Abstract
Purpose
Given increasing interest in using the capability approach for health economic evaluations and a growing literature, this paper aims to synthesise current information about the characteristics of capability instruments and their application in health economic evaluations.
Methods
A systematic literature review was conducted to assess studies that contained information on the development, psychometric properties and valuation of capability instruments, or their application in economic evaluations.
Results
The review identified 98 studies and 14 instruments for inclusion. There is some evidence on the psychometric properties of most instruments. Most papers found moderate-to-high correlation between health and capability measures, ranging between 0.41 and 0.64. ASCOT, ICECAP-A, -O and -SCM instruments have published valuation sets, most frequently developed using best–worst scaling. Thirteen instruments were originally developed in English and one in Portuguese; however, some translations to other languages are available. Ten economic evaluations using capability instruments were identified. The presentation of results show a lack of consensus regarding the most appropriate way to use capability instruments in economic evaluations with discussion about capability-adjusted life years (CALYs), years of capability equivalence and the trade-off between maximisation of capability versus sufficient capability.
Conclusion
There has been increasing interest in applying the capability-based approach in health economic evaluations, but methodological and conceptual issues remain. There is still a need for direct comparison of the different capability instruments and for clear guidance on when and how they should be used in economic evaluations.
Keywords: Capability approach, Patient reported outcome measures, Outcome, Validation, Preference weighting, Economic evaluation
Background
Economic evaluations assess whether an intervention provides value for money through the comparative analysis of alternative courses of action in terms of both costs and consequences [1]. The assessment of consequences in economic evaluation requires information about their identification (what), measurement (how much) and valuation (how valuable) [2]. Standard methods of health economic evaluations identify outcomes based on a rather narrow definition of health that aims to express outcomes in Quality-Adjusted Life Years (QALYs). However, there are many interventions, particularly in the areas of mental health, end-of-life care, public health and social care, where the impacts of interventions go beyond this narrow view of health. The contemporary literature (e.g. [3–6]) recognises the need to move away from the standard methods for assessing effects of interventions and toward incorporating outcomes beyond the QALY framework, when producing an economic evaluation which feeds into decision making about resource allocation in health-related interventions. The most promising approach to address this issue is the application of Sen’s capability framework, which was introduced by Sen [7] in the early 1980s as an alternative to standard utilitarian welfare economics. The core focus of the capability approach is on what individuals are able to be and do in their lives (i.e. capable of). The application of the capability approach in health economics has gained popularity because it potentially provides a richer evaluative space for the evaluation of interventions [8].
There has been increasing interest in developing instruments for using the capability approach in the measurement and valuation of outcomes for health economic evaluations. Capability instruments have been in the public domain for over a decade and publications have started to shift from methodological issues towards use of the measures within economic evaluations. Some decision-making institutions currently recommend the inclusion of capability measures in economic evaluations in certain contexts. The Zorginstituut in the Netherlands [9] recommends the inclusion of ICEpop CAPability measure for Older people (ICECAP-O) alongside the EuroQol instrument (EQ-5D) for the evaluation of interventions in long-term care, where the relevant outcomes extend beyond health. The most recent methods guideline [10] of the National Institute for Health and Care Excellence (NICE) acknowledges that the intended outcomes of interventions go beyond changes in health status for some decision problems; hence, ‘broader, preference weighted measures of outcomes, based on specific instruments, may be more appropriate…’ and ‘the economic analysis may also consider effects in terms of capability and well-being’ (p. 137). The manual specifically recommends the Adult Social Care Outcomes Toolkit (ASCOT) and ICECAP-O instruments.
However, the choice between instruments and their practical application in particular contexts lack a systematic approach. For instance, the ICECAP-O recommended by NICE is targeted at a subgroup of the population (older adults), whilst the ASCOT was specifically developed for the assessment of social care interventions. A recent review of the literature examined current trends in the application of ICECAP-O [11]. The authors found that the ICECAP-O has mainly been included as a secondary economic measure and the reporting of results is brief with minimal detail and often no discussion or interpretation. An overview of the psychometric properties of all potential capabilities instruments and their usefulness for economic evaluations would contribute to providing a clear guidance. This could later be used as a reference point for future comparative analysis of policies or interventions. Hence, the main aim of this paper is to synthesise the current evidence about the application of capability instruments in health economic evaluations. This translates into the following objectives: (i) to summarise information about the development, psychometric properties and preference valuation of relevant capability instruments; (ii) to compare the identified capability instruments in terms of their psychometric properties and up-to-date application in health economic evaluations; (iii) to identify applied evaluations that have used the capability-based approach in health economic evaluations and (iv) to pinpoint the challenges and considerations in the application of the capability approach in economic evaluations of health-related interventions.
Methods
Identification of relevant studies
The identification of papers was based on two main approaches: a traditional systematic literature search and a comprehensive pearl growing method [12]. The grey literature search in Google Advance either generated an unmanageable number of hits due to the term “capability” being used across a number of disciplines with varying meanings, as well as having generic lay use and interpretation of the term; or there was no addition to the search of other databases when more precise terms were used. As the development and validation of the capability approach in health economics currently appears to be concentrated among a limited group of researchers, as an additional step, websites dedicated to the instruments identified through the systematic search were specifically targeted and reviewed for relevant information.
Systematic literature search
Firstly, we conducted a systematic literature search. Search terms combined expressions for economic evaluation and frequently used terms for the capability approach, including synonyms and names of instruments most well-known in the area of health economics. Search terms are presented in Appendix 1. The selection of databases was based on similar reviews of health measures (PROMs) [6, 13] in the area and included Embase, Medline, Web of Science, Psychinfo and Scopus. The literature search was conducted on 1 February 2019 and the review was limited to the last 20 years when the first publications in this topic area appeared [14]. Relevant systematic literature reviews were searched for further references and their findings were kept for comparison and discussion.
Comprehensive pearl growing method
The term ‘capability’ produces very broad ranging results when used as a search term due to its wide range of meanings, including lay meanings. The so-called comprehensive pearl growing method [12] is a technique used to ensure all relevant articles are included, particularly in case of issues with vocabulary in a search strategy. This method is particularly useful in interdisciplinary research and where recent developments are expected in the literature. The process of pearl growing commences with the identification of ‘key pearls’ (i.e. key studies), that can be identified from within the literature as being compatible with the aim of the review [12]. Once the key pearls have been identified, these are used to generate the ‘first wave of pearls’, that is, papers that have cited the key pearls within their reference list. It has been used successfully in a different type of review in the context of capabilities [13]. This second approach was implemented to validate the strategy applied during the systematic search and to identify potential further papers.
Two waves of the pearl growing method were conducted: one focusing on the development of instruments and a second wave related to the application of the instruments. A third wave was deemed unnecessary because the identified last generation of seminal papers were published only recently and have not been cited yet. The results are presented in Table 1. The first wave used for citation searching were the developmental studies of the four most commonly used and reported capability instruments: ASCOT, ICECAP-O, its version for adults (ICECAP-A) and the Oxford CAPabilities questionnaire-Mental Health (OxCAP-MH). The second wave relied on the three main papers from the last 5 years (but already with some relevant citations) that aimed to identify recent developments and up-to-date knowledge in the application of the capability approach in health economic evaluations. The number of citations was retrieved from Scopus on 14 March 2019.
Table 1.
Key pearls for the two waves of the comprehensive pearl growing method
| Wave | Study | Number of citations | Short description |
|---|---|---|---|
| Wave 1 | [52] | 92 | Development of the ASCOT |
| [53] | 146 | Development of the ICECAP-A | |
| [54] | 158 | Development of the ICECAP-O | |
| [39] | 66 | Development of the OxCAP-MH | |
| Wave 2 | [48] | 27 | Description of new methods to conduct economic evaluations using the capability approach |
| [55] | 13 | Presents the opportunities and challenges of the capability approach in health economics | |
| [49] | 4 | Critical review of relevant questionnaires to measure and value capability |
Study selection
Titles and abstracts were sifted by two researchers (TL and AL) and studies were included for further assessment if they met the following inclusion criteria: (1) Full paper available in English or German languages. (2) Scope of study is the area of health or health-related interventions, including any interventions specifically targeting the promotion of health and prevention and treatment of ill-health irrespective of the sector where these were implemented. Hence, our study also included potentially relevant studies from the social care and public health sectors. (3) Focus of research is the evaluation or assessment of the outcomes of interventions using the capability approach. (4) Paper includes information on the use (or recommended use) of the capability approach in economic evaluations. (5) Paper is an applied evaluation OR focuses on the development, psychometric validation (or comparison to other tools) or preference valuation of instruments.
The full paper was retrieved if a study met the inclusion criteria based on its title and abstract. Consequently, full papers were assessed by two researchers (TH and AL) for inclusion based on their contribution to at least one of the aims of this literature review and subsequently allocated to the categories of either (i) applied evaluations (using a capability instrument in a completed economic evaluation) or (ii, iii, iv, v) methods papers. Methods papers were further categorised based on their relevance to the identification, measurement and valuation of outcomes, as well as the practical application of tools and theoretical contributions. Papers were grouped into categories of (ii) instrument development, (iii) psychometric validation or quantitative comparison of instruments, (iv) preference valuation of instruments and (v) methods for incorporation of the capability approach in economic evaluations. The latter one includes potential fields of application, approaches to use the results, incorporation of the results into a potential framework, for instance, Capability-Adjusted Life Years (CALYs), years of full capability or years of sufficient capability equivalence, etc. Some of the studies with significant theoretical contributions to the application of the capability approach in health economic evaluations which did not fit the above criteria were noted for discussion.
No specific quality assessment was applied, all studies which provided information on either the psychometric properties or use of capabilities instruments in economic evaluations were included. The instruments were assessed based on their psychometric properties according to the COSMIN checklist [15], feasibility [16], potential for transferability and evidence regarding valuation.
Data extraction and analysis
Separate data extraction forms were created for empirical and psychometric evaluation (and other methods) studies. The search for information on valuation included any kind of preference-based valuation of instruments (or their dimensions/domains) and the existence of value sets. Further information on data extraction is presented in Appendix 2.
Trends in the literature were analysed based on the number of different types of studies published each year. The information elicited from the studies was structured according to the capability instrument in question. Information about economic evaluations, and the psychometric properties and correlation coefficients from studies comparing instruments are presented in review tables. Due to the variability of methods used in the validation and comparison studies, only narrative synthesis, including tabulation and frequency analyses, was conducted as no statistical pooling was possible. The information gathered was synthesised in a qualitative rather than quantitative manner by TH.
Results
Search results
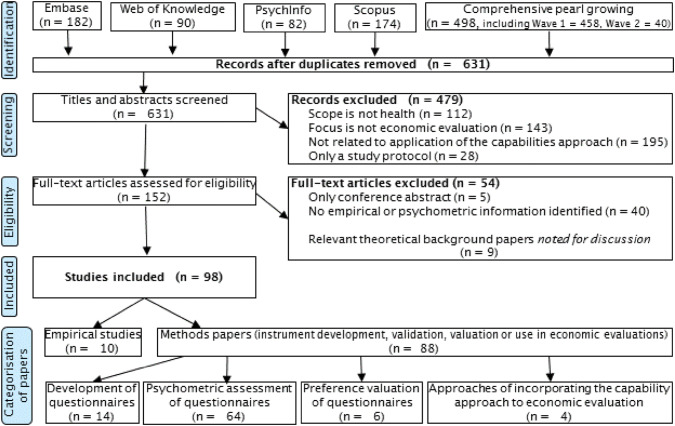
The literature search identified 98 studies for inclusion (Appendix 4 provides a complete list). The pearl growing method identified 29 citations beyond those captured by the systematic search strategy. However, none of the additional references met the inclusion criteria, and the papers included in this review were actually all picked up by the systematic search. An overview of the literature search based on the PRISMA statement is presented in Fig. 1.
Fig. 1.
PRISMA chart
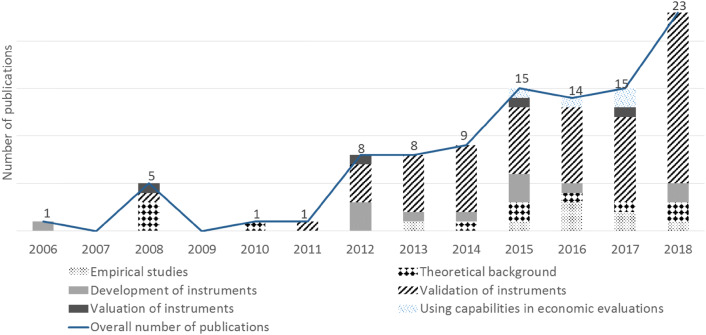
The increasing number of relevant publications in recent years is a clear trend (shown in Fig. 2). A further trend also appears to be a shift from developmental studies towards the validation of capability instruments and their use in empirical studies.
Fig. 2.
Annual changes in the number and type of publications related to using the capability approach in the economic evaluation of health-related interventions. Year 2019 not included in this figure because data were not available for the full year. Instruments to assess capability
Instruments to assess capability
Development of instruments
The literature review identified 14 capability instruments. Table 2 shows the heterogeneity of the capability instruments in terms of development methods, disease areas, types of interventions, population groups and the questionnaire structure.
Table 2.
