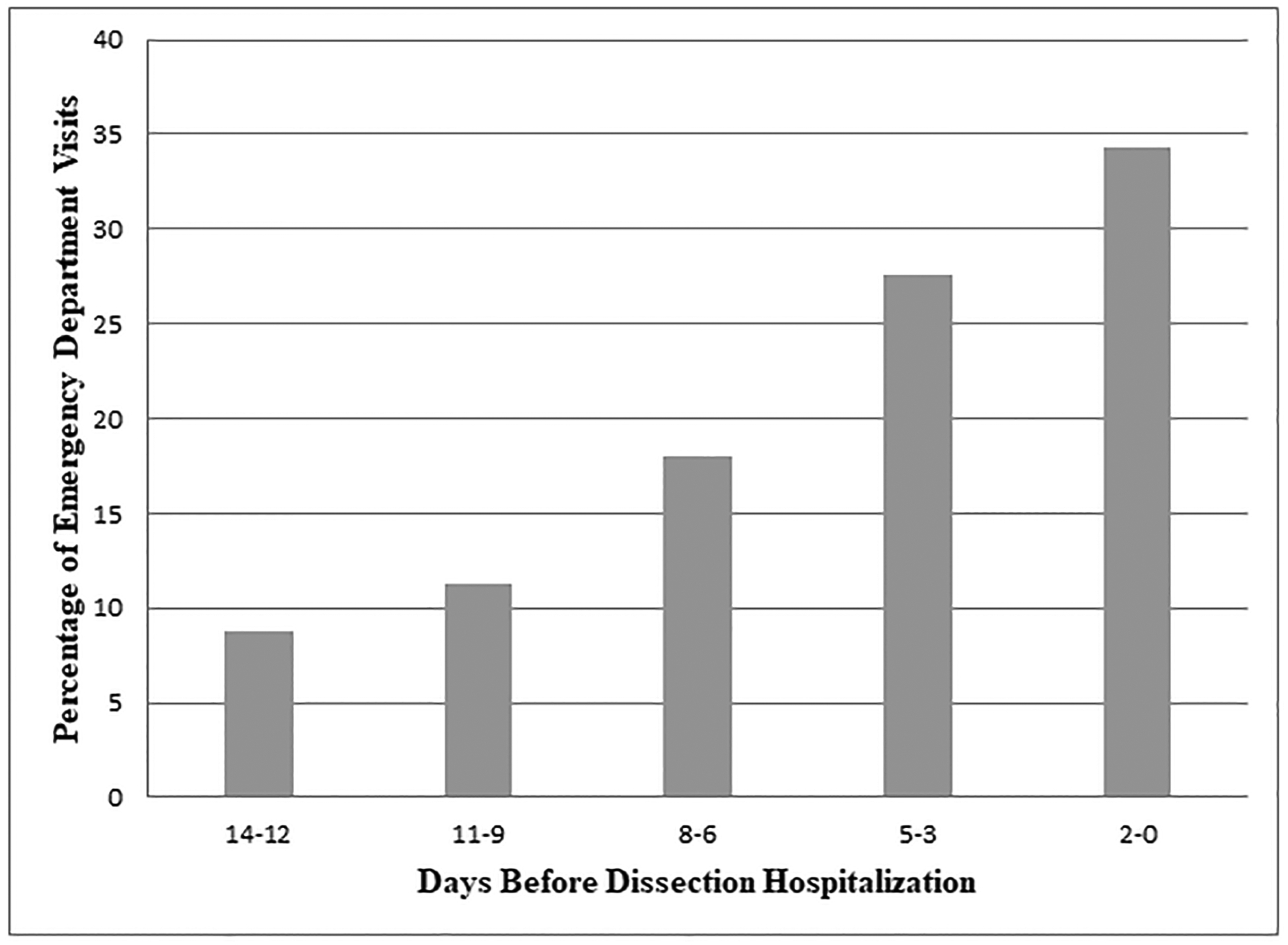
Time (days) from Emergency Department (ED) treat-and-release visit for symptoms or signs of cervicocephalic artery dissection before hospital admission among patients with a probable ED misdiagnosis. ED encounters on the same day of hospital admission (day zero) that resulted in discharge to home are included.
Stroke was diagnosed in 83 (38.1%; 95% CI, 31.6–44.9%) patients with a probable dissection misdiagnosis versus 3,150 (45.8%; 95% CI, 44.7–47.0%; P=0.02) without misdiagnosis. After adjustment for demographics and vascular comorbidities, there was no difference in rates of stroke (OR 0.82; 95% CI, 0.62–1.09) or in-hospital death (OR 0.26; 95% CI, 0.07–1.08) between the two groups.
Discussion
In a large heterogeneous cohort, we found that approximately 1 in 30 cervicocephalic artery dissection patients had a probable preceding ED misdiagnosis. This rate of misdiagnosis is within the range of prior measurements of cerebrovascular disease misdiagnosis in the ED. In a study of patients admitted for stroke or transient ischemic attack using HCUP data from 9 states, the rate of probable misdiagnosis at index ED visit was 1.2%.8 In a Canadian study of 1,507 hospitalized patients with subarachnoid hemorrhage, ED misdiagnosis occurred in 5.4%.9 In our recent study of 5,966 patients with cerebral venous thrombosis, 3.6% had a probable ED misdiagnosis.10 Though these rates of diagnostic error are similar, whether or not there are similar reasons for ED misdiagnosis for these different cerebrovascular diseases requires further study.
