Abstract
Corneal keratopigmentation (KTP) has a long history of use in management of patients suffering from disfiguring corneal opacities. Due to progresses and modifications in KTP surgical techniques and its low rate of complications, it is taken into consideration to be used in selected groups of patients for therapeutic or functional indications. In this paper we present an overview on clinical applications of KTP in both cosmetic and functional aspects and also, we discuss the outcomes of KTP and its characteristics in experimental and histopathological studies.
Subject terms: Corneal diseases, Pupil disorders
摘要
角膜墨染术 (Corneal keratopigmentation KTP) 在治疗角膜混浊的患者有着悠久的历史。由于KTP手术技术的更新与改进以及其并发症的低发生率, 因此通常被考虑用于治疗性或功能性适应症的患者。本文阐述了KTP在美容和功能方面的临床应用, 并讨论了KTP的手术效果及其在实验和组织病理学研究中的特点。
Introduction
Keratopigmentation (KTP) better known as corneal tattooing has been used for cosmetic management of corneal opacities for centuries [1, 2].
Different methods have been proposed and modified over the years. The history of corneal tattoos dates back to 2000 years when Galen, a Greek physician, mentioned this method for the first time [3–5]. The same technique was later described by Aetius in 450 AD that was done in an attempt to mask leukomatous opacities of the eye [6]. Both physicians would first cauterise the corneal surface with a heated stilt and after the cauterisation, the dye was applied to the eye using a variety of pigments such as powdered nutgalls, iron or copper sulphate [6, 7]. Following Galen’s reference to corneal tattooing in the 2nd century, the technique was not mentioned until 1869, when an oculoplastic surgeon Louis Von Wecker invented a new method. After anaesthesia with cocaine and putting a thick layer of Indian ink solution over the cornea, he would then insert pigment into the corneal tissue by puncturing the cornea via a grooved needle. This method had influenced corneal tattooing methods since then. Taylor in his new method, used bundle of needles instead of a single needle to tattoo the eye [8]. In 1901, Nieden devised a tattooing needle, based on the idea of a fountain pen, in a method similar to the Edison electric pen [7, 9]. Armaignac used a small funnel fixed to the cornea by small three points. He placed China ink into the instrument and tattoo was done using a needle. This method created a perfectly round pupil [6, 7].
KTP has also been demonstrated as a therapeutic option in patients with symptomatic glare associated with iris loss, atrophy or trauma [10–15] and in subjects with aniridia or iris coloboma to decrease light scattering and photophobia [12, 16–18] and also in the treatment of intractable diplopia [14–19], showing that this technique may not only can be used to improve the cosmetic appearance of blind eyes with leukomas but also it can be performed in sighted eyes for functional problems [20]. More recently it has been used in cases of limbal dermoids [21].
In spite of the advances made in ocular surface reconstructive procedures and the availability of cosmetic contact lenses, KTP could be used as an alternative option in patients with severe cosmetic defects who are intolerant to contact lenses and at high risk for penetrating keratoplasty [18].
Today, various KTP techniques exist. Usually dyes are applied to the anterior stroma following epithelial debridement or trans-epithelial needle puncture (superficial technique). However, several complications including pigment non-homogeneity, colour fading, intraoperative corneal perforation and uveitis occur frequently after the procedure [1, 3, 22]. In addition, the repeated manipulation is painful and there is the risk of recurrent corneal erosions [23, 24].
In a newer method, the dye is applied directly into the stroma (intrastromal technique), with more desirable results in terms of colour distribution and stability; however, it has the risk of uneven tissue dissection or secondary corneal perforation [23, 25, 26].
Femtosecond laser-assisted keratopigmentation (FLAK) is a novel technique that has been recently introduced for performing KTP to restore cosmetic and functional problems [27]. The procedure provides uniform lamellar depth and a smoother stromal bed [28–30]. Femtosecond laser could be applied for lamellar dissection with reduced risk of perforation, in patients with corneal opacity [23].
In this review, we gathered the diverse data with attention being focused on clinical applications of KTP in both cosmetic and therapeutic aspects and also we discussed its outcomes and characteristics in experimental and histopathological studies. In this paper we followed the description and classification of KTP techniques that Alio et al. made in their previous works. Order and contents of the present review, the division of the different techniques, the acronyms and abbreviations and the descriptions are mainly corresponding to their publication [31].
We conducted a wide search on databases including PubMed, Scopus and Google scholar by using specific keywords of corneal tattooing and KTP. Full-text articles of cohort studies, case series and case reports published in English language before February 2019 were selected to be reviewed.
Pigments
During the history of KTP, different pigments have been used, which nowadays, their indications are limited. Some of these pigments have been tested in different immunological and histopathological experiments with acceptable results. Different chemical substances, such as Indian ink, organic colours, Chinese ink, animal uveal pigment, platinum chloride [32], and even soot have been used [3, 9, 32–35]. Pigments, which can provide good cosmetic appearance, have less reactions and do not fade cosmetically are acceptable. CE mark (Conformitѐ Europѐene) pigments are made up of a variety of materials, such as lactic acid, propanediol and other micronized minerals. These pigments have various colours, such as black, green and brown (Biochromaeyes, Blue Green Company, Spain) [36].
KTP methods
Studies have been reported various techniques of KTP including superficial (superficial manual and superficial automated KTP) and intrastromal (manual intralamellar KTP and FLAK) methods [31] (Fig. 1).