Overview of the main characteristics and development methods of instruments that measure and value capability for economic evaluations in health
| Instrument | Instrument full name | Field | Population | Number of | Development method | Informants | Number of informants | References | |
|---|---|---|---|---|---|---|---|---|---|
| Dimensions | Levels | ||||||||
| ACQ‐CMH‐104 | Achieved Capabilities Questionnaire for Community Mental Health | Mental health | Patients | 104 | Unknown | Focus groups | Participants of Portuguese community mental health services | 50 | [56] |
| ASCOT | Adult Social Care Outcomes Toolkit | Social care | Patients | 8 | 4 | Delphi exercise, Literature review and expert opinion, Further improvement of the Older People’s Utility Scale (OPUS) | Experts and service users | 330 | [52] |
| ASCOT Easy Read version | Easy Read Version of the Adult Social Care Outcomes Toolkit | Social care | People w. intellectual disabilities | 8 | 4 | Focus groups and in-depth interviews | Intellectual disability or autism | 54 | [57] |
| ASCOT – proxy version | Proxy-report version of the Adult Social Care Outcomes Toolkit | Social care | Patients | 8 | 4 | In-depth qualitative interviews | Adult care workers or unpaid family carers of patients with cognitive and/or communication impairments | 25 | [58] |
| ASCOT-Carer | Carer Version of Adult Social Care Outcomes Toolkit | Social care | Carers | 7 | 4 | Literature review and feedback from service users, carers, practitioners and policy-makers | Service users, carers, practitioners and policy-makers | 31 | [59] |
| CAF | Currently Achieved Functioning | General | Older people | 5 | 5 | In-depth qualitative interviews | Older people living in 3 Dutch urban areas | 99 | [60] |
| ICECAP-A | ICEpop CAPability measure for Adults | General | General public | 5 | 4 | In-depth, informant-led, interviews | General public (purposively selected through a random electoral sample) | 36 | [53] |
| ICECAP-CPM | ICEpop CAPability Close Person Measure | End of life | Close persons | 6 | 5 | In-depth qualitative interviews | Bereaved within the last 2 years or with a close person currently receiving end-of-life care | 27 | [61] |
| ICECAP-O | ICEpop CAPability measure for Older people | General | Older people | 5 | 4 | In-depth qualitative interviews | Purposively selected informants aged 65 and over in private households | 40 | [54] |
| ICECAP-SCM | ICEpop CAPability Supportive Care Measure | End of life | Patients | 7 | 4 | In-depth qualitative interviews | Older people from different groups across the dying trajectory | 23 | [62] |
| OCAP-18 | OCAP-18 | Public health | General public | 18 | Unknown |
Theoretical framework, Focus groups and in-depth interviews |
Purposively sampled from various community groups in Glasgow, United Kingdom | 40 | [63] |
| OxCAP-MH | Oxford Capabilities Questionnaire for Mental Health | Mental health | Patients | 16 | 5 |
Theoretical framework, Focus group discussions |
Psychiatrists, Psychologists, Social scientists, Health economists | 336 | [39] |
| (Low-income questionnaire) | (Low-income questionnaire) | Low-income settings | General public | 6 | Unknown | Focus groups | Women in rural Malawi | 129 | [64] |
| (Chronic pain questionnaire) | (Chronic pain questionnaire) | Chronic pain | Patients | 8 | Unknown | Focus groups and in-depth interviews | Respondents were recruited through a Pain Management Clinic in the East of England | 16 | [65] |
Availability of evidence on the characteristics of capability instruments
As Table 3 demonstrates, there is at least some evidence about the psychometric properties of most instruments.
Table 3.
Availability of evidence on the characteristics of capability instruments for health economic evaluations
| Instrument | Reliability | Validity | Responsiveness | Interpretability/Feasibility | Valuation |
|---|---|---|---|---|---|
| ACQ‐CMH‐104 | [66] | [66] | Unknown | Unknown | Unknown |
| ASCOT | [67] | [21, 68, 69, 70, 71, 72, 73, 74] | [71] | [75] | [52] |
| ASCOT easy read | Unknown | Unknown | Unknown | [57] | Unknown |
| ASCOT-proxy | Unknown | Unknown | Unknown | [58] | Unknown |
| ASCOT-carer | [76] | [76] | Unknown | Unknown | Unknown |
| CAF | Unknown | Unknown | Unknown | [60] | Unknown |
| ICECAP-A | [77] | [20, 23, 24, 27, 33, 34, 38, 78, 79, 80] | [23, 32, 33, 34, 37, 81] | [82, 83, 84] | [85] |
| ICECAP-CPM | Unknown | Unknown | Unknown | Unknown | Unknown |
| ICECAP-O | [30, 86, 87] | [18, 21, 22, 25, 26, 40, 74, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96] | [26, 31, 35, 36, 95, 97] | [25, 26, 30, 40, 89, 91, 98, 99] | [88] |
| ICECAP-SCM | Unknown | Unknown | Unknown | [29, 83] | [100, 101] |
| low-income Q | Unknown | [102] | Unknown | Unknown | Unknown |
| pain Q | Unknown | Unknown | Unknown | Unknown | Unknown |
| OCAP-18 | Unknown | Unknown | Unknown | Unknown | Unknown |
| OxCAP-MH | [17, 19, 103] | [17, 19, 103] | [17] | [39] | Unknown |
The most recently developed instruments, unsurprisingly, have less information available about their reliability, validity and responsiveness; an exception is OCAP-18 which was among the first capability instruments to be developed, but for which there is no further psychometric evidence available. The main difference across different groups of capability instruments is whether valuations that reflect the preferences of patients or the general public are available. The ASCOT and most ICECAP instruments have reported valuation studies and are therefore considered to possess evidence regarding their ability to reflect values of informants, whilst this is currently missing, for instance, for OxCAP-MH.
Different language versions of instruments
Apart from ACQ‐CMH‐104, all instruments were originally developed in English. The ASCOT, ICECAP-A, ICECAP-O and OxCAP-MH instruments have been translated to further languages, and these new versions have been validated (Table 4).
Table 4.
Availability of different language versions of capability instruments
| Instrument | Availability of language versions beside Englisha |
|---|---|
| ACQ‐CMH‐104 | Only available in Portuguese language |
| ASCOT | Japanese [105]; Dutch [106] |
| ASCOT easy read | None identified |
| ASCOT-proxy | None identified |
| ASCOT-carer | None identified |
| CAF | None identified |
| ICECAP-A | Chinese [107], Danish (unpublished), Dutch (unpublished), German [107], Italian (unpublished), Persian (unpublished), Welsh (unpublished) |
| ICECAP-CPM | none identified |
| ICECAP-O | Chinese (unpublished), Dutch [92], French (unpublished), German [18], Spanish [87], Swedish [86], Welsh (unpublished); Italian, Norwegian and Portuguese [109] |
| ICECAP-SCM | None identified |
| low-income Q | None identified |
| pain Q | None identified |
| OCAP-18 | None identified |
| OxCAP-MH | German [103] |
aInformation on unpublished translations of instruments stem from the dedicated websites of the instruments
Validation of capability instruments
Reliability
The test–retest reliability of most instruments have been successfully assessed in some groups of population, e.g. ACQ‐CMH‐104 [56]; ASCOT [72]; ICECAP-A [77]; ICECAP-O [86]; OxCAP-MH [19].
Validity
There were 25 studies among the included papers that used Pearson’s or Spearman rank correlation coefficients to quantitatively assess the validity of all language versions of the capability instruments and/or compare it to other instruments. Quantitative evidence was provided on the validity of six capability instruments, including ACQ‐CMH‐104, ASCOT, ICECAP-A, ICECAP-O, OxCAP-MH and Women’s Capabilities Index. Table 5 (and Appendix 5) summarise the correlations.
Table 5.
Construct validity of capability instruments for health economic evaluations
| Capabilities instrument | Compared with… (full names in Appendix 5) | Value of correlation* | Population (country in Appendix 5) | Number of informants | References |
|---|---|---|---|---|---|
| ACQ‐CMH‐104 | RAS | 0.46* | Psychiatric patients | 92 | [66] |
| WHOQOL‐Bref | 0.60* | Psychiatric patients | 129 | [66] | |
| ASCOT | Barthel Index | 0.45 | Older social care users | 205 | [21] |
| Cantril’s Ladder | 0.66 | Older social care users | 205 | [21] | |
| CASP-12 | 0.58 | Older home care residents | 301 | [52] | |
| EQ-5D-3L | 0.41 | Older home care residents | 301 | [52] | |
| EQ-5D-3L | 0.40 | Older home care residents | 301 | [70] | |
| EQ-5D-3L | 0.47 | Older home care residents | 224 | [68] | |
| EQ-5D-3L | 0.41* | Frail older adults living at home | 190 | [74] | |
| EQ-5D-3L | 0.37 | Older social care users | 748 | [72] | |
| EQ-5D-5L | 0.63 | Older social care users | 205 | [21] | |
| EQ-5D-5L | 0.24 | Older adults in a day rehabilitation facility | 22 | [71] | |
| EQ-5D-VAS | 0.64 | Older social care users | 205 | [21] | |
| GDS-15 | − 0.69 | Older social care users | 205 | [21] | |
| GHQ-12 | − 0.58 | Older home care residents | 301 | [52] | |
| ICECAP-A | 0.62 | Older social care users | 748 | [72] | |
| ICECAP-O | 0.81 | Older social care users | 205 | [21] | |
| ICECAP-O | 0.41* | Frail older adults living at home | 190 | [74] | |
| ICECAP-O | 0.67 | Older social care users | 748 | [72] | |
| OPQOL-13 | 0.76 | Older social care users | 205 | [21] | |
| OPQOL-brief | 0.38 | Older adults in a day rehabilitation facility | 22 | [71] | |
| OPQoL-Brief | 0.58 | Older social care users | 87 | [69] | |
| SWLS | 0.74 | Older social care users | 205 | [21] | |
| ASCOT-Carer | CES | 0.58 | Social care recipients | 376 | [76] |
| CSI | − 0.59 | Social care recipients | 384 | [76] | |
| EQ-5D-3L | 0.34 | Social care recipients | 382 | [76] | |
| QoL | 0.62 | Social care recipients | 384 | [76] | |
| ICECAP-A | 15D | 0.50* | Healthy general public and patients from 8 disease areas | 6756 | [24] |
| AQoL-8D | 0.31* | Healthy general public and patients from 8 disease areas | 6756 | [24] | |
| AQoL-8D | 0.80 | Healthy general public and patients with 7 chronic conditions | 8022 | [20] | |
| EQ-5D-3L | 0.53 | Women with lower urinary tract infection | 478 | [23] | |
| EQ-5D-3L | 0.49 | Knee pain patients in primary care | 500 | [27] | |
| EQ-5D-5L | 0.62* | Healthy general public and patients with 7 chronic conditions | 1212 | [108] | |
| EQ-5D-5L | 0.49* | Healthy general public and patients from 8 disease areas | 6756 | [24] | |
| EQ-5D-5L | 0.60 | Healthy general public and patients with 7 chronic conditions | 8022 | [20] | |
| HUI-3 | 0.32* | Healthy general public and patients from 8 disease areas | 6756 | [24] | |
| LDQ | − 0.48 | Opiate substitution recipients | 83 | [34] | |
| SF-6D | 0.64* | Healthy general public and patients with 7 chronic conditions | 1212 | [108] | |
| SF-6D | 0.47* | Healthy general public and patients from 8 disease areas | 6756 | [24] | |
| SSQ | 0.43 | Opiate substitution recipients | 83 | [34] | |
| SWLS | 0.66* | Healthy general public and patients with 7 chronic conditions | 1212 | [108] | |
| ICECAP-O | ADRQL | 0.53* | Nursing home residents with dementia | 95 | [18] |
| Barthel Index | 0.49 | Older social care users | 209 | [21] | |
| Barthel Index | 0.72* | Nursing home residents with dementia | 95 | [18] | |
| Cantril’s Ladder | 0.74 | Older social care users | 213 | [21] | |
| CTM-3 | 0.23 | Patients from outpatient day rehabilitation unit | 82 | [22] | |
| EQ-5D-3L | 0.34 | Older people with hip fracture | 113 | [95] | |
| EQ-5D-3L | 0.69* | Nursing home residents with dementia | 95 | [18] | |
| EQ-5D-3L | 0.53 | Older people after hip fracture surgery | 87 | [93] | |
| EQ-5D-3L | 0.44 | Patients from outpatient day rehabilitation unit | 80 | [22] | |
| EQ-5D-3L | 0.47 | Patients visiting the clinic | 215 | [25] | |
| EQ-5D-3L | 0.63 | Frail older adults living at home | 190 | [74] | |
| EQ-5D-5L | 0.68 | Older social care users | 207 | [21] | |
| EQ-5D-5L | 0.63 | General population aged 70 or older | 516 | [90] | |
| EQ-5D-VAS | 0.66 | Older social care users | 208 | [21] | |
| GDS-15 | − 0.73 | Older social care users | 210 | [21] | |
| OHS | 0.38 | Older people with hip fracture | 113 | [95] | |
| OPQOL-13 | 0.80 | Older social care users | 211 | [21] | |
| SWLS | 0.82 | Older social care users | 212 | [21] | |
| ICECAP-O family version | EQ-5D family version | 0.57* | Nursing professionals of psycho-geriatric elderly | 96 | [92] |
| EQ-VAS family version | 0.43* | Family members of psycho-geriatric elderly | 68 | [92] | |
| ICECAP-O nursing version | EQ-5D nursing version | 0.48* | Nursing professionals of psycho-geriatric elderly | 96 | [92] |
| EQ-VAS nursing version | 0.55* | Family members of psycho-geriatric elderly | 68 | [92] | |
| OxCAP-MH | BPRS | − 0.41 | Patients with psychosis | 172 | [19] |
| BSI-18 | − 0.67* | Patients in socio-psychiatric services | 162 | [17] | |
| EQ-5D VAS | 0.58* | Patients in socio-psychiatric services | 161 | [17] | |
| EQ-5D-3L | 0.45 | Patients with psychosis | 172 | [19] | |
| EQ-5D-5L | 0.66* | Patients in socio-psychiatric services | 160 | [17] | |
| EQ-5D-VAS | 0.52 | Patients with psychosis | 172 | [19] | |
| GAF | 0.24 | Patients with psychosis | 172 | [19] | |
| GAF | 0.35* | Patients in socio-psychiatric services | 168 | [17] | |
| Mini-ICF-APP | − 0.47* | Patients in socio-psychiatric services | 167 | [17] | |
| SIX | 0.12 | Patients with psychosis | 172 | [19] | |
| WHOQOL-Bref Environment | 0.69* | Patients in socio-psychiatric services | 166 | [17] | |
| WHOQOL-BREF Physical health | 0.69* | Patients in socio-psychiatric services | 163 | [17] | |
| WHOQOL-Bref Psychological | 0.75* | Patients in socio-psychiatric services | 164 | [17] | |
| WHOQOL-Bref Social relationships | 0.50 | Patients in socio-psychiatric services | 165 | [17] | |
| Women’s Capabilities Index | WHOQOL-Bref | 0.62* | Women from Malawi | 20 | [64] |
Values in italic are Pearson’s coefficients, values in standard writing are Spearman rank correlations. A * behind the value means that the study used a non-English version of the capability instrument
There is variation between studies in the correlation measures used, the instruments compared, the characteristics of the population, number of informants, testing of hypotheses generated regarding likely associations between the data and testing across known groups for discriminant and convergent validity. Hence, it is difficult to provide general statements about the comparison of capability instruments with other PROMs, or to conduct statistical pooling of the results. High correlation estimates (above 0.8) were found between capability instruments: ASCOT/ICECAP-O [49] and ICECAP-A/AQoL-8D [20].