We did not find differences in the risk of stroke or in-hospital death among patients with a probable ED misdiagnosis as compared to other dissection patients. However, we were unable to evaluate the impact that diagnosing dissection in the ED may have had on patients who were initially misdiagnosed. It remains plausible that a timely diagnosis of dissection can positively impact patient outcomes by preventing subsequent ischemic events. The short-term risk of incident stroke after isolated cervical artery dissection is non-trivial.7 In the CADISS study, although the frequency of ischemic stroke within one year of dissection was only ~2.5% regardless of treatment allocation, 7% of patients had a minor stroke or TIA an average of 3 days before study enrollment.4, 11 When dissections are diagnosed early, stroke prevention strategies can be initiated to mitigate subsequent stroke risk when this risk is at its highest.4, 7, 11 Improved access to neurological consultation in the ED may help reduce rates of ED stroke misdiagnosis, but further research is needed.12
Our study has important limitations. First, our study is prone to ascertainment error because cases of cervicocephalic artery dissection were identified through diagnostic code claims rather than prospective adjudication. Second, we were unable to account for hospital-level (e.g., teaching status) or provider-level (e.g., years in practice) factors which might affect the accuracy of dissection diagnoses. Third, using data from only two East Coast states as well as excluding patients with a history of cerebrovascular disease may limit the generalizability of our findings. Finally, given the limitations of the HCUP dataset, we were unable to assess stroke severity and functional outcomes.
Conclusions
We found that approximately 1 in 30 patients with cervicocephalic artery dissection had a probable ED misdiagnosis in the 14 days before their hospitalization for dissection. After adjustment for demographics and vascular comorbidities, probable ED misdiagnosis of dissection was not associated with increased odds of stroke or death at index hospitalization.
Supplementary Material
Sources of Funding
ALL is supported by NIH grant K23NS107643. BBN is supported by NIH grants K23NS091395 and R01HL144541, NIDILRR grant 90REGE0012-01-11. HK is supported by NIH grants K23NS082367, R01NS097443, and U01NS095869 and the Michael Goldberg Research Fund. AEM is supported by AHA grant 18CDA34110419 and the Leon Levy Foundation in Neuroscience.
Footnotes
Disclosures
BBN and AEM have received personal fees for medicolegal consulting on stroke. HK is a co-PI for the NIH-funded ARCADIA trial which receives in-kind study drug from the BMS-Pfizer Alliance and in-kind study assays from Roche Diagnostics, serving as Deputy Editor for JAMA Neurology, serving as a steering committee member of Medtronic’s Stroke AF trial (uncompensated), serving on an endpoint adjudication committee for a trial of empagliflozin for Boehringer-Ingelheim, and having served on an advisory board for Roivant Sciences related to Factor XI inhibition.
References
- 1.Giroud M, Fayolle H, Andre N, Dumas R, Becker F, Martin D, et al. Incidence of internal carotid artery dissection in the community of Dijon. J Neurol Neurosurg Psychiatry. 1994;57:1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee VH, Brown RD Jr., Mandrekar JN, Mokri B. Incidence and outcome of cervical artery dissection: A population-based study. Neurology. 2006;67:1809–1812 [DOI] [PubMed] [Google Scholar]
- 3.Beletsky V, Nadareishvili Z, Lynch J, Shuaib A, Woolfenden A, Norris JW, et al. Cervical arterial dissection: Time for a therapeutic trial? Stroke. 2003;34:2856–2860 [DOI] [PubMed] [Google Scholar]
- 4.investigators Ct, Markus HS, Hayter E, Levi C, Feldman A, Venables, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): A randomised trial. Lancet Neurol. 2015;14:361–367 [DOI] [PubMed] [Google Scholar]
- 5.Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995;45:1517–1522 [DOI] [PubMed] [Google Scholar]
- 6.Biller J, Sacco RL, Albuquerque FC, Demaerschalk BM, Fayad P, Long PH, et al. Cervical arterial dissections and association with cervical manipulative therapy: A statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2014;45:3155–3174 [DOI] [PubMed] [Google Scholar]
- 7.Morris NA, Merkler AE, Gialdini G, Kamel H. Timing of incident stroke risk after cervical artery dissection presenting without ischemia. Stroke. 2017;48:551–555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Newman-Toker DE, Moy E, Valente E, Coffey R, Hines AL. Missed diagnosis of stroke in the emergency department: A cross-sectional analysis of a large population-based sample. Diagnosis. 2014;1:155–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vermeulen MJ, Schull MJ. Missed diagnosis of subarachnoid hemorrhage in the emergency department. Stroke. 2007;38:1216–1221 [DOI] [PubMed] [Google Scholar]
- 10.Liberman AL, Gialdini G, Bakradze E, Chatterjee A, Kamel H, Merkler AE. Misdiagnosis of cerebral vein thrombosis in the emergency department. Stroke. 2018;49:1504–1506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Markus HS, Levi C, King A, Madigan J, Norris J, Cervical Artery Dissection in Stroke Study I. Antiplatelet therapy vs anticoagulation therapy in cervical artery dissection: The cervical artery dissection in stroke study (CADISS) randomized clinical trial final results. JAMA Neurol. 2019;76(6):657–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bakradze E, Liberman AL. Diagnostic error in stroke-reasons and proposed solutions. Curr Atheroscler Rep. 2018;20:11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