Fig. 1. Illustrations of different methods of keratopigmentations (KTP).
a Manual intralamellar KTP to create a corneal pocket. b Creation of corneal flap using femtosecond laser in a lamellar plane. c Superficial automated KTP using automatic micro-puncturing device.
Manual intralamellar KTP (MIK)
The most common technique for corneal tattoo has been done by MIK. This technique has been termed as intrastromal corneal tattoo pocket procedure because in this procedure a pigment is inserted into the anterior corneal stroma through intrastromal corneal pocket [37].
As aforementioned earlier, many patients undergoing KTP for functional or therapeutic purposes have visual dysfunctions and do not have cosmetic indications for KTP. Several studies have reported using a surgical marking pen in order to ensure amelioration of visual symptoms before proceeding with KTP. By applying a temporary mark to the area over a peripheral iridotomy, it will give this chance to the patient to determine whether cosmetic appearance is acceptable after applying KTP procedure [38].
After creating a corneal pocket in the depth of 40–50% of corneal thickness, a radial incision is performed with a calibrated diamond knife, and then the cornea is dissected intralamellary and circumferentially at the same depth until the full depth of the blade is reached. Finally, the pigment will be injected with a 27-gauge needle into the dissected corneal tunnel. In this technique the number of incisions and size of dissection are based on the area of iris defect.
Advantages of this technique are being a safe, rapid and well-tolerated intervention, leaving an intact corneal surface and low rate of complications [37].
Superficial manual KTP (SMK)
This method was the pioneer of KTP techniques and had been applied before development of automated KTP devices. A 25-gauge needle for injecting pigments is used by puncturing the area of cornea repeatedly. Today, SMK is scarcely performed because of the introduction of the automated KTP devices. However, SMK can still be used in cases with small defects need to be obscured [39].
Superficial automated KTP (SAK)
SAK is an automatic micro puncturing of most anterior layers of the corneal stroma to an approximate depth of 120 μm from corneal surface. This technique is done by the Vissum Eye MP system device (Blue Green Medical, Madrid, Spain). By repeating the micro puncturing, the volume of pigments reaches to an acceptable amount for cosmetic appearance [14, 36, 39]. Usually, when the intralamellar KTP is not sufficient to provide adequate cosmetic appearance, superficial KTP can be applied. For both SMK and SAK procedures, ocular topical anaesthetic is used before and during surgery. If the pigmentation is extensive, peribulbar anaesthetic can be used over that area [14].
Femtosecond laser-assisted KTP (FAK)
The use of femtosecond laser in KTP is a novel technique for KTP. The first step prior to FAK is to measure the thickness of cornea to determine the appropriate lamellar depth for femtosecond laser tunnel [13, 15]. The types of FAK technique are single tunnel and double tunnel. In single-tunnel technique, femtosecond laser is applied to make a circular tunnel in cornea. However, the depth of the tunnel should not be <250 µm. Following the opening of the tunnel, the pigments will be injected by a flat cannula. In double-tunnel technique, two intrastromal tunnels are created by femtosecond laser [36]. One of these tunnels should be in greater depth than the other one. Then, a lamellar dissector is used for dissecting the intrastromal tunnels from incisions and to widen the tunnel to reach to the limbal area. Then, dark pigment will be injected into the deeper tunnel [15]. After that, light pigment is injected by automatic micro puncture through the superficial tunnel. Double-technique FAK is often performed for light colour eyes. Dark pigment plays the role of pigmentary epithelium of the iris, which prevents light from entering the eye and alleviate dysphotopsia. The aim of this technique is to improve both visual symptoms and cosmetic appearance of the eye. FAK technique gives this chance to tattoo different areas of cornea. FAK is more accurate, quicker, safer, easier to do, with less postoperative complications and recovery time in comparison with manual intralamellar and superficial corneal tattooing [15].
Cosmetic KTP
Disfiguring corneal opacity and disproportion in the appearance of the eyes are considered as issues that may directly affect personal quality of life and self-confidence of patients. Thus, nowadays several corneal tattooing methods have been used to permanently repair the aesthetic defects of colour changes in the eye for patients (Fig. 2). In addition, some cases are referred and ask for corneal tattooing for purely cosmetic purposes to enhance or change their natural eye colour [39].
Fig. 2.

Keratopigmentation for cosmetic purpose in a visual lost eye with a history of a failed penetrating keratoplasty and total graft opacity.
KTP indications for cosmetic purposes consist of a variable defects, such as total or partial corneal leukomas, that take place in infection, trauma, opacification of the donor–recipient borders in eyes with previous keratoplasty, Chronic corneal oedema that may happen after several unsuccessful keratoplasties, congenital glaucoma or Fuchs dystrophy, phthisis bulbi, sclerocornea, eyes with no sight with paralytic mydriasis or no pupil with the iris pulled backward because of trauma. Moreover, some subjects may do it for purely cosmetic reasons as they tended to change or enhance their eye colour appearances [36, 39, 40].
SAK, FAK, MIK, SMK, small-incision lenticule extraction, intralamellar corneal staining, superficial corneal staining, multiple non-continuous trans-epithelial puncture technique, flap-based tattooing techniques and femtosecond-assisted anterior lamellar corneal tattoo have been reported in different studies for performing KTP [25, 39, 41, 42] (Table 1).