The examined studies provided very diverse estimates for the correlations between Health-related Quality of Life (HRQoL) and the different capability instruments. Most studies compared the ASCOT, ICECAP-A and ICECAP-O instruments with either disease-specific or generic HRQoL instruments. A wide range of disease-specific instruments were applied across studies, mainly being used when informants consisted of patients and social care recipients. EQ-5D-3L/-5L was used in 92% (n = 23) of the included validation and comparison studies as a HRQoL measure. In most cases, the 5L version of the EQ-5D instruments provided higher correlation coefficients compared to the 3L version. The higher correlation with capability instruments could be explained by lower ceiling effects and higher sensitivity to minor changes in the 5L version compared to the 3L version.
There seem to be a consensus in the literature that the capability approach provides complementary information to HRQoL measures. However, capability instruments could also be perceived as enhanced rather than complementary to the narrow interpretation of well-being/quality of life when focusing only on HRQoL. Most studies [25–27] found that the ICECAP and EQ-5D instruments provide complementary information, and a mapping is not recommended between them. Engel et al. [24] found that the ICECAP-A provides evidence above that gathered from most commonly used preference-based HRQoL instruments. Similar findings were reported for other capability instruments. Forder and Caiels [68] found that ASCOT has greater validity in measuring the effects of social care services than EQ-5D. Van Leeuwen et al. [28] investigated the validity of ICECAP-O and ASCOT among Dutch older adults. Although it could be attributable to cultural transferability issues, they found that respondents did not feel that these instruments give a comprehensive picture of their HRQoL because they did not find all domains of the instruments relevant, whilst other important domains were not covered, particularly concerns or delight about the well-being of family members. HRQoL instruments capture an important part of broader well-being, and some studies [22, 23] established strong and positive association between capability and HRQoL instruments, which questions whether they focus on complementary constructs. Evidence suggests that some capability instruments could rather be interpreted as an enhancement of the HRQoL concept, for instance, an exploratory factor analysis [17] found that all EQ-5D-5L items and seven OxCAP-MH items loaded on one factor and nine remaining OxCAP-MH items loaded on a separate factor.
It is questionable whether the issues discussed above relate to all HRQoL measures or only the EQ-5D Utility instrument. Lower correlation between the OxCAP-MH and EQ-5D Utility scores was observed in the Vergunst et al. [19] study than between OxCAP-MH and EQ-5D-VAS. This could be explained by the fact that the latter reflects the patient’s overall judgement about their health status rather than focusing only five dimensions of their health, which is arguably more in line with the underlying broader well-being concept and the used non-preference-based index score of the OxCAP-MH instrument.
Interpretability
In terms of ease of understanding, Bailey et al. [29] investigated the appropriateness of ICECAP-SCM to measure QoL and found that the capability instrument appeared more meaningful, easier to complete and had fewer errors among patients and close persons, compared to EQ-5D-5L. However, these results did not apply to healthcare professionals who preferred the EQ-5D-5L over ICECAP-SCM when measuring clinician-rated health states because it focused on observable attributes. Similar studies have also demonstrated the feasibility of use of other ICECAP measures [81, 90]. Malley et al. [70] and Towers et al. [67] demonstrated the feasibility of using ASCOT among older people and care home residents; however, the study also highlighted the need for proxy respondents in some situations. This later led to the development of a proxy version of the ASCOT, which demonstrated good feasibility [58]. Davis et al. [30] reported that the level of agreement between patient and proxy for the EQ-5D-3L was significantly better than the level of agreement observed for the ICECAP-O in case of patients with vascular cognitive impairment. The authors conclude that due to its complexity, the ICECAP-O may have limited clinical, research and policy-related utility among individuals with mild cognitive impairment. However, these results need to be interpreted carefully due to the differing number of levels and the greater ability of proxies to observe the dimensions in EQ-5D. Although it could be explained by translational issues, van Leeuwen [28] who also reported difficulties with understanding the ASCOT and ICECAP-O in a study assessing a small number (n = 10) of Dutch, community-dwelling frail older adults. Simon et al. [39] explored the feasibility of OxCAP-MH among severely ill mental health service users. Patients provided positive feedback and felt that the questions allowed them to express their views and experience on topics they considered important but which were often left out of clinical or research interviews [39].
Responsiveness
The sensitivity of the capability instruments to measure changes is generally reported to be higher than in case of HRQoL measures [6, 17, 31–34]. However, some authors found capability instruments to be less responsive than HRQoL measures. Davis et al. [35] and Couzner et al. [36] reported that the difference in values between the patient and general population groups was found to be far more pronounced for the EQ-5D-3L than for the ICECAP-O. There is a consensus in the literature that changes related to the broader meaning of health are better captured by the capability instruments than by EQ-5D [37–39]. Coast et al. [40] found strong evidence of association of general health with all capability attributes except for the attachment domain of ICECAP-A. Laszewska et al. [17] found that the OxCAP-MH may be seen as enhanced rather than complementary in its concept, when compared to EQ-5D-5L.
Valuation of instruments
From the reviewed 14 capability instruments, only four have a published valuation set. These used the best–worst scaling method, most often relying on the MaxDiff model. Informants mainly came from the general public. There is no published evidence available for the valuation of the remaining ten capability questionnaires (Table 6).
Table 6.
Valuation of capability instruments for health economic evaluations
| Instrument | Methods of valuation | Number of choices per BWS task | Number of BWS tasks per respondents | Population | Number of informants | References |
|---|---|---|---|---|---|---|
| ASCOT | BWS, TTO | 4 | 8 | General public | 958 (BWS) + 126 (TTO) | [52] |
| ICECAP-A | BWS | 5 | 16 | General public | 413 | [85] |
| ICECAP-O | Variants of DCEs and BWS tasks (online) | 5 | 16 | General public aged 65 or over | 255 | [88] |
| ICECAP-SCM | BWS | 7 | 16 | General public | 6020 | [101, 110] |
Applied economic evaluations and potential methods to incorporate the capability approach
Ten applied evaluations were identified in this review that have used a capability-based instrument as secondary outcome measure in health economic evaluations. No economic evaluation was found where a capability instrument was used as a primary measure of health outcomes. The information extracted from the applied evaluations is presented in Table 7 and in Appendix 6.
Table 7.
Applied evaluations using the capability approach in their economic evaluations
| Capability measure | Disease | Time points | Other HE measures | Changes in QALYs vs. capability values | Presentation of results | Reference |
|---|---|---|---|---|---|---|
| ICECAP-A | Visual impairment | Baseline; 2–4 months | EQ-5D-5L | Nearly identicala | Cost per Year of Full Capability (YFC) | [111] |
| Diabetic plantar ulceration | Baseline; 6 months | EQ-5D-5L | QALYs negative; Capability positive | Cost and outcome data presented separately | [43] | |
| Drug addiction | Baseline; 12 months | EQ-5D-5L | Full capability higher than Sufficient capability, and both higher than QALYs | Years of full capability (YFC), years of sufficient capability equivalent (YSC) | [112] | |
| Schizophrenia | Baseline; 12–36–48 weeks | EQ-5D-3L | Nearly identicala | Cost and outcome data presented separately | [44] | |
| ICECAP-O | Health decline in the older people | Baseline; 3 months | EQ-5D-3L | QALYs positive; Capability negative | Incremental net monetary benefit (INMB) regressions based on capability QALYs | [31] |
| Heart failure, chronic obstructive pulmonary disease, or diabetes | Baseline; 12 months | EQ-5D-3L | Nearly identicala | Willingness to pay for 100% improvement in capability | [113] | |
| Visual impairment | 3 months; post-intervention; pre-study | EQ-5D-5L | Capability higher than QALYs | Costs per years of well-being | [46] | |
| Hip fracture | Baseline; 3 months | EQ-5D-3L | Capability lower than QALYs | Cost and outcome data presented separately | [42] | |
| OxCAP-MH | Psychosis | Baseline; 6–12 months | EQ-5D-3L | Nearly identicala | Cost and outcome data presented separately | [45] |
| ICECAP-A and OxCAP-MH | Schizophrenia or schizoaffective disorder and depression | Baseline, 3–6–9 months | EQ-5D-5L | QALYs positive; Capability: no significant change | Cost and outcome data presented separately | [114] |
aNearly identical means that the difference between baseline and follow-up are within a 10% range when comparing the QALYs and capability estimates
The number of economic evaluations reporting the use of a capability instrument has increased in recent years and further increases can be expected given that this search identified a number of recent study protocols (e.g. [41, 42, 114]). Four further studies were identified that specifically addressed the issues and discussed considerations when incorporating the capability approach into health-related economic evaluations.
A recent review [13] focused on using the capability approach in health research, not limited to economic evaluations. It identified four distinct common areas of application including: (1) physical activity and diet; (2) patient empowerment; (3) multidimensional poverty and (4) assessments of health and social care interventions. The authors also noted that there is a noticeable non-reliance on health status as a sole indicator of capability in health, and differences were found across studies in approaches to applying mixed methods, selecting capability dimensions and weighting capabilities. The current review identified applied economic evaluations from areas with widely accepted issues related to outcomes beyond the QALYs framework, e.g. mental health, visual impairment, chronic diseases and health decline in older people.
The presentation of results in the included economic evaluations demonstrate that there is a lack of consensus regarding the most appropriate way to use capability instruments in economic evaluations. Some authors present cost and outcome data separately and conduct a cost-consequence analysis [42–45], whilst others reported the results following the idea behind the incremental cost-effectiveness ratio (ICER) [31, 46]. This lack of consensus about the use of capability instruments in decision making relates to the different approaches taken by different research groups to valuation, which means that in practice these measures are not comparable along the lines of a QALY. The idea of CALYs has been proposed by Mansdotter et al. [47] who highlights the following issues. First, it is questionable which capabilities are able to explain differences in well-being and are sensitive to public policies in high-income countries. Second, questions of the relevant instruments should capture voluntary and involuntary positions because an applied conceptualization of the capability approach includes opportunity as well as achievement. Third, methods for weighting capability and threshold values should be established, similar to QALYs. Finally, a trade-off should be made between the maximisation of capability and equity.
Mitchell et al. [48] proposed the concept of years of sufficient capability which is more closely aligned to the theory underpinning the capability approach because it has a greater focus on those in capability poverty. The process of defining a threshold for sufficient capability should be based on generating a sufficient capability score and using these scores to produce a capability outcome over time [48]. The use of ICECAP-A in the economic evaluations included in this literature review seem to focus on the choice between the options of years of full capability vs. years of sufficient capability equivalent [48].
The current state of the art identified in the reported economic evaluations applying the capability approach to their assessment are in line with the previously identified main challenges [50], including the need to research what the value of a capability improvement is, how to use the instruments globally, and compare the sensitivity of each measure to different patient groups and conditions. Only one study [49] was identified that posed a critique to using the capability approach in health economic evaluations. The authors claim that the method used in the questionnaires to measure capability will result in a capability set that is an inaccurate description of the individual’s true capability set. The measured capability set will either represent only one combination and ignore the value of choice in the capability set, or represent one combination that is not actually achievable by the individual. In addition, existing methods of valuing capability may be inadequate because they do not consider that capability is a set. (Although the Oxford instruments were developed based on Nussbaum’s 10 basic human capabilities.) Hence, it may be practically more feasible to measure and value capability approximately rather than directly. Nevertheless, the argument is based on the questionable assumption that all capabilities have to be traded against other capabilities.
Discussion
This systematic literature review about capability instruments in economic evaluations of health-related interventions included 98 articles and identified 14 capability-based instruments. It provides a unique, comprehensive synthesis of the relevant evidence by focusing on the full spectrum of potentially available capability measures and summarising the practical and theoretical aspects of use of these instruments in economic evaluations. Most identified information related to the ASCOT, ICECAP-A, ICECAP-O and OxCAP-MH instruments.