Table 1.
Cosmetic KTP.
| No. | Authors | Number of eyes | Method of KTP | Type of pigment material | Outcomes and follow-up time |
|---|---|---|---|---|---|
| 1 | Alio et al. [36] | 234 eyes | SAK, FAK, MIK | First GP, second GP and third generation CE mark pigments | 12.82% of patients complained of surgical complication (45% organic and 55% functional complications) within 4 months to 13 years FU |
| 2 | Ferrari and van Haselenase [52] | 1 healthy subject | Femtosecond-assisted annular KTP | Pigment neoris®-Biotic | No complications in 8 months FU |
| 3 | Alsmman et al. [53] | 53 blind eyes with corneal disfiguring opacities | Multiple trans-epithelial intrastromal injections | Rotring painting ink | No complications in 12 months FU |
| 4 | Al-Shymali et al. [39] | 127 cosmetically disabled eyes out of entire 136 eyes | SMK and SAK | First GP, second GP and third generation CE mark pigments | No complications reported up to 3 months, 12 eyes (11.2%) developed complications in more than 3 months FU |
| 5 | Jacob et al. [54] | 3 eyes | (SMILE)-assisted sutureless corneal resurfacing with interface tattooing | Dye powder | No complications in 12–25 months FU |
| 6 | Lin et al. [40] | 40 eyes | Anterior stromal puncture | Chinese ink | 3 of 31 patients had recurrent bullae formation and received conjunctival flaps or a TSCL to relieve symptoms in 26.4 months FU |
| 7 | Bandivadekar et al. [21] | 3 eyes | Bare corneal bed tattooing along with simple shave excision | 2% Gold chloride, reduced by 1% hydrazine hydrate | No complications in 12 months FU |
| 8 | Alio et al. [41] | 7 patients for purely cosmetic reasons | SAK, MIK, FAK | Micronized mineral pigments | No complications in 6–30 months FU |
| 9 | Liu et al. [55] | 32 eyes | LK combined with KTP(22 patients) single-personalised KTP (10 patients) | India ink | No complications in 36 months FU |
| 10 | Park et al. [42] | 33 eyes with total corneal opacity | Multiple non-continuous trans-epithelial puncture technique (pointage technique) | Black carbon particle suspension dye | 9% developed delayed corneal epithelial healing in 12 months FU |
| 11 | Hos et al. [25] | 6 eyes | Large lamellar limbus-to-limbus flap-based corneal tattooing and small central flap-based corneal tattooing | Liquid tattooing dyes | No complications in 1 year FU |
| 12 | Irfan et al. [9] | 44 blind eye | Deeply stromal staining by a black precipitate agent | 2% Gold chloride, reduced by 2% hydrazine hydrate | Minimal pigment loss was observed in 5 cases after 3 months and they underwent repeat procedure after 1 year FU |
| 13 | Cha et al. [56] | 9 eyes with limbal dermoids | Inserting dye into the anterior stromal space by creating a long puncture canal | Tissue-marking dye | No complications noted during 3 years FU |
| 14 | Jeong et al. [24] | 6 eyes with total leukoma | Anterior stromal space filling, created by air bubble infiltration | Tissue-marking dye | No complications during surgery and in 14 months FU |
| 15 | Kim et al. [34] | 147 blind eyes | Anterior stroma needle puncturing | Tissue-marking dye | Re-opacification or increased opacity (n = 7), fading of colour (n = 5), epithelial growth (n = 5) in 5 years FU |
| 16 | Alio et al. [35] | 37 out of total 40 eyes with disfiguring corneal opacities or severe leukoma | ICS (28 patients), SCS (8 patients), combined ICS and SCS (4 patients) in total patients | Mineral micronized pigments | No complications noted in 12 months FU |
| 17 | Chang et al. [57] | 401 patients with corneal opacities | Repetitive anterior stromal injection | Tissue-marking dye | No complication noted except two patients had a residual corneal opacity in 15.7 months FU |
| 18 | Fogla et al. [58] | 1 patient with poor cosmetic appearance | Inside the stromal bed over the area of corneal opacity and beneath the flap, overlying the stromal opacity with the help of an iris spatula | Dye powder (organic dye) | No complications during 9 months FU |
| 19 | Kim et al. [23] | 6 eyes with total or partial corneal opacity | Femtosecond laser for dissection and flap creation | Tissue-marking dye | No complications except an incomplete lamellar cut within 6–16 months of FU |
| 20 | Kymionis et al. [26] | 1 subject with leukocoria | FALT | Commercially available black tattoo pigment | No complications during 6 months FU |
| 21 | Lee et al. [59] | 3 cases with corneal opacities | Ink injection beneath the amniotic membrane transplantation | India Ink Reagent Dropper | No complications in 15–20 months FU |
| 22 | Pitz et al. [3] | 11 patients who were not consent for enucleation | Anterior stromal needle puncturing | Commercially available drawing ink | All patients complained about a surgically induced moderate foreign body sensation, conjunctival redness and corneal epithelial defect in 4 years of FU |
SAK superficial automated keratopigmentation, FAK femtosecond-assisted keratopigmentation, MIK manual intralamellar keratopigmentation, GP generations of pigments, SMK superficial manual keratopigmentation, SMILE small-incision lenticule extraction, TSCL therapeutic soft contact lens, LK lamellar keratoplasty, ICS intralamellar corneal staining, SCS superficial corneal staining, FALT femtosecond-assisted anterior lamellar corneal tattoo, FU follow-up
Complications of such procedures are commonly classified by the time of the occurrence to intraoperative and postoperative events. Intraoperative complications mainly include perforation, corneal melting, corneal infections, epithelial erosions, dye leakage into the conjunctival space or anterior chamber and any surgical malpractices (technical mistakes). Whereas, late-onset complications are consisting of light sensitivity, inconsistent dyeing of the opacity, fading of pigments, uveitis, corneal oedema, conjunctivitis, epithelial defects and any visual field limitations. In a comprehensive study, conducted by Alio et al., to evaluate the complications of 234 eyes of 204 patients who underwent for KTP with different techniques via three pigments generation, they showed that 12.82% of all cases were faced complications. The most common complication was complaining of light sensitivity (49%) and the least frequent complications were visual field limitation (4%) and magnetic resonance imaging (MRI) alterations (2%) [36].
Functional KTP
KTP has been used recently for improving functional visual symptoms and is limited to a few studies in comparison with cosmetic purposes (Table 2).
Table 2.
Functional KTP.
| No. | Authors | Number of eyes | Method of KTP | Type of pigment material | Outcomes and FUT |
|---|---|---|---|---|---|
| 1 | Al-shymali et al. [39] | 9 functionally disabled eyes out of entire 136 eyes (6 eyes with aniridia, 2 eyes with albinism, 1 eye with iris cyst) | SMK, SAK | First GP, second GP and third generation CE mark pigments | Postoperative complications: 1 patient with pain while undergoing MRI in FU < 3 months and 12 eyes with organic complications in FU > 3 months (2-neovascularization, 6-colour fading and 7-change in colour in 2.4–14 years FU |
| 2 | Tone et al. [38] | 5 eyes with post-LPI dysphotopsias | MIK | An alcohol-based commercially available black tattoo pigment | Immediate postoperative relief in all symptoms of patients |
| 3 | Ricardo et al. [22] | 2 eyes with post PI symptoms | FAK | Black and brown tattoo pigments | Total elimination of symptoms, and no significant complications in 6–8 months FU |
| 4 | Alio et al. [15] | A case with unilateral Urrets-Zavalia syndrome | Double-intrastromal tunnel FAK | Mineral micronized black pigment | No postoperative complications in 12 months FU |
| 5 | Segal et al. [37] | 5 eyes with post PI symptoms | Intrastromal lamellar pocket technique | Commercially available black pigment | No major complications but postoperatively, all patients complained of mild irritation and/or photophobia, lasting from 2 days to 2 weeks |
| 6 | Alio et al. [13] | A case of essential iris atrophy | FAK | Mineral micronized pigment | No intraoperative or postoperative complications 12 months FU |
| 7 | Alio et al. [14] | 11 eyes with iris defects | MIK (8 patients), MIK + SAK (2 patients), FAK (1 patient) | Mineral micronized pigments | No major complications in any patients in 3–12 months FU |
| 8 | Gupta et al. [43] | Complicated PI | Intrastromal lamellar pocket technique | Black sterile marking ink | No complications in 12 months FU |
| 9 | Islam et al. [44] | Post PI symptoms | Corneal stromal pocket anterior to PI | Hydrazine hydrate solution | No complications in 20 months FU |
FUT follow-up time, GP generations of pigments, MIK manual intralamellar keratopigmentation, SAK superficial automated keratopigmentation, SMK superficial manual keratopigmentation, FAK femtosecond-assisted keratopigmentation, PI peripheral iridotomy
Patients undergoing KTP for therapeutic reasons usually complain of photophobia, diplopia, glare and halos, which are usually secondary to iris defects, aniridia, iridodialysis and iris atrophies after trauma or anterior segment surgery, such as peripheral iridotomies, and even congenital defects, such as albinism or essential iris atrophies [14, 22, 37, 43, 44]. Based on observations, patients who underwent corneal tattooing were intolerant or unwilling to accept other alternative therapeutic options, such as cosmetic contact lens, iris suturing or implantation of an artificial iris [14].
KTP satisfaction and complications
The complications of KTP are basically classified into organic and functional complications. The toxicity of the pigments and their durability has been one of the main concerns.
Visual field limitation, light sensitivity and MRI alterations are considered as functional complications. Change in colour, colour fading and neovascularization are described as organic complications. Potential risks of KTP include corneal perforation (Fig. 3), toxic reaction to pigment, microbial infection and undesirable migration of pigment [36, 38]. Based on previous studies, organic complications usually occur with first- and second-generation pigments. KTP with third-generation pigments is more effective in ameliorating visual symptoms and improving cosmetic appearance. KTP outcomes can be influenced by depth of injection and composition of pigments. Current investigations indicate that deep corneal tunnels have better outcomes than superficial ones. Washing eyes after KTP is reported to decrease the risk of light sensitivity [36].
Fig. 3.