The development of capability instruments relies on methods similar to those applied in the case of HRQoL measures. Capability instruments were often compared to EQ-5D, but less often to each other. Possible reasons for this are that some instruments are population or disease-specific, and that the inclusion of two instruments measuring the same concept in an applied evaluation study is assumed to unnecessarily increase participants’ completion burden. In general, the information identified in the literature regarding the comparison of capability measures with other instruments could not be used for a pooled analysis. This is mainly due to the vast variation in the correlation measures used, the instruments compared, the characteristics of the populations and the number of informants. Despite the diverse quantitative estimates for the correlations with EQ-5D, the different capability instruments and the limited available data, this review confirms that capability measures capture a wider range of outcomes than the EQ-5D and may be more responsive when an intervention is likely to have broad impacts on HRQoL. Following the guidelines [51] to evaluate the strength of correlations, this generally observed moderate-to-high correlation suggests that EQ-5D and capability instruments measure somewhat similar, yet complementary concepts. However, there are competing statements in the literature regarding the association between capability and HRQoL instruments. Most authors argue that these measures complement each other; however, some studies suggest that capability instruments could be perceived as enhancements of the HRQoL concept. It is possible that this relationship depends on the choice of both capability and health instruments used in these comparisons. For instance, the OxCAP-MH has a relatively high number of items, which potentially capture a broader range of capability concepts than measures such as the ICECAP measures. Similarly, the EQ-5D measure of health has a narrower focus than other health measures such as measures based on SF-36 or the AQoL. The higher correlations between capability instruments and the EQ-5D-VAS scores than those observed between capability instruments and the EQ-5D utility scores suggest that respondents’ overall judgement of their health status on a VAS seems to reflect better broader quality-of-life concepts present in the capability approach than specific scores for a certain limited number of HRQoL dimensions. Moreover, the differences in correlations found between measures may be due to differences in the populations studied. Hence, further research could explore which population subgroups and disease areas could benefit from the inclusion of certain capability instruments in economic evaluations.
Three of the identified 14 capability instruments were used in applied economic evaluation of interventions in the health and social care field; however, only as secondary outcome measures. Eight of the identified ten applied economic evaluations were conducted in the United Kingdom. This may be the result of the fact that the measures were developed in the UK and only available in English for some years. From the perspective of (health) economists concerned with economic evaluations, a good outcome measure should possess three main characteristics [2]. First, it should be comparable among diseases and interventions to allow for interpretation in a comparative way for resource allocation purposes. The capability instruments identified in this literature review were developed for specific population groups; hence, a comparison is currently challenging without a standard application of, for instance, the CALYs framework. Second, the instruments should have a scale with interval properties. All instruments provide a summary score; however, only a few are anchored and therefore have interval properties. The ICECAP scores are anchored on no capability and full capability, and the ASCOT scales are anchored on death and full capability. Finally, most economists are looking for an outcome measure for economic evaluation that reflects preferences, either of individual patients or the general public. Instruments with tariffs derived from the general population (ASCOT, ICECAP-A and ICECAP-SCM) or the relevant subpopulation (ICECAP-O) possess this characteristic. On the other hand, reducing capabilities information only to a single, preference-based index value on a scale of 0–1 may limit the actionable policy relevance of the information [39]. The two approaches, however, are not mutually exclusive and more research is needed about the relative values of different capabilities and their variance according to population specifics (e.g. age, disease experience, culture). More information about the weights people allocate to the attributes and levels of capability instruments would be needed to improve our understanding of the relative value of individual capability domains and dimensions.
Major limitations of this study design include that the search was limited to English and German. Next, this review only assessed instruments and studies reported in the literature, and a thorough grey literature search could not be conducted due to difficulties with the search term capability. In terms of grey literature, only dedicated websites of capability instruments were reviewed for relevant information. This resulted in some limitations, for instance, some cost-effectiveness components of studies that have used ASCOT have not been written up as journal articles and fell therefore outside the findings of this review [118, 119]. Furthermore, ongoing research and developments could not be included which could be important in such a dynamically moving area. For example, we found information about ongoing economic evaluations [41, 42, 114] with the identified instruments where results expected to be published soon, additional capability instruments might have been used in unpublished economic evaluations, or some are currently under development. There is a potential need to update this literature review in the future to gather information from this rapidly growing body of literature about the potential development of additional capability measures, the further validation of existing ones, the empirical use of capability measures in economic evaluations, and the lessons learned from these applications.
Conclusion
There has been an increasing interest in the application of the capability-based approach in economic evaluations of health-related interventions. Different instruments are available and the choice between them should be based on both the research question and the characteristics of the instruments. Further research should focus on the comparison of the existing capability instruments and examining the correlation across capability measures. This would help future researchers in choosing the most suitable capability instrument for their study and provide further information for instrument developers.
Acknowledgements
Open access funding provided by Medical University of Vienna.
Appendix 1: search strategy
Embase and Medline via Embase.com
((‘economic evaluation’/exp OR ‘economic*’:ti,ab,kw OR ‘cost-effective*’:ti,ab,kw OR ‘cost-utility’:ti,ab,kw OR ‘cost-benefit’:ti,ab,kw) AND ((‘ascot’:ti,ab,kw OR ‘icecap’:ti,ab,kw OR ‘oxcap-mh’:ti,ab,kw) OR (capabilit* NEXT/2 (perspective OR approach)):ti,ab,kw)) AND (2000:py OR 2001:py OR 2002:py OR 2003:py OR 2004:py OR 2005:py OR 2006:py OR 2007:py OR 2008:py OR 2009:py OR 2010:py OR 2011:py OR 2012:py OR 2013:py OR 2014:py OR 2015:py OR 2016:py OR 2017:py OR 2018:py OR 2019:py) (182 results).
Web of science
TS = (“economic evaluation”) OR TI = (“economic evaluation”) OR TS = (“economic assessment”) OR TI = (“economic assessment”) OR TS = (cost-effectiveness) OR TI = (cost-effectiveness) OR TS = (cost-utility) OR TI = (cost-utility) OR TS = (cost-benefit) OR TI = (cost-benefit) AND TS = (“capabilit* approach”) OR TI = (“capabilit* approach”) OR TS = (“capabilit* perspective”) OR TI = (“capabilit* perspective”) OR TS = (ascot) OR TI = (ascot) OR TS = (icecap*) OR TI = (icecap*) OR TS = (oxcap-mh) OR TI = (oxcap-mh)
Limitations: Last 20 years
Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI (90 results)
Psychinfo
((capabilit* or ascot or oxcap-mh or icecap).ab. or (capabilit* or ascot or oxcap-mh or icecap).ti.) and ((cost-effectiveness or cost-utility or cost-benefit or economic evaluation or economic assessment).ti. or (cost-effectiveness or cost-utility or cost-benefit or economic evaluation or economic assessment).ab.)
Limitations: Last 20 years (82 results)
Scopus
TITLE-ABS-KEY ((“capabilit* approach”) OR (“capabilit* perspective”) OR (ascot) OR (oxcap-mh) OR (icecap)) AND TITLE-ABS-KEY ((economic AND evaluation) OR (economic AND assessment) OR cost-effectiveness OR cost-utility OR cost-benefit)
Limitations: English, German, last 20 years (174 results)
Appendix 2: data extraction
The final list of extracted data in case of applied papers included
First author,
Year of publication (1999, …, 2018),
Country of study, Disease area,
Type of intervention,
Population under investigation,
Aim of study (to assess cost-effectiveness, to …),
Type of economic evaluation (cost-minimisation analysis, cost-consequence analysis, cost-effectiveness analysis, cost-utility analysis, cost–benefit analysis, not applicable),
Perspective of study (healthcare service, societal, other),
Capability instrument used (multiple choice between: ICECAP-A, ICECAP-O, OxCAP-MH, ASCOT, Other),
Time points of measurement (pre-study, baseline, post-study, 1 month, …, 12 months, beyond 12 months),
Other instruments used,
Methods to address missing data,
Presentation of results, e.g. cost/CALYs, p value of capability instrument (less than 0.05, greater than 0.05), Comparison of results to QALYs (lower, nearly identical, higher),
Comparison of incremental cost-effectiveness ratios (difference in costs per extra year to gain well-being, expressed in EUR),
Use of capability data in economic modelling (yes, no),
Recommendation to apply capability in future economic evaluations (yes, no),
Further comments on the capability instrument.
Data extraction in case of methods papers included the
First author,
Year of publication (2009, …, 2018),
Type of study (Comparison of questionnaires; Development of questionnaires; Methods to incorporate CA to economic evaluation; Theoretical background of CA),
Aim of study,
Capability instrument in question (multiple choice between: ICECAP-A, ICECAP-O, OxCAP-MH, ASCOT, Other),
Recommendation to apply capability in future economic evaluations (yes, no),
Further comments on the capability instrument.
Appendix 3
See Table 8.
Table 8.
List of included papers
| Author | Year | References | Category | Instrument(s) |
|---|---|---|---|---|
| Al-Janabi | 2012 | [53] | Development | ICECAP-A |
| Al-Janabi | 2015 | [77] | Validation | ICECAP-A |
| Al-Janabi | 2013 | [33] | Validation | ICECAP-A |
| Al-Janabi | 2013 | [82] | Validation | ICECAP-A |
| Bailey | 2016 | [29] | Validation | ICECAP-SCM |
| Barnes | 2016 | [44] | Empirical | ICECAP-A |
| Baumgardt | 2018 | [103] | Validation | OxCAP-MH |
| Botes | 2018 | [60] | Development | CAF |
| Botes | 2018 | [115] | Validation | CAF |
| Bray | 2017 | [111] | Empirical | ICECAP-A |
| Burns | 2016 | [45] | Empirical | OxCAP-MH |
| Chen | 2018 | [20] | Validation | ICECAP-A |
| Coast | 2008 | [88] | Valuation | ICECAP-O |
| Coast | 2016 | [100] | Valuation | ICECAP-SCM |
| Coast | 2008 | [40] | Validation | ICECAP-O |
| Coast | 2018 | [83] | Validation | ICECAP-A, ICECAP-SCM |
| Comans | 2012 | [97] | Validation | ICECAP-O |
| Couzner | 2012 | [22] | Comparison | ICECAP-O |
| Couzner | 2013 | [36] | Validation | ICECAP-O |
| Davis | 2013 | [25] | Comparison | ICECAP-O |
| Davis | 2016 | [30] | Validation | ICECAP-O |
| Davis | 2017 | [35] | Validation | ICECAP-O |
| Engel | 2018 | [78] | Validation | ICECAP-A |
| Engel | 2018 | [79] | Validation | ICECAP-A |
| Engel | 2016 | [89] | Validation | ICECAP-O |
| Engel | 2017 | [24] | Comparison | ICECAP-A |
| Flynn | 2015 | [85] | Valuation | ICECAP-A |
| Forder | 2011 | [68] | Validation | ASCOT |
| Franklin | 2018 | [26] | Comparison | ICECAP-O |
| Goranitis | 2016 | [34] | Comparison | ICECAP-A |
| Goranitis | 2017 | [112] | Empirical | ICECAP-A |
| Goranitis | 2016 | [23] | Validation | ICECAP-A |
| Greco | 2018 | [102] | Validation | low-income Q |
| Greco | 2015 | [64] | Development | low-income Q |
| Grewal | 2006 | [54] | Development | ICECAP-O |
| Hackert | 2017 | [21] | Comparison | ASCOT, ICECAP-O |
| Hackert | 2019 | [90] | Validation | ICECAP-O |
| Handels | 2018 | [109] | Translation | ICECAP-O |
| Henderson | 2013 | [113] | Empirical | ICECAP-O |
| Horder | 2016 | [86] | Validation | ICECAP-O |
| Horwood | 2014 | [91] | Validation | ICECAP-O |
| Huynh | 2017 | [101] | Valuation | ICECAP-SCM |
| Jones | 2017 | [32] | Validation | ICECAP-A |
| Kaambwa | 2019 | [69] | Validation | ASCOT |
| Karimi | 2016 | [49] | Incorporation | General |
| Keeley | 2013 | [80] | Validation | ICECAP-A |
| Keeley | 2015 | [81] | Validation | ICECAP-A |
| Keeley | 2016 | [27] | Comparison | ICECAP-A |
| Khan | 2018 | [116] | Validation | ICECAP-A |
| Kinghorn | 2015 | [65] | Development | Pain Q |
| Łaszewska | 2019 | [17] | Comparison | OxCAP-MH |
| Linton | 2018 | [108] | Validation | ICECAP-A |
| Looman | 2014 | [98] | Validation | ICECAP-O |
| Lorgelly | 2015 | [63] | Development | OCAP-18 |
| Makai | 2014 | [6] | Validation | ASCOT, ICECAP-O |
| Makai | 2015 | [31] | Empirical | ICECAP-O |
| Makai | 2012 | [92] | Validation | ICECAP-O |
| Makai | 2014 | [18] | Validation | ICECAP-O |
| Malley | 2012 | [70] | Validation | ASCOT |
| Mansdotter | 2017 | [47] | Incorporation | General |
| Milte | 2014 | [71] | Comparison | ASCOT |
| Milte | 2018 | [93] | Validation | ICECAP-O |
| Mitchell | 2017 | [13] | Incorporation | General |
| Mitchell | 2015 | [37] | Validation | ICECAP-A |
| Mitchell | 2013 | [94] | Comparison | ICECAP-O |
| Mitchell | 2015 | [48] | Incorporation | General |
| Mitchell | 2017 | [38] | Comparison | ICECAP-A |
| Netten | 2012 | [52] | Development | ASCOT |
| Parker | 2019 | [43] | Empirical | ICECAP-A |
| Parsons | 2014 | [95] | Validation | ICECAP-O |
| Patty | 2018 | [46] | Empirical | ICECAP-O |
| Peak | 2018 | [84] | Validation | ICECAP-A |
| Rand | 2017 | [72] | Comparison | ASCOT |
| Rand | 2012 | [58] | Development | ASCOT-proxy |
| Ratcliffe | 2013 | [99] | Validation | ICECAP-O |
| Sacchetto | 2016 | [56] | Development | ACQ‐CMH‐104 |
| Sacchetto | 2018 | [66] | Validation | ACQ‐CMH‐104 |
| Sarabia-Cobo | 2017 | [87] | Comparison | ICECAP-O |
| Shiroiwa | 2018 | [105] | Validation | ASCOT |
| Simon | Unpublished | [114] | Empirical | OxCAP-MH |
| Simon | 2018 | [117] | Translation | OxCAP-MH |
| Simon | 2013 | [39] | Development | OxCAP-MH |
| Stevens | 2018 | [73] | Comparison | ASCOT |
| Sutton | 2014 | [62] | Development | ICECAP-SCM |
| Tang | 2018 | [107] | Comparison | ICECAP-A |
| Towers | 2015 | [75] | Validation | ASCOT |
| Towers | 2016 | [67] | Validation | ASCOT |
| Turnpenny | 2018 | [57] | Development | ASCOT Easy Read |
| Van Leeuwen | 2015 | [74] | Comparison | ASCOT, ICECAP-O |
| Van Leeuwen | 2015 | [106] | Validation | ASCOT |
| Van Leeuwen | 2014 | [104] | Validation | ASCOT |
| Van Leeuwen | 2015 | [28] | Validation | ASCOT, ICECAP-O |
| Vergunst | 2017 | [19] | Comparison | OxCAP-MH |
| Williams | 2016 | [42] | Empirical | ICECAP-O |
| Xin | 2017 | [96] | Comparison | ICECAP-O |
Appendix 4
See Table 9.