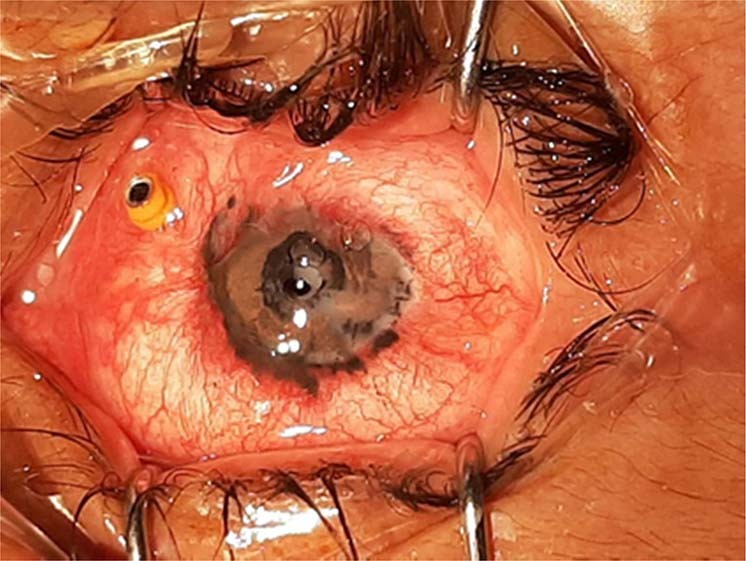
A previously silicone oil filled eye with corneal perforation after a recent femtosecond laser-assisted keratopigmentation.
There are controversial ideas about MRI after KTP. Several studies suggest that heavy metals, such as iron, found in tattoos may cause alteration of local magnetic field and distort the image of the globe. Also, some patients reported that they complained pain when they underwent MRI in less than 3 months after KTP [14, 36, 37]. However, another study did not report serious soft tissue reactions or adverse events during MRI [45].
One of the rare complications after KTP is granulomatous keratitis, which has been reported to be induced by multiple stromal puncture techniques. Stromal infiltration and granulomatous reaction around the pigment in absence of viral, fungal and bacterial pathogens suggest granulomatous keratitis [46].
Experimental studies
In 2011, Sirerol et al. conducted an experimental animal study on the two groups of hens to investigate the tolerance, biocompatibility and cosmetic outcomes of a new mineral micronized pigment in corneal tattooing. The central intralamellar KTP was performed by a new pigment formulation (iron oxide, ferric oxide yellow and pigment blue). All hens were regularly examined by a slit lamp to detect any sign of postoperative adverse effects, such as corneal inflammation, pigment diffusion, colour changes and any sign of neovascularization within 1 month (group A) and 3 months (group B), which resulted in acceptable cosmetic appearance without corneal complications during the follow-up period [18]. In another study with the same materials and method which was conducted on 28 eyes of 14 white rabbits by Amesty et al., favourable outcomes were achieved and the corneas showed a good appearance cosmetically [47].
Moreover, Alsmman Hassan and Abd Soliman Elhaliem have investigated the safety and effectiveness of corneal tattooing by Rotring China painting ink in their experimental animal study. Ten corneas of ten male rabbits were successfully stained by the foregoing pigment and animals were kept for duration of 6 months follow-up. During this period, there were no sign of corneal ulceration or intraocular inflammation and no significant complication has been reported. In addition, lately the animals were enucleated for further histological evaluation, which resulted in no findings in favour of abnormal dispersion of stain inside the cornea or infiltration of inflammatory cells through the tissue [48]. Rodriguez et al. conducted an experimental study to assess the tolerance and outcomes of micronized mineral pigments by using SAK technique for the first time. In this regard, 40 eyes of 40 rabbits were divided into two groups of iris-simulated tattooed with different colours and pupil-simulated black tattooed and eventually, all eyes were enucleated after 6 months of follow-up in order to investigate the histological outcomes of this procedure including possible pigment dispersion, inflammation or neovascularization. The results of slit-lamp examination in 2, 4 and 6 months’ follow-ups were unremarkable. Only a mild-to-moderate conjunctival injection and transitory corneal epithelial defects were detected in 13 and 27 eyes at the first week of surgery, respectively. In addition, good aesthetic appearance was achieved for all eyes after SAK procedure and no sign of defect and abnormality was detected in corneal histopathological study [27].
Histopathological studies
In Amesty et al. study, histopathological examination revealed no evidence of pigment effusion or colour change, stromal inflammation and neovascularization in treated corneas coloured with micronized mineral pigments [20].
To evaluate long-term ultrastructural changes in non-metallic corneal tattooing, Sekundo et al. examined two tattooed eyes that were obtained by penetrating keratoplasty. On transmission electron microscopy there were no granules in extracellular matrix. They concluded that particles of non-metallic dyes can actively be ingested and retained within the cell membrane of keratocytes for a very long time [16].
In 1987, Fujita et al. injected India ink particles and polystyrene latex beads into the corneal stroma of rabbits. They demonstrated that rabbit corneal fibroblasts can endocytosis the particles within a period of 3–4 days after injection; besides, all those particles were stored unchanged for 6 months [49].
In Takahashi et al.'s study, Indian ink particles were found both intracellular and extracellular in the corneas of three Japanese patients who received KTP 12, 20 and 34 years earlier [50]. To compare metallic tattoo with non-metallic tattoo, ultrastructural studies demonstrated intracellular granules in keratocytes in non-metallic tattoo and intracellular and extracellular granules in the metallic one using platinum chloride [16, 51].
In conclusion, with all the evidence raised and the clinical studies published it is clear that KTP offers today an excellent option for the corneal surgeon that provides acceptable functional and cosmetic outcomes in disabled corneas, irregular pupils or traumatic iris injuries, which can be performed with different procedures. With great advances in KTP technology and recent micro-granulated mineral pigments which donate better results, it seems needing to be popularised and pervasive.
Acknowledgements
We acknowledge Dr Alio and his colleagues because of their great work in developing the novel system of keratopigmentation. Also, we would like thank Danial Alebouyeh for his contribution in designing the illustrations used in this paper.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mannis MJ, Eghbali K, Schwab IR. Keratopigmentation: a review of corneal tattooing. Cornea. 1999;18:633. [PubMed] [Google Scholar]
- 2.Duke-Elder SL. System of ophthalmology, vol 3: diseases of the outer eye part 2. London: Henry Kimpton; 1965.
- 3.Pitz S, Jahn R, Frisch L, Duis A, Pfeiffer N. Corneal tattooing: an alternative treatment for disfiguring corneal scars. Br J Ophthalmol. 2002;86:397–9. doi: 10.1136/bjo.86.4.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samderubun EMvdV, Kok JH. Dermatology as a modern treatment for coloring leucoma corneae. Cornea. 1994;13:349–53. doi: 10.1097/00003226-199407000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Holth S. Revival of Galen’s corneal staining with coppersulfate and tannine should be abandoned. Am J Ophthalmol. 1931;14:378–9. [Google Scholar]
- 6.Ziegler SL. Multicolor tattooing of the cornea. Trans Am Ophthalmol Soc. 1922;20:71. [PMC free article] [PubMed] [Google Scholar]
- 7.Hassan A, Hamad A, Soliman AE, Gamal-Eldeen N. Intrastromal injection of China painting ink in corneas of male rabbits: clinical and histological study. J Ophthalmol. 2016;2016:1–6. [DOI] [PMC free article] [PubMed]
- 8.Roy J. Tattooing of the cornea. Can Med Assoc J. 1938;39:436. [PMC free article] [PubMed] [Google Scholar]
- 9.Irfan S, Rashid F, Shahzad I. To assess the efficacy of chemical corneal tattooing for unsightly corneal scars. Pak J Ophthalmol. 2014;30:151–155.
- 10.Reed JW. Corneal tattooing to reduce glare in cases of traumatic iris loss. Cornea. 1994;13:401–5. doi: 10.1097/00003226-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Remky A, Redbrake C, Wenzel M. Intrastromal corneal tattooing for iris defects. J Cataract Refract Surg. 1998;24:1285–7. doi: 10.1016/s0886-3350(98)80215-0. [DOI] [PubMed] [Google Scholar]
- 12.Beekhuis WH, Drost B, der Velden E. A new treatment for photophobia in posttraumatic aniridia: a case report. Cornea. 1998;17:338–41. [PubMed] [Google Scholar]
- 13.Alió JL, Rodriguez AE, Toffaha BT, Piñero DP, Moreno LJ. Femtosecond-assisted keratopigmentation for functional and cosmetic restoration in essential iris atrophy. J Cataract Refract Surg. 2011;37:1744–7. doi: 10.1016/j.jcrs.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Alio JL, Rodriguez AE, Toffaha BT. Keratopigmentation (corneal tattooing) for the management of visual disabilities of the eye related to iris defects. Br J Ophthalmol. 2011;95:1397–401. doi: 10.1136/bjophthalmol-2011-300170. [DOI] [PubMed] [Google Scholar]
- 15.Alio JL, Rodriguez AE, Toffaha BT, El Aswad A. Femtosecond-assisted keratopigmentation double tunnel technique in the management of a case of Urrets-Zavalia syndrome. Cornea. 2012;31:1071–4. doi: 10.1097/ICO.0b013e318243f6b1. [DOI] [PubMed] [Google Scholar]
- 16.Sekundo W, Seifert P, Seitz B, Loeffler KU. Long term ultrastructural changes in human corneas after tattooing with non-metallic substances. Br J Ophthalmol. 1999;83:219–24. doi: 10.1136/bjo.83.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burris TE, Holmes-Higgin DK, Silvestrini TA. Lamellar intrastromal corneal tattoo for treating iris defects (artificial iris) Cornea. 1998;17:169–73. doi: 10.1097/00003226-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Sirerol B, Walewska-Szafran A, Alio JL, Klonowski P, Rodriguez AE. Tolerance and biocompatibility of micronized black pigment for keratopigmentation simulated pupil reconstruction. Cornea. 2011;30:344–50. doi: 10.1097/ICO.0b013e3181eae251. [DOI] [PubMed] [Google Scholar]
- 19.Laria C, Alió J, Piñero D. Intrastromal corneal tattooing as treatment in a case of intractable strabismic diplopia (double binocular vision) Binocul Vis Strabismus Q. 2010;25:238–42. [PubMed] [Google Scholar]