Table 9.
Correlations reported in the included studies
| Capabilities instrument | Compared with (long name) | Compared with (short name) | Country | Population | Number of informants | Measurement of correlation | Value of correlation | Reference |
|---|---|---|---|---|---|---|---|---|
| ACQ‐CMH‐104 | WHOQOL‐Bref | WHOQOL‐Bref | Portugal | Psychiatric patients participating in community mental health organisations | 129 | Pearson coefficient | 0.60 | [66] |
| ACQ‐CMH‐104 | RAS-P | Recovery assessment scale | Portugal | Psychiatric patients participating in community mental health organisations | 92 | Pearson coefficient | 0.46 | [66] |
| ASCOT | EQ-5D-3L | EQ-5D-3L | UK | Day care for older people | 224 | Spearman Rank | 0.47 | [68] |
| ASCOT | ICECAP-O | ICECAP-O | UK | Older social care users | 205 | Spearman Rank | 0.81 | [21] |
| ASCOT | EQ-5D-5L | EQ-5D-5L | UK | Older social care users | 205 | Spearman Rank | 0.63 | [21] |
| ASCOT | EQ-5D-VAS | EQ-5D-VAS | UK | Older social care users | 205 | Spearman Rank | 0.64 | [21] |
| ASCOT | Barthel Index | Barthel Index | UK | Older social care users | 205 | Spearman Rank | 0.45 | [21] |
| ASCOT | GDS-15 (negative correlation) | GDS-15* | UK | Older social care users | 205 | Spearman Rank | 0.69 | [21] |
| ASCOT | OPQOL-13 | OPQOL-13 | UK | Older social care users | 205 | Spearman Rank | 0.76 | [21] |
| ASCOT | SWLS | SWLS | UK | Older social care users | 205 | Spearman Rank | 0.74 | [21] |
| ASCOT | Cantril’s Ladder | Cantril’s Ladder | UK | Older social care users | 205 | Spearman Rank | 0.66 | [21] |
| ASCOT | Older People’s Quality-of-Life brief questionnaire | OPQoL-Brief | Australia | Community-dwelling older people receiving aged care services | 87 | Spearman Rank | 0.58 | [69] |
| ASCOT | EQ-5D-3L | EQ-5D-3L | UK | Older people receiving publicly funded home care services | 301 | Pearson correlation | 0.40 | [70] |
| ASCOT | EQ-5D-5L | EQ-5D-5L | Australia | Older adults in a day rehabilitation facility | 22 | Spearman Rank | 0.24 | [71] |
| ASCOT | Brief Older People’s Quality of Life | OPQOL-brief | Australia | Older adults in a day rehabilitation facility | 22 | Spearman Rank | 0.38 | [71] |
| ASCOT | EQ-5D-3L | EQ-5D-3L | UK | Older home care residents | 301 | Pearson coefficient | 0.41 | [52] |
| ASCOT | GHQ-12 (negative correlation) | GHQ-12* | UK | Older home care residents | 301 | Pearson coefficient | 0.58 | [52] |
| ASCOT | Control and autonomy subscale of CASP-12 | CASP-12 | UK | Older home care residents | 301 | Pearson coefficient | 0.58 | [52] |
| ASCOT | EQ-5D-3L | EQ-5D-3L | UK | General population | 200 | Gradient | 0.98 | [73] |
| ASCOT | EQ-5D-3L | EQ-5D-3L | Netherlands | Frail older adults living at home | 190 | Spearman Rank | 0.41 | [74] |
| ASCOT | ICECAP-O | ICECAP-O | Netherlands | Frail older adults living at home | 190 | Spearman Rank | 0.41 | [74] |
| ASCOT | EQ-5D-3L | EQ-5D-3L | UK | Community-based adult social care service users | 748 | Spearman Rank | 0.37 | [72] |
| ASCOT | ICECAP-O | ICECAP-O | UK | Community-based adult social care service users | 748 | Spearman Rank | 0.67 | [72] |
| ASCOT | ICECAP-A | ICECAP-A | UK | Community-based adult social care service users | 748 | Spearman Rank | 0.62 | [72] |
| ASCOT-Carer | Carer Experience Scale (CES) | CES | UK | Social care recipients | 376 | Spearman Rank | 0.58 | [76] |
| ASCOT-Carer | Carer Strain Index (negative correlation) | CSI | UK | Social care recipients | 384 | Spearman Rank | − 59 | [76] |
| ASCOT-Carer | EQ-5D-3L | EQ-5D-3L | UK | Social care recipients | 382 | Spearman Rank | 0.34 | [76] |
| ASCOT-Carer | QoL (single item using a 7-point Likert scale) | QoL | UK | Social care recipients | 384 | Spearman Rank | 0.62 | [76] |
| ICECAP-A | Assessment of Quality of Life | AQoL-8D | Australia, Canada, Germany, Norway, UK, USA | Patients with seven chronic conditions and a sample of the ‘healthy’ public | 8022 | Spearman Rank | 0.80 | [20] |
| ICECAP-A | EQ-5D-5L | EQ-5D-5L | Australia, Canada, Germany, Norway, UK, USA | Patients with seven chronic conditions and a sample of the ‘healthy’ public | 8022 | Spearman Rank | 0.60 | [20] |
| ICECAP-A | 15D | 15D | 6 countries (MIC) | Representative healthy cohort and from patients in eight clinical areas | 6756 | Pearson coefficient (average of correlations among factors) | 0.50 | [24] |
| ICECAP-A | AQoL-8D | AQoL-8D | 6 countries (MIC) | Representative healthy cohort and from patients in eight clinical areas | 6756 | Pearson coefficient (average of correlations among factors) | 0.31 | [24] |
| ICECAP-A | EQ-5D-5L | EQ-5D-5L | 6 countries (MIC) | Representative healthy cohort and from patients in eight clinical areas | 6756 | Pearson coefficient (average of correlations among factors) | 0.49 | [24] |
| ICECAP-A | HUI-3 | HUI-3 | 6 countries (MIC) | Representative healthy cohort and from patients in eight clinical areas | 6756 | Pearson coefficient (average of correlations among factors) | 0.32 | [24] |
| ICECAP-A | SF-6D | SF-6D | 6 countries (MIC) | Representative healthy cohort and from patients in eight clinical areas | 6756 | Pearson coefficient (average of correlations among factors) | 0.47 | [24] |
| ICECAP-A | HUI-3 | HUI-3 | Australia, Canada, Germany, Norway, UK, and USA | Individuals with self-reported depression | 917 | R2 | 0.46 | [79] |
| ICECAP-A | SF-6D | SF-6D | Australia, Canada, Germany, Norway, UK, and USA | Individuals with self-reported depression | 917 | R2 | 0.36 | [79] |
| ICECAP-A | 15D | 15D | Australia, Canada, Germany, Norway, UK, and USA | Individuals with self-reported depression | 917 | R2 | 0.42 | [79] |
| ICECAP-A | Assessment of Quality-of-Life Multi-Attribute Utility Instrument | AQoL-8D | Australia, Canada, Germany, Norway, UK, and USA | Individuals with self-reported depression | 917 | R2 | 0.58 | [79] |
| ICECAP-A | EQ-5D-5L | EQ-5D-5L | Australia, Canada, Germany, Norway, UK, and USA | Individuals with self-reported depression | 917 | R2 | 0.34 | [79] |
| ICECAP-A | EQ-5D-5L | EQ-5D-5L | Canada | Patients with Spinal Cord Injury | 364 | Path analysis | 0.37 | [78] |
| ICECAP-A | Assessment of Quality-of-Life Multi-Attribute Utility Instrument | AQoL-8D | Canada | Patients with Spinal Cord Injury | 364 | Path analysis | 0.54 | [78] |
| ICECAP-A | Leeds Dependence Questionnaire (negative correlation) | LDQ* | UK | Individuals receiving opiate substitution treatment for more than 12 months | 83 | Pearson coefficient | 0.48 | [34] |
| ICECAP-A | Social Satisfaction Questionnaire | SSQ | UK | Individuals receiving opiate substitution treatment for more than 12 months | 83 | Pearson coefficient | 0.43 | [34] |
| ICECAP-A | EQ-5D-3L | EQ-5D-3L | UK | Women with lower urinary tract symptoms | 478 | Pearson coefficient | 0.53 | [23] |
| ICECAP-A | EQ-5D-3L | EQ-5D-3L | UK | Knee pain patients in primary care | 500 | Spearman Rank | 0.49 | [27] |
| ICECAP-A | 36-Item Short Form Health Survey | SF-36 | Australia, Canada, Germany, Norway, UK, USA | Patients with seven chronic conditions and a sample of the ‘healthy’ public | 8022 | R2 | 0.57 | [116] |
| ICECAP-A | 36-Item Short Form Health Survey | AQoL-8D | Australia, Canada, Germany, Norway, UK, USA | Patients with seven chronic conditions and a sample of the ‘healthy’ public | 8022 | R2 | 0.71 | [116] |
| ICECAP-A | EQ-5D-5L | EQ-5D-5L | Germany | Healthy Samples and Seven Health Condition Groups | 1212 | Pearson coefficient | 0.62 | [108] |
| ICECAP-A | SWLS | SWLS | Germany | Healthy Samples and Seven Health Condition Groups | 1212 | Pearson coefficient | 0.66 | [108] |
| ICECAP-A | SF-6D | SF-6D | Germany | Healthy Samples and Seven Health Condition Groups | 1212 | Pearson coefficient | 0.64 | [108] |
| ICECAP-A | Depression, Anxiety and Stress Scale | DASS-D | 4 English speaking countries of MIC | Individuals with depression | 617 | R2 | ? | [38] |
| ICECAP-A | Kessler Psychological Distress Scale | K10 | 4 English speaking countries of MIC | Individuals with depression | 617 | R2 | ? | [38] |
| ICECAP-A | EQ-5D-3L | EQ-5D-3L | China | General population | 975 | Polychoric correlation coefficient | 0.45 | [107] |
| ICECAP-O | EQ-5D-3L | EQ-5D-3L | UK | General population aged 65 and over | 315 | Chi-squared tests | 0.42 (Attachment), 0.008** (Security), < 0.001** (Role), < 0.001** (Enjoyment), < 0.001** (Control) | [40] |
| ICECAP-O | EQ-5D | EQ-5D-3L | Australia | Patients from an outpatient day rehabilitation unit | 80 | Spearman Rank | 0.44 | [22] |
| ICECAP-O | CTM-3 | CTM-3 | Australia | Patients from an outpatient day rehabilitation unit | 82 | Spearman Rank | 0.23 | [22] |
| ICECAP-O | EQ-5D | EQ-5D-3L | Canada | Participants visiting the Vancouver Falls Prevention Clinic | 215 | Spearman Rank | 0.47 | [25] |
| ICECAP-O | EQ-5D-3L | EQ-5D-3L | UK | Aged over 65 years, requiring a hospital visit and/or care home resident, and recruited to one of 3 studies forming the Medical Crisis in Older People (MCOP) programme | 584 | R2 | 0.35 | [26] |
| ICECAP-O | EQ-5D-5L | EQ-5D-5L | UK | Older social care users | 207 | Spearman Rank | 0.68 | [21] |
| ICECAP-O | EQ-5D-VAS | EQ-5D-VAS | UK | Older social care users | 208 | Spearman Rank | 0.66 | [21] |
| ICECAP-O | Barthel Index | Barthel Index | UK | Older social care users | 209 | Spearman Rank | 0.49 | [21] |
| ICECAP-O | GDS-15 (negative correlation) | GDS-15* | UK | Older social care users | 210 | Spearman Rank | 0.73 | [21] |
| ICECAP-O | OPQOL-13 | OPQOL-13 | UK | Older social care users | 211 | Spearman Rank | 0.80 | [21] |
| ICECAP-O | SWLS | SWLS | UK | Older social care users | 212 | Spearman Rank | 0.82 | [21] |
| ICECAP-O | Cantril’s Ladder | Cantril’s Ladder | UK | Older social care users | 213 | Spearman Rank | 0.74 | [21] |
| ICECAP-O | EQ-5D-5L | EQ-5D-5L | UK | People aged 70 and older | 516 | Spearman Rank | 0.63 | [90] |
| ICECAP-O | Barthel Index | Barthel Index | Germany | Nursing Home Residents with Dementia | 95 | Pearson coefficient | 0.72 | [18] |
| ICECAP-O | EQ-5D-3L | EQ-5D-3L | Germany | Nursing Home Residents with Dementia | 95 | Pearson coefficient | 0.69 | [18] |
| ICECAP-O | ADRQL | ADRQL | Germany | Nursing Home Residents with Dementia | 95 | Pearson coefficient | 0.53 | [18] |
| ICECAP-O | EQ-5D-3L | EQ-5D-3L | Australia | Older people following surgery for hip fracture | 87 | Spearman Rank | 0.53 | [93] |
| ICECAP-O | Western Ontario and McMaster Universities | WOMAC | UK | Osteoarthritis patients requiring joint replacement | 105 | R2 | 0.40 | [94] |
| ICECAP-O | EQ-5D-3L | EQ-5D-3L | UK | Participants aged 65 years and over with an intracapsular fracture of the hip | 113 | Pearson coefficient | 0.34 | [95] |
| ICECAP-O | Oxford Hip Score | OHS | UK | Participants aged 65 years and over with an intracapsular fracture of the hip | 113 | Pearson coefficient | 0.38 | [95] |