- 20.Amesty MA, Rodriguez AE, Hernández E, De Miguel MP, Alio JL. Tolerance of micronized mineral pigments for intrastromal keratopigmentation: a histopathology and immunopathology experimental study. Cornea. 2016;35:1199–205. doi: 10.1097/ICO.0000000000000900. [DOI] [PubMed] [Google Scholar]
- 21.Bandivadekar P, Agarwal T, Temkar S. Shave excision with keratopigmentation for limbal dermoid. Eye Contact Lens. 2018;44:e7–e9. doi: 10.1097/ICL.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 22.da Silva Ricardo JR, Medhi J, Pineda R. Femtosecond laser-assisted keratopigmentation for the management of visual disabilities due to peripheral iridectomies. J Glaucoma. 2015;24:e22–e4. doi: 10.1097/IJG.0000000000000057. [DOI] [PubMed] [Google Scholar]
- 23.Kim J-H, Lee D, Hahn T-W, Choi S-K. New surgical strategy for corneal tattooing using a femtosecond laser. Cornea. 2009;28:80–4. doi: 10.1097/ICO.0b013e318181a83c. [DOI] [PubMed] [Google Scholar]
- 24.Jeong J, Lee HJ, Lee SH. Corneal tattooing method using dye injection into the anterior stroma infiltrated with small air bubbles. Acta Ophthalmol. 2013;91:e417–e8. doi: 10.1111/aos.12098. [DOI] [PubMed] [Google Scholar]
- 25.Hos D, Heindl LM, Bucher F, Cursiefen C. Novel lamellar, flap-based tattooing techniques for corneal opacities in scarred and vascularized blind eyes. Cornea. 2015;34:82–6. doi: 10.1097/ICO.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 26.Kymionis GD, Ide T, Galor A, Yoo SH. Femtosecond-assisted anterior lamellar corneal staining-tattooing in a blind eye with leukocoria. Cornea. 2009;28:211–3. doi: 10.1097/ICO.0b013e3181859fbb. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez AE, Amesty MA, El Bahrawy M, Rey S, del Barrio JA, Alio JL. Superficial automated keratopigmentation for iris and pupil simulation using micronized mineral pigments and a new puncturing device: experimental study. Cornea. 2017;36:1069–75. doi: 10.1097/ICO.0000000000001249. [DOI] [PubMed] [Google Scholar]
- 28.Binder PS. Flap dimensions created with the IntraLase FS laser. J Cataract Refract Surg. 2004;30:26–32. doi: 10.1016/S0886-3350(03)00578-9. [DOI] [PubMed] [Google Scholar]
- 29.Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30:804–11. doi: 10.1016/j.jcrs.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 30.Sarayba MA, Ignacio TS, Tran DB, Binder PS. A 60 kHz IntraLase femtosecond laser creates a smoother LASIK stromal bed surface compared to a Zyoptix XP mechanical microkeratome in human donor eyes. J Refract Surg. 2007;23:331–7. doi: 10.3928/1081-597X-20070401-04. [DOI] [PubMed] [Google Scholar]
- 31.Alio Jorge, Amesty María. Text and Atlas on Corneal Pigmentation. 2015. Pigments Selection; pp. 7–7. [Google Scholar]
- 32.Duggan JN, Nanavati B. Tattooing of corneal opacity with gold and platinum chloride. Br J Ophthalmol. 1936;20:419. doi: 10.1136/bjo.20.7.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pitz S, Jahn R, Frisch L, Duis A, Pfeiffer N. Corneal tattooing. Present-day evaluation of a historic treatment method. Ophthalmologe. 2000;97:147. doi: 10.1007/s003470050025. [DOI] [PubMed] [Google Scholar]
- 34.Kim C, Kim KH, Han YK, Wee WR, Lee JH, Kwon J-W. Five-year results of corneal tattooing for cosmetic repair in disfigured eyes. Cornea. 2011;30:1135–9. doi: 10.1097/ICO.0b013e3181f2391a. [DOI] [PubMed] [Google Scholar]
- 35.Alio JL, Sirerol B, Walewska–Szafran A, Miranda M. Corneal tattooing (keratopigmentation) with new mineral micronised pigments to restore cosmetic appearance in severely impaired eyes. Br J Ophthalmol. 2010;94:245–9. doi: 10.1136/bjo.2008.149435. [DOI] [PubMed] [Google Scholar]
- 36.Alio JL, Al-Shymali O, Amesty MA, Rodriguez AE. Keratopigmentation with micronised mineral pigments: complications and outcomes in a series of 234 eyes. Br J Ophthalmol. 2018;102:742–7. doi: 10.1136/bjophthalmol-2017-310591. [DOI] [PubMed] [Google Scholar]
- 37.Segal L, Choremis J, Mabon M. Intrastromal corneal tattooing for symptomatic iridotomies. Br J Ophthalmol. 2012;96:464–5. doi: 10.1136/bjophthalmol-2011-300923. [DOI] [PubMed] [Google Scholar]
- 38.Tone SO, Li DQ, Ashkenazy Z, Borovik A, Slomovic AR, Rootman DS, et al. Simple preoperative ink test as a novel adjunct to intrastromal keratopigmentation for post-laser peripheral iridotomy dysphotopsias. Cornea. 2017;36:1282–4. doi: 10.1097/ICO.0000000000001288. [DOI] [PubMed] [Google Scholar]
- 39.Al-Shymali O, Rodriguez AE, Amesty MA, Alio JL. Superficial keratopigmentation: an alternative solution for patients with cosmetically or functionally impaired eyes. Cornea. 2019;38:54–61. doi: 10.1097/ICO.0000000000001753. [DOI] [PubMed] [Google Scholar]
- 40.Lin H-C, Wang Y-L, Chen G-W, Yen C-H. Corneal tattooing and anterior stromal puncture for treating symptomatic bullous keratopathy. Cornea. 2016;35:355–7. doi: 10.1097/ICO.0000000000000693. [DOI] [PubMed] [Google Scholar]
- 41.Alió JL, Rodriguez AE, El Bahrawy M, Angelov A, Zein G. Keratopigmentation to change the apparent color of the human eye: a novel indication for corneal tattooing. Cornea. 2016;35:431–7. doi: 10.1097/ICO.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 42.Park JH, Um T, Kim MJ, Tchah H, Kim JY. A new multiple noncontinuous puncture (pointage) technique for corneal tattooing. Int J Ophthalmol. 2015;8:928. doi: 10.3980/j.issn.2222-3959.2015.05.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gupta D, Broadway D. cost-effective tattooing: the use of sterile ink for corneal tattooing after complicated peripheral iridotomies an alternative to expensive salts. J Glaucoma. 2010;19:566–7. doi: 10.1097/IJG.0b013e3181ca771e. [DOI] [PubMed] [Google Scholar]
- 44.Islam N, Franks W. Therapeutic corneal tattoo following peripheral iridotomy complication. Eye. 2006;20:389. doi: 10.1038/sj.eye.6701861. [DOI] [PubMed] [Google Scholar]
- 45.Tope WD, Shellock FG. Magnetic resonance imaging and permanent cosmetics (tattoos): survey of complications and adverse events. J Magn Reson Imaging. 2002;15:180–4. doi: 10.1002/jmri.10049. [DOI] [PubMed] [Google Scholar]
- 46.Sharma A, Gupta P, Dogra MR, Hidayat AA, Gupta A. Granulomatous keratitis following corneal tattooing. Indian J Ophthalmol. 2003;51:265. [PubMed] [Google Scholar]
- 47.Amesty MA, Alio JL, Rodriguez AE. Corneal tolerance to micronised mineral pigments for keratopigmentation. Br J Ophthalmol. 2014;98:1756–60. doi: 10.1136/bjophthalmol-2014-305611. [DOI] [PubMed] [Google Scholar]
- 48.Alsmman Hassan AH, Abd Soliman Elhaliem NG-E. Intrastromal injection of china painting ink in corneas of male rabbits: clinical and histological study. J Ophthalmol. 2016;2016:8145926. doi: 10.1155/2016/8145926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fujita H, Ueda A, Nishida T, Otori T. Uptake of India ink particles and latex beads by corneal fibroblasts. Cell Tissue Res. 1987;250:251–5. doi: 10.1007/BF00219069. [DOI] [PubMed] [Google Scholar]
- 50.Takahashi J, Sakimoto T, Kitano S. The phagocytosis in the stroma of tattooed cornea. Atarashii Ganka. 1990;7:725–8. [Google Scholar]
- 51.Olander K, Kanai A, Kaufman H. An analytical electron microscopic study of a corneal tattoo. Ann Ophthalmol. 1983;15:1046–9. [PubMed] [Google Scholar]
- 52.Ferrari F, van Haselen R. The safety and effectiveness of a novel annular keratopigmentation method: a case report. Case Rep Ophthalmol. 2018;9:35–42. doi: 10.1159/000485554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alsmman AH, Mostafa EM, Mounir A, Farouk MM, Elghobaier MG, Radwan G. Outcomes of corneal tattooing by rotring painting ink in disfiguring corneal opacities. J Ophthalmol. 2018;2018:5971290. doi: 10.1155/2018/5971290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jacob S, Narasimhan S, Agarwal A, Agarwal A, Ai S. Combined interface tattooing and fibrin glue-assisted sutureless corneal resurfacing with donor lenticule obtained from small-incision lenticule extraction for limbal dermoid. J Cataract Refract Surg. 2017;43:1371–5. doi: 10.1016/j.jcrs.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 55.Liu X, Shen JH, Zhou Q, Liu ZX, Tang SF, Chen RR, et al. Personalised lamellar keratoplasty and keratopigmentation in Asian corneal leucoma patients. Int J Clin Exp Med. 2015;8:9446–53. [PMC free article] [PubMed] [Google Scholar]
- 56.Cha DM, Shin K-H, Kim KH, Kwon J-W. Simple keratectomy and corneal tattooing for limbal dermoids: results of a 3-year study. Int J Ophthalmol. 2013;6:463. doi: 10.3980/j.issn.2222-3959.2013.04.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chang KC, Kwon JW, Han YK, Wee WR, Lee JH. The epidemiology of cosmetic treatments for corneal opacities in a Korean population. Korean J Ophthalmol. 2010;24:148–54. doi: 10.3341/kjo.2010.24.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fogla R, Gupta A, Indumathy TR. Microkeratome-assisted corneal tattooing: a case report. Cornea. 2010;29:446–8. doi: 10.1097/ICO.0b013e3181ae2560. [DOI] [PubMed] [Google Scholar]
- 59.Lee JE, Jun JB, Choi HY, Oum BS, Lee JS. Corneal tattooing to mask subsequent opacification after amniotic membrane grafting for stromal corneal ulcer. Acta Ophthalmol Scand. 2006;84:696–8. doi: 10.1111/j.1600-0420.2006.00680.x. [DOI] [PubMed] [Google Scholar]