| ICECAP-O | Barthel Index measure of activities of daily living | Barthel Index | Spain | Nursing professionals serving as proxy respondents for dementia patients | 217 | Not reported | 0.68 | [87] |
| ICECAP-O | Alzheimer’s Disease-Related Quality of Life | ADRQL | Spain | Nursing professionals serving as proxy respondents for dementia patients | 217 | Not reported | 0.61 | [87] |
| ICECAP-O | EQ-5D extended with a cognitive dimension | EQ-5D + C | Spain | Nursing professionals serving as proxy respondents for dementia patients | 217 | Not reported | 0.62 | [87] |
| ICECAP-O | EQ-5D-3L | EQ-5D-3L | Netherlands | Frail older adults living at home | 190 | Spearman Rank | 0.63 | [74] |
| ICECAP-O | Parkinson’s specific QoL | PDQ-39 | ? | People with Parkinson’s | 1023 | Not reported | 0.53 | [96] |
| ICECAP-O family version | EQ-5D family version | EQ-5D family version | Netherlands | Nursing professionals of psycho-geriatric elderly | 96 | Pearson coefficient | 0.57 | [92] |
| ICECAP-O family version | EQ-VAS family version | EQ-VAS family version | Netherlands | Family members of psycho-geriatric elderly | 68 | Pearson coefficient | 0.43 | [92] |
| ICECAP-O nursing version | EQ-5D nursing version | EQ-5D nursing version | Netherlands | Nursing professionals of psycho-geriatric elderly | 96 | Pearson coefficient | 0.48 | [92] |
| ICECAP-O nursing version | EQ-VAS nursing version | EQ-VAS nursing version | Netherlands | Family members of psycho-geriatric elderly | 68 | Pearson coefficient | 0.55 | [92] |
| OxCAP-MH | EQ-5D-index UK | EQ-5D-index UK | Austria | Patients in socio-psychiatric services | 159 | Spearman Rank | 0.67 | [17] |
| OxCAP-MH | EQ-5D-index DE | EQ-5D-index DE | Austria | Patients in socio-psychiatric services | 160 | Spearman Rank | 0.66 | [17] |
| OxCAP-MH | EQ-5D VAS | EQ-5D VAS | Austria | Patients in socio-psychiatric services | 161 | Spearman Rank | 0.58 | [17] |
| OxCAP-MH | BSI-18 | BSI-18 | Austria | Patients in socio-psychiatric services | 162 | Spearman Rank | − 67 | [17] |
| OxCAP-MH | WHOQOL-BREF Physical health | WHOQOL-BREF Physical health | Austria | Patients in socio-psychiatric services | 163 | Spearman Rank | 0.69 | [17] |
| OxCAP-MH | WHOQOL-BREF Psychological | WHOQOL-BREF Psychological | Austria | Patients in socio-psychiatric services | 164 | Spearman Rank | 0.75 | [17] |
| OxCAP-MH | WHOQOL-BREF Social relationships | WHOQOL-BREF Social relationships | Austria | Patients in socio-psychiatric services | 165 | Spearman Rank | 0.50 | [17] |
| OxCAP-MH | WHOQOL-BREF Environment | WHOQOL-BREF Environment | Austria | Patients in socio-psychiatric services | 166 | Spearman Rank | 0.69 | [17] |
| OxCAP-MH | Mini-ICF-APP | Mini-ICF-APP | Austria | Patients in socio-psychiatric services | 167 | Spearman Rank | − 0.47 | [17] |
| OxCAP-MH | Global Assessment of Functioning | GAF | Austria | Patients in socio-psychiatric services | 168 | Spearman Rank | 0.35 | [17] |
| OxCAP-MH | EQ-5D-3L Utility | EQ-5D-3L | UK | Patients with psychosis | 172 | Pearson coefficient | 0.45 | [19] |
| OxCAP-MH | EuroQol Visual Analogue Scale | EQ-5D-VAS | UK | Patients with psychosis | 172 | Pearson coefficient | 0.52 | [19] |
| OxCAP-MH | Brief Psychiatric Rating Scale (negative correlation) | BPRS* | UK | Patients with psychosis | 172 | Pearson coefficient | 0.41 | [19] |
| OxCAP-MH | Global Assessment of Functioning | GAF | UK | Patients with psychosis | 172 | Pearson coefficient | 0.24 | [19] |
| OxCAP-MH | Objective Social Outcomes Index | SIX | UK | Patients with psychosis | 172 | Pearson coefficient | 0.12 | [19] |
| Women’s Capabilities Index | WHOQOL-Bref | WHOQOL-Bref | Malawi | Women from Mchinji, Malawi | 20 | Pearson correlation | 0.62 | [64] |
Appendix 5
See Table 10.
Table 10.
Abbreviations of health-related instruments
| Short form | Full name of instrument |
|---|---|
| 15D | 15D |
| SF-36 | 36-Item Short Form Health Survey |
| ADRQL | Alzheimer’s Disease-Related Quality of Life |
| AQoL-8D | Assessment of Quality-of-Life Multi-Attribute Utility Instrument |
| Barthel Index | Barthel Index measure of activities of daily living (ADL) |
| OPQOL-brief | brief Older People’s Quality of Life |
| BPRS | Brief Psychiatric Rating Scale |
| BSI-18 | brief symptom inventory 18 |
| Cantril’s Ladder | Cantril’s Ladder |
| CES | Carer Experience Scale |
| CSI | Carer Strain Index |
| CASP-12 | Control and autonomy subscale of CASP-12 |
| CTM-3 | Care Transitions Measure |
| DASS-D | Depression, Anxiety and Stress Scale (DASS-D of DASS-21) |
| EQ-5D + C | EQ-5D extended with a cognitive dimension |
| EQ-5D-VAS | EuroQol Visual Analogue Scale |
| GDS-15 | 15-item Geriatric Depression Scale |
| GHQ-12 | 12-item General Health Questionnaire |
| GAF | Global Assessment of Functioning |
| HUI-3 | Health Utilities Index Mark 3 |
| K10 | Kessler Psychological Distress Scale |
| LDQ | Leeds Dependence Questionnaire |
| Mini-ICF-APP | Mini-ICF-APP Social Functioning Scale |
| SIX | Objective Social Outcomes Index |
| OPQoL-Brief | Older People’s Quality-of-Life brief questionnaire (13 items) |
| OHS | Oxford Hip Score |
| PDQ-39 | Parkinson’s specific Quality of Life |
| RAS-P | Recovery Assessment Scale |
| SF-6D | Short Form Six Dimension |
| SSQ | Social Satisfaction Questionnaire |
| SWLS | Satisfaction with Life Scale |
| WOMAC | Western Ontario and McMaster Universities |
| WHOQOL-Bref | World Health Organization Quality-of-Life Instruments - abbreviated version |
Appendix 6
See Table 11.
Table 11.
Details of applied evaluations
| Author, Year | Country | Disease | Intervention | Population | Perspective | Capability measure | Time points | Missing data |
|---|---|---|---|---|---|---|---|---|
| Barnes, 2016 | UK | Schizophrenia | Citalopram (ACTIONS trial) | Adult patients | Societal | ICECAP-A | Baseline; 12–36–48 weeks | Multiple imputation |
| Bray, 2017 | UK | Visual impairment | Portable electronic vision enhancement system (compared with optical low vision aids) | Adult patients | Societal | ICECAP-A | Baseline; 2 months; 4 months | Not reported |
| Burns, 2016 | UK | Psychosis | Community treatment orders | Adult patients | Health and social care | OxCAP-MH | Baseline; 6 months; 12 months | Multiple imputation |
| Goranitis, 2017 | UK | Drug addiction | 2 Psychological interventions relative to usual care | Treatment resistant adult addicts | Health and social care | ICECAP-A | Baseline; 12 months | Chained equations with predictive mean matching |
| Henderson, 2013 | UK | Heart failure, chronic obstructive pulmonary disease, or diabetes | Community-based telehealth (Whole Systems Demonstrator) | People with a long-term condition | Societal | ICECAP-O | Baseline; 12 months | Multiple imputation |
| Makai, 2014 | Netherlands | Health decline in the elderly | Walcheren integrated care model | Frail elderly | Societal | ICECAP-O | Baseline, 3 months | Not reported |
| Parker, 2019 | UK | Diabetic plantar ulceration | Traditional vs. digital foot orthoses | Adult patients | Healthcare provider | ICECAP-A | Baseline; 6 months | Not reported |
| Patty, 2018 | Netherlands | Visual impairment | ICT training | Adult patients | Societal | ICECAP-O | 3 months; post-intervention; pre-study | Not reported |
| Simon, unpublished | UK | Schizophrenia or schizoaffective disorder and depression | Positive Memory Training (PoMeT) | Adult patients | (1) Healthcare, (2) Health and social care, (3) Broader societal | ICECAP-A and OxCAP-MH | Baseline, 3, 6 and 9 months | Stepwise approach |
| Williams, 2016 | UK | Hip fracture | Multidisciplinary rehabilitation package following hip fracture | Older adults (aged ≥ 65) | Healthcare provider | ICECAP-O | Baseline, 3 months | Not reported |
Author contributions
TH and JS conceived of the presented idea and developed the conceptual framework of this research. JS provided the resources to this study. TH and AL conducted the systematic literature search and sifting of abstracts and titles. TH took the lead in writing the manuscript in close consultation with JC, AL, TS and JS. All authors provided critical feedback and helped shape the research, analysis and manuscript.
Funding
Joanna Coast is supported by the Wellcome Trust [205384/Z/16/Z]. The author(s) received no further financial support for the research, authorship, and/or publication of this article.
Compliance with ethical standards
Conflict of interest
JC has led the development of the ICECAP measures. JS has led the development of the OxCAP-MH measure. The remaining authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Standard Methods for the economic evaluation of health care programme. 3. Oxford: Oxford University Press; 2005. [Google Scholar]
- 2.Fox-Rushby JCJ. Approaches to measuring health and life. In: Fox-Rushby JCJ, editor. Economic evaluation. Maidenhead: London School of Hygiene and Tropical Medicine, Open University Press; 2008. pp. 85–100. [Google Scholar]
- 3.Nord E. Beyond QALYs: Multi-criteria based estimation of maximum willingness to pay for health technologies. The European Journal of Health Economics. 2018;19(2):267–275. doi: 10.1007/s10198-017-0882-x. [DOI] [PubMed] [Google Scholar]
- 4.Greco G, Lorgelly P, Yamabhai I. Outcomes in economic evaluations of public health interventions in low- and middle-income countries: Health capabilities and subjective wellbeing. Health Economics. 2016;25(Suppl 1):83–94. doi: 10.1002/hec.3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Makai P, Brouwer WBF, Koopmanschap MA, Stolk EA, Nieboer AP. Quality of life instruments for economic evaluations in health and social care for older people: A systematic review. Social Science and Medicine. 2014;102:83–93. doi: 10.1016/j.socscimed.2013.11.050. [DOI] [PubMed] [Google Scholar]
- 6.Al-Janabi H, Flynn TN, Coast J. QALYs and carers. PharmacoEconomics. 2011;29(12):1015–1023. doi: 10.2165/11593940-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 7.Sen A. Commodities and capabilities. Amsterdam: Elsevier; 1985. [Google Scholar]
- 8.Coast J, Flynn T, Sutton E, Al-Janabi H, Vosper J, Lavender S, et al. Investigating choice experiments for preferences of older people (ICEPOP): Evaluative spaces in health economics. Journal of Health Services Research and Policy. 2008;13(SUPPL. 3):31–37. doi: 10.1258/jhsrp.2008.008024. [DOI] [PubMed] [Google Scholar]
- 9.Nederland, Z. (2016). Guideline for economic evaluations in healthcare. Retrieved from https://english.zorginstituutnederland.nl/publications/reports/2016/06/16/guideline-for-economic-evaluations-in-healthcare.
- 10.NICE. (2017). Developing NICE guidelines: The manual 2014 (April 2017 update)—Incorporating economic evaluation. [PMG20]: National Institute for Health and Clinical Excellence.
- 11.Proud L, McLoughlin C, Kinghorn P. ICECAP-O, the current state of play: A systematic review of studies reporting the psychometric properties and use of the instrument over the decade since its publication. Quality of Life Research. 2019 doi: 10.1007/s11136-019-02114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hartley RJ, Keen EM, Large JA, Tedd LA. Search strategies. In: Hartley RJ, editor. Online searching: Principles and practice. London: Bowker-Saur; 1990. pp. 153–173. [Google Scholar]
- 13.Mitchell PM, Roberts TE, Barton PM, Coast J. Applications of the capability approach in the health field: A literature review. Social Indicators Research. 2017;133(1):345–371. doi: 10.1007/s11205-016-1356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anand P, Wailoo A. Utilities versus rights to publicly provided goods: Arguments and evidence from health care rationing. Economica. 2000;67:543–577. [Google Scholar]
- 15.Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Quality of Life Research. 2010;19(4):539–549. doi: 10.1007/s11136-010-9606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B. Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain. 2006;125(1):143–157. doi: 10.1016/j.pain.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Laszewska A, Schwab M, Leutner E, Oberrauter M, Spiel G, Simon J. Measuring broader wellbeing in mental health services: Validity of the German language OxCAP-MH capability instrument. Quality of Life Research. 2019;28(8):2311–2323. doi: 10.1007/s11136-019-02187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Makai P, Beckebans F, Van Exel J, Brouwer WBF. Quality of life of nursing home residents with dementia: Validation of the German version of the ICECAP-O. PLoS ONE. 2014;9(3):e92016. doi: 10.1371/journal.pone.0092016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vergunst F, Jenkinson C, Burns T, Anand P, Gray A, Rugkåsa J, et al. Psychometric validation of a multi-dimensional capability instrument for outcome measurement in mental health research (OxCAP-MH) Health and Quality of Life Outcomes. 2017;15(1):250. doi: 10.1186/s12955-017-0825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen G, Ratcliffe J, Kaambwa B, McCaffrey N, Richardson J. Empirical comparison between capability and two health-related quality of life measures. Social Indicators Research. 2018;140(1):175–190. [Google Scholar]
- 21.Hackert MQN, Exel JV, Brouwer WBF. Valid outcome measures in care for older people: Comparing the ASCOT and the ICECAP-O. Value in Health. 2017;20(7):936–944. doi: 10.1016/j.jval.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Couzner L, Ratcliffe J, Crotty M. The relationship between quality of life, health and care transition: An empirical comparison in an older post-acute population. Health and Quality of Life Outcomes. 2012 doi: 10.1186/1477-7525-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goranitis I, Coast J, Al-Janabi H, Latthe P, Roberts TE. The validity and responsiveness of the ICECAP-A capability-well-being measure in women with irritative lower urinary tract symptoms. Quality of Life Research. 2016;25(8):2063–2075. doi: 10.1007/s11136-015-1225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Engel L, Mortimer D, Bryan S, Lear SA, Whitehurst DGT. An investigation of the overlap between the ICECAP-A and five preference-based health-related quality of life instruments. PharmacoEconomics. 2017;35(7):741–753. doi: 10.1007/s40273-017-0491-7. [DOI] [PubMed] [Google Scholar]
- 25.Davis JC, Liu-Ambrose T, Richardson CG, Bryan S. A comparison of the ICECAP-O with EQ-5D in a falls prevention clinical setting: Are they complements or substitutes? Quality of Life Research. 2013;22(5):969–977. doi: 10.1007/s11136-012-0225-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Franklin M, Payne K, Elliott RA. Quantifying the relationship between capability and health in older people: Can’t Map Won’t Map. Medical Decision Making. 2018;38(1):79–94. doi: 10.1177/0272989X17732975. [DOI] [PubMed] [Google Scholar]
- 27.Keeley T, Coast J, Nicholls E, Foster NE, Jowett S, Al-Janabi H. An analysis of the complementarity of ICECAP-A and EQ-5D-3 L in an adult population of patients with knee pain. Health and Quality of Life Outcomes. 2016;14(1):36. doi: 10.1186/s12955-016-0430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Leeuwen KM, Jansen AP, Muntinga ME, Bosmans JE, Westerman MJ, van Tulder MW, et al. Exploration of the content validity and feasibility of the EQ-5D-3L, ICECAP-O and ASCOT in older adults. BMC Health Services Research. 2015;15:201. doi: 10.1186/s12913-015-0862-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bailey C, Kinghorn P, Orlando R, Armour K, Perry R, Jones L, et al. The ICECAP-SCM tells you more about what I’m going through’: A think-aloud study measuring quality of life among patients receiving supportive and palliative care. Palliative Medicine. 2016;30(7):642–652. doi: 10.1177/0269216315624890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davis JC, Hsiung GY, Bryan S, Jacova C, Jacova P, Munkacsy M, et al. Agreement between patient and proxy assessments of quality of life among older adults with vascular cognitive impairment using the EQ-5D-3L and ICECAP-O. PLoS ONE. 2016;11(4):e0153878. doi: 10.1371/journal.pone.0153878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Makai P, Looman W, Adang E, Melis R, Stolk E, Fabbricotti I. Cost-effectiveness of integrated care in frail elderly using the ICECAP-O and EQ-5D: Does choice of instrument matter? European Journal of Health Economics. 2015;16(4):437–450. doi: 10.1007/s10198-014-0583-7. [DOI] [PubMed] [Google Scholar]
- 32.Jones CJ, Payne K, Gannon B, Verstappen S. Exploring the impact of health status and well-being of people with inflammatory arthritis on presenteeism in the workplace: A qualitative study. Annals of the Rheumatic Diseases. 2017;76:437–438. [Google Scholar]
- 33.Al-Janabi H, Peters TJ, Brazier J, Bryan S, Flynn TN, Clemens S, et al. An investigation of the construct validity of the ICECAP-A capability measure. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2013;22(7):1831–1840. doi: 10.1007/s11136-012-0293-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goranitis I, Coast J, Day E, Copello A, Freemantle N, Seddon J, et al. Measuring Health and Broader Well-Being Benefits in the Context of Opiate Dependence: The Psychometric Performance of the ICECAP-A and the EQ-5D-5L. Value in Health. 2016;19(6):820–828. doi: 10.1016/j.jval.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 35.Davis JC, Best JR, Dian L, Khan KM, Hsu CL, Chan W, et al. Are the EQ-5D-3L and the ICECAP-O responsive among older adults with impaired mobility? Evidence from the Vancouver Falls Prevention Cohort Study. Quality of Life Research. 2017;26(3):737–747. doi: 10.1007/s11136-016-1487-z. [DOI] [PubMed] [Google Scholar]
- 36.Couzner L, Crotty M, Norman R, Ratcliffe J. A comparison of the EQ-5D-3L and CECAP-O in an older post-acute patient population relative to the general population. Applied Health Economics and Health Policy. 2013;11(4):415–425. doi: 10.1007/s40258-013-0039-8. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell PM, Al-Janabi H, Richardson J, Iezzi A, Coast J. The relative impacts of disease on health status and capability wellbeing: A multi-country study. PLoS ONE. 2015;10(12):e0143590. doi: 10.1371/journal.pone.0143590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mitchell PM, Al-Janabi H, Byford S, Kuyken W, Richardson J, Iezzi A, et al. Assessing the validity of the ICECAP-A capability measure for adults with depression. BMC Psychiatry. 2017 doi: 10.1186/s12888-017-1211-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Simon J, Anand P, Gray A, Rugkasa J, Yeeles K, Burns T. Operationalising the capability approach for outcome measurement in mental health research. Social Science and Medicine. 2013;98:187–196. doi: 10.1016/j.socscimed.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 40.Coast J, Peters TJ, Natarajan L, Sproston K, Flynn T. An assessment of the construct validity of the descriptive system for the ICECAP capability measure for older people. Quality of Life Research. 2008;17(7):967–976. doi: 10.1007/s11136-008-9372-z. [DOI] [PubMed] [Google Scholar]
- 41.Deidda M, Coll-Planas L, Giné-Garriga M, Guerra-Balic M, Roqué Figuls MI, Tully MA, et al. Cost-effectiveness of exercise referral schemes enhanced by self-management strategies to battle sedentary behaviour in older adults: Protocol for an economic evaluation alongside the SITLESS three-armed pragmatic randomised controlled trial. British Medical Journal Open. 2018 doi: 10.1136/bmjopen-2018-022266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams NH, Roberts JL, Din NU, Totton N, Charles JM, Hawkes CA, et al. Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR): A phase II randomised feasibility study of a multidisciplinary rehabilitation package following hip fracture. British Medical Journal Open. 2016 doi: 10.1136/bmjopen-2016-012422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parker DJ, Nuttall GH, Bray N, Hugill T, Martinez-Santos A, Edwards RT, et al. A randomised controlled trial and cost-consequence analysis of traditional and digital foot orthoses supply chains in a National Health Service setting: Application to feet at risk of diabetic plantar ulceration. Journal of foot and ankle research. 2019;12:2. doi: 10.1186/s13047-018-0311-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barnes TRE, Leeson VC, Paton C, Costelloe C, Simon J, Kiss N, et al. Antidepressant controlled trial for negative symptoms in schizophrenia (ACTIONS): A double-blind, placebo-controlled, randomised clinical trial. Health Technology Assessment. 2016;20(29):1–45. doi: 10.3310/hta20290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burns T, R. J., Yeeles K, Catty J, on behalf of the Oxford Mental Health Coercion (OCTET) Programme Group (2016). Coercion in mental health: A trial of the effectiveness of community treatment orders and an investigation of informal coercion in community mental health care. Programme Grants Applied Research (Vol. 4). [PubMed]
- 46.Patty NJS, Koopmanschap M, Holtzer-Goor K. A cost-effectiveness study of ICT training among the visually impaired in the Netherlands. BMC ophthalmology. 2018 doi: 10.1186/s12886-018-0761-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Månsdotter A, Ekman B, Feldman I, Hagberg L, Hurtig AK, Lindholm L. We propose a novel measure for social welfare and public health: Capability-adjusted life-years, CALYs. Applied Health Economics and Health Policy. 2017;15(4):437–440. doi: 10.1007/s40258-017-0323-0. [DOI] [PubMed] [Google Scholar]
- 48.Mitchell PM, Roberts TE, Barton PM, Coast J. Assessing sufficient capability: A new approach to economic evaluation. Social Science and Medicine. 2015;139:71–79. doi: 10.1016/j.socscimed.2015.06.037. [DOI] [PubMed] [Google Scholar]
- 49.Karimi M, Brazier J, Basarir H. The capability approach: A critical review of its application in health economics. Value in Health. 2016;19(6):795–799. doi: 10.1016/j.jval.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 50.Lorgelly PK. Choice of outcome measure in an economic evaluation: A potential role for the capability approach. PharmacoEconomics. 2015;33(8):849–855. doi: 10.1007/s40273-015-0275-x. [DOI] [PubMed] [Google Scholar]
- 51.Hopkins, W. G. (2002). A new view of statistics. Retrieved February 21, 2019, from, http://www.sportsci.org/resource/stats/effectmag.html.
- 52.Netten A, Burge P, Malley J, Potoglou D, Towers AM, Brazier J, Flynn T, Forder J, Wall B. Outcomes of social care for adults: Developing a preference-weighted measure. Health Technology Assessment. 2012;16(16):1–166. doi: 10.3310/hta16160. [DOI] [PubMed] [Google Scholar]
- 53.Al-Janabi HF, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: The ICECAP-A. Quality of Life Research. 2012;21(1):167–176. doi: 10.1007/s11136-011-9927-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grewal I, Lewis J, Flynn T, Brown J, Bond J, Coast J. Developing attributes for a generic quality of life measure for older people: Preferences or capabilities? Social Science Medicine. 2006;62(8):1891–1901. doi: 10.1016/j.socscimed.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 55.Coast J, Kinghorn P, Mitchell P. The development of capability measures in health economics: Opportunities challenges and progress. Patient. 2015;8(2):119–126. doi: 10.1007/s40271-014-0080-1. [DOI] [PubMed] [Google Scholar]
- 56.Sacchetto B, Aguiar R, Vargas-Moniz MJ, Jorge-Monteiro MF, Neves MJ, Cruz MA, et al. The capabilities questionnaire for the community mental health context (CQ-CMH): A measure inspired by the capabilities approach and constructed through consumer-researcher collaboration. Psychiatric Rehabilitation Journal. 2016;39(1):55–61. doi: 10.1037/prj0000153. [DOI] [PubMed] [Google Scholar]
- 57.Turnpenny A, Caiels J, Whelton B, Richardson L, Beadle-Brown J, Crowther T, et al. Developing an easy read version of the adult social care outcomes toolkit (ASCOT) Journal of Applied Research in Intellectual Disabilities. 2018;31(1):e36–e48. doi: 10.1111/jar.12294. [DOI] [PubMed] [Google Scholar]
- 58.Rand S, Caiels J, Collins G, Forder J. Developing a proxy version of the Adult social care outcome toolkit (ASCOT) Health and Quality of Life Outcomes. 2017 doi: 10.1186/s12955-017-0682-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rand, S., Malley, J., & Netten, A. (2012). Measuring the social care outcomes of informal carers: An interim technical report for the identifying the impact of adult social care (IIASC) Study. In C. a. L. Personal Social Services Research Unit (PSSRU) (Ed.), (Discussion paper ed.).
- 60.Botes R, Vermeulen KM, Gerber AM, Ranchor AV, Buskens E. Functioning and quality of life in dutch oldest old with diverse levels of dependency. Patient Preference and Adherence. 2018;12:2187–2196. doi: 10.2147/PPA.S175388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Canaway A, Al-Janabi H, Kinghorn P, Bailey C, Coast J. Development of a measure (ICECAP-Close Person Measure) through qualitative methods to capture the benefits of end-of-life care to those close to the dying for use in economic evaluation. Palliative Medicine. 2017;31(1):53–62. doi: 10.1177/0269216316650616. [DOI] [PubMed] [Google Scholar]
- 62.Sutton EJ, Coast J. Development of a supportive care measure for economic evaluation of end-of-life care using qualitative methods. Palliative Medicine. 2014;28(2):151–157. doi: 10.1177/0269216313489368. [DOI] [PubMed] [Google Scholar]
- 63.Lorgelly PK, Lorimer K, Fenwick EAL, Briggs AH, Anand P. Operationalising the capability approach as an outcome measure in public health: The development of the OCAP-18. Social Science and Medicine. 2015;142:68–81. doi: 10.1016/j.socscimed.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 64.Greco G, Skordis-Worall J, Mkandawire B, Mills A. What is a good life? Selecting capabilities to assess women’s quality of life in rural Malawi. Social Science and Medicine. 2015;130:69–78. doi: 10.1016/j.socscimed.2015.01.042. [DOI] [PubMed] [Google Scholar]
- 65.Kinghorn P, Robinson A, Smith RD. Developing a capability-based questionnaire for assessing well-being in patients with chronic pain. Social Indicators Research. 2015;120(3):897–916. [Google Scholar]
- 66.Sacchetto B, Ornelas J, Calheiros MM, Shinn M. Adaptation of Nussbaum’s capabilities framework to community mental health: A consumer-based capabilities measure. American Journal of Community Psychology. 2018;61(1–2):32–46. doi: 10.1002/ajcp.12221. [DOI] [PubMed] [Google Scholar]
- 67.Towers AM, Smith N, Palmer S, Welch E, Netten A. The acceptability and feasibility of using the Adult Social Care Outcomes Toolkit (ASCOT) to inform practice in care homes. BMC Health Services Research. 2016 doi: 10.1186/s12913-016-1763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Forder JE, Caiels J. Measuring the outcomes of long-term care. Social Science and Medicine. 2011;73(12):1766–1774. doi: 10.1016/j.socscimed.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 69.Kaambwa B, Gill L, McCaffrey N, Lancsar E, Cameron ID, Crotty M, et al. An empirical comparison of the OPQoL-Brief, EQ-5D-3L and ASCOT in a community dwelling population of older people. Health and Quality of Life Outcomes. 2015 doi: 10.1186/s12955-015-0357-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Malley JN, Towers AM, Netten AP, Brazier JE, Forder JE, Flynn T. An assessment of the construct validity of the ASCOT measure of social care-related quality of life with older people. Health and Quality of Life Outcomes. 2012 doi: 10.1186/1477-7525-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Milte CM, Walker R, Luszcz MA, Lancsar E, Kaambwa B, Ratcliffe J. How important is health status in defining quality of life for older people? An exploratory study of the views of older South Australians. Applied Health Economics and Health Policy. 2014;12(1):73–84. doi: 10.1007/s40258-013-0068-3. [DOI] [PubMed] [Google Scholar]
- 72.Rand S, Malley J, Towers AM, Netten A, Forder J. Validity and test-retest reliability of the self-completion adult social care outcomes toolkit (ASCOT-SCT4) with adults with long-term physical, sensory and mental health conditions in England. Health and Quality of Life Outcomes. 2017 doi: 10.1186/s12955-017-0739-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stevens K, Brazier J, Rowen D. Estimating an exchange rate between the EQ-5D-3L and ASCOT. European Journal of Health Economics. 2018;19(5):653–661. doi: 10.1007/s10198-017-0910-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van Leeuwen KM, Bosmans JE, Jansen APD, Hoogendijk EO, van Tulder MW, van der Horst HE, et al. Comparing measurement properties of the EQ-5D-3L, ICECAP-O, and ASCOT in frail older adults. Value in Health. 2015;18(1):35–43. doi: 10.1016/j.jval.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 75.Towers AM, Holder J, Smith N, Crowther T, Netten A, Welch E, et al. Adapting the adult social care outcomes toolkit (ASCOT) for use in care home quality monitoring: Conceptual development and testing. BMC Health Services Research. 2015 doi: 10.1186/s12913-015-0942-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rand SE, Malley JN, Netten AP, Forder JE. Factor structure and construct validity of the Adult Social Care Outcomes Toolkit for Carers (ASCOT-Carer) Quality of Life Research. 2015;24(11):2601–2614. doi: 10.1007/s11136-015-1011-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Al-Janabi H, Flynn TN, Peters TJ, Bryan S, Coast J. Test-retest reliability of capability measurement in the UK general population. Health Economics (United Kingdom) 2015;24(5):625–630. doi: 10.1002/hec.3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Engel L, Bryan S, Noonan VK, Whitehurst DGT. Using path analysis to investigate the relationships between standardized instruments that measure health-related quality of life, capability wellbeing and subjective wellbeing: An application in the context of spinal cord injury. Social Science and Medicine. 2018;213:154–164. doi: 10.1016/j.socscimed.2018.07.041. [DOI] [PubMed] [Google Scholar]
- 79.Engel L, Chen G, Richardson J, Mihalopoulos C. The impact of depression on health-related quality of life and wellbeing: Identifying important dimensions and assessing their inclusion in multi-attribute utility instruments. Quality of Life Research. 2018;27(11):2873–2884. doi: 10.1007/s11136-018-1936-y. [DOI] [PubMed] [Google Scholar]
- 80.Keeley T, Al-Janabi H, Lorgelly P, Coast J. A qualitative assessment of the content validity of the ICECAP-A and EQ-5D-5L and their appropriateness for use in health research. PLoS ONE. 2013 doi: 10.1371/journal.pone.0085287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Keeley T, Al-Janabi H, Nicholls E, Foster NE, Jowett S, Coast J. A longitudinal assessment of the responsiveness of the ICECAP-A in a randomised controlled trial of a knee pain intervention. Quality of Life Research. 2015;24(10):2319–2331. doi: 10.1007/s11136-015-0980-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Al-Janabi H, Keeley T, Mitchell P, Coast J. Can capabilities be self-reported? A think aloud study. Social Science and Medicine. 2013;87:116–122. doi: 10.1016/j.socscimed.2013.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Coast J, Bailey C, Orlando R, Armour K, Perry R, Jones L, et al. Adaptation, acceptance and adaptive preferences in health and capability well-being measurement amongst those approaching end of life. Patient-Patient Centered Outcomes Research. 2018;11(5):539–546. doi: 10.1007/s40271-018-0310-z. [DOI] [PubMed] [Google Scholar]
- 84.Peak J, Goranitis I, Day E, Copello A, Freemantle N, Frew E. Predicting health-related quality of life (EQ-5D-5 L) and capability wellbeing (ICECAP-A) in the context of opiate dependence using routine clinical outcome measures: CORE-OM, LDQ and TOP. Health and Quality of Life Outcomes. 2018 doi: 10.1186/s12955-018-0926-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Flynn TN, Huynh E, Peters TJ, Al-Janabi H, Clemens S, Moody A, et al. Scoring the icecap-a capability instrument. Estimation of a UK general population tariff. Health Economics. 2015;24(3):258–269. doi: 10.1002/hec.3014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hörder H, Gustafsson S, Rydberg T, Skoog I, Waern M. A cross-cultural adaptation of the ICECAP-O: Test–retest reliability and item relevance in Swedish 70-year-olds. Societies. 2016;6(4):30. [Google Scholar]
- 87.Sarabia-Cobo CM, Paras-Bravo P, Amo-Setien FJ, Alconero-Camarero AR, Saenz-Jalon M, Torres-Manrique B, et al. Validation of the Spanish Version of the ICECAP-O for nursing home residents with dementia. PLoS ONE. 2017 doi: 10.1371/journal.pone.0169354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Coast J, Flynn TN, Natarajan L, Sproston K, Lewis J, Louviere JJ, et al. Valuing the ICECAP capability index for older people. Social Science and Medicine. 2008;67(5):874–882. doi: 10.1016/j.socscimed.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 89.Engel L, Chudyk AM, Ashe MC, McKay HA, Whitehurst DGT, Bryan S. Older adults’ quality of life —exploring the role of the built environment and social cohesion in community-dwelling seniors on low income. Social Science and Medicine. 2016;164:1–11. doi: 10.1016/j.socscimed.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 90.Hackert MQN, van Exel J, Brouwer WBF. Does the ICECAP-O cover the physical, mental and social functioning of older people in the UK? [Article] Quality of Life Research. 2019;28(3):761–770. doi: 10.1007/s11136-018-2042-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Horwood J, Sutton E, Coast J. Evaluating the face validity of the ICECAP-O capabilities measure: A “Think Aloud” study with hip and knee arthroplasty patients. Applied Research in Quality of Life. 2014;9(3):667–682. [Google Scholar]
- 92.Makai P, Brouwer WBF, Koopmanschap MA, Nieboer AP. Capabilities and quality of life in Dutch psycho-geriatric nursing homes: An exploratory study using a proxy version of the ICECAP-O. Quality of Life Research. 2012;21(5):801–812. doi: 10.1007/s11136-011-9997-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Milte R, Crotty M, Miller MD, Whitehead C, Ratcliffe J. Quality of life in older adults following a hip fracture: An empirical comparison of the ICECAP-O and the EQ-5D-3 L instruments. Health and Quality of Life Outcomes. 2018 doi: 10.1186/s12955-018-1005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mitchell PM, Roberts TE, Barton PM, Pollard BS, Coast J. Predicting the ICECAP-O capability index from the WOMAC osteoarthritis index: Is mapping onto capability from condition-specific health status questionnaires feasible? Medical Decision Making. 2013;33(4):547–557. doi: 10.1177/0272989X12475092. [DOI] [PubMed] [Google Scholar]
- 95.Parsons N, Griffin XL, Achten J, Costa ML. Outcome assessment after hip fracture: Is EQ-5D the answer? [Article] Bone and Joint Research. 2014;3(3):69–75. doi: 10.1302/2046-3758.33.2000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xin Y, Lewsey J, Gray R, Clarke CE, Coast J, Rick C, et al. Too broad to be sensitive? Exploring the responsiveness of the ICECAP-O capability wellbeing measure compared to the EQ-5D-3L to the change of clinical and QoL aspects in people with parkinson’s. Value in Health. 2017;20(9):A763. [Google Scholar]
- 97.Comans TA, Scuffham PA, Gray L, Peel N. Utility values for use in health care decision making for older frail adults. Value in Health. 2012;15(7):A639. [Google Scholar]
- 98.Looman WM, Fabbricotti IN, Huijsman R. The short-term effects of an integrated care model for the frail elderly on health, quality of life, health care use and satisfaction with care. International Journal of Integrated Care. 2014 doi: 10.5334/ijic.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ratcliffe J, Lester LH, Couzner L, Crotty M. An assessment of the relationship between informal caring and quality of life in older community-dwelling adults - more positives than negatives? Health and Social Care in the Community. 2013;21(1):35–46. doi: 10.1111/j.1365-2524.2012.01085.x. [DOI] [PubMed] [Google Scholar]
- 100.Coast J, Huynh E, Kinghorn P, Flynn T. Complex valuation: Applying ideas from the complex intervention framework to valuation of a new measure for end-of-life care. PharmacoEconomics. 2016;34(5):499–508. doi: 10.1007/s40273-015-0365-9. [DOI] [PubMed] [Google Scholar]
- 101.Huynh E, Coast J, Rose J, Kinghorn P, Flynn T. Values for the ICECAP-Supportive Care Measure (ICECAP-SCM) for use in economic evaluation at end of life. Social Science and Medicine. 2017;189:114–128. doi: 10.1016/j.socscimed.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 102.Greco G, Skordis-Worrall J, Mills A. Development, validity, and reliability of the women’s capabilities index. Journal of Human Development and Capabilities. 2018;19(3):271–288. doi: 10.1080/19452829.2017.1422704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Baumgardt J, Daum M, Von Dem Knesebeck O, Speck A, Röh D. Assess capabilities among chronically mentally ill people: First test results on a draft german version of the OxCAP-MH as Part of the BAESCAP Study. Psychiatrische Praxis. 2018;45(3):140–147. doi: 10.1055/s-0043-101903. [DOI] [PubMed] [Google Scholar]
- 104.van Leeuwen KM, Malley J, Bosmans JE, Jansen AP, Ostelo RW, van der Horst HE, Netten A. What can local authorities do to improve the social care-related quality of life of older adults living at home? Evidence from the Adult Social Care Survey. Health and Place. 2014;29:104–113. doi: 10.1016/j.healthplace.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 105.Shiroiwa T, Moriyama Y, Nakamura-Thomas H, Morikawa M, Fukuda T, Batchelder L, et al. Development of japanese preference weight for the adult social care outcomes toolkit (ASCOT) SCT4. Value in Health. 2018;21:S323. doi: 10.1007/s11136-019-02287-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.van Leeuwen KM, Bosmans JE, Jansen APD, Rand SE, Towers AM, Smith N, et al. Dutch translation and cross-cultural validation of the Adult Social Care Outcomes Toolkit (ASCOT) Health and Quality of Life Outcomes. 2015 doi: 10.1186/s12955-015-0249-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tang C, Xiong Y, Wu H, Xu J. Adaptation and assessments of the Chinese version of the ICECAP-A measurement. Health and Quality of Life Outcomes. 2018 doi: 10.1186/s12955-018-0865-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Linton MJ, Mitchell PM, Al-Janabi H, Schlander M, Richardson J, Iezzi A, et al. Comparing the german translation of the ICECAP-A capability wellbeing measure to the original english version: Psychometric properties across healthy samples and seven health condition groups. Applied Research in Quality of Life. 2018 [Google Scholar]
- 109.Handels RLH, Sköldunger A, Bieber A, Edwards RT, Gonçalves-Pereira M, Hopper L, et al. Quality of life, care resource use, and costs of dementia in 8 European countries in a cross-sectional cohort of the actifcare study. Journal of Alzheimer’s Disease. 2018;66(3):1027–1040. doi: 10.3233/JAD-180275. [DOI] [PubMed] [Google Scholar]
- 110.Coast J, Bailey C, Canaway A, Kinghorn P. Measuring and valuing outcomes for care at the end of life: The capability approach. In: Round J, editor. Care at the end of life: An economic perspective. Cham: Springer; 2016. pp. 89–101. [Google Scholar]
- 111.Bray N, Brand A, Taylor J, Hoare Z, Dickinson C, Edwards RT. Portable electronic vision enhancement systems in comparison with optical magnifiers for near vision activities: An economic evaluation alongside a randomized crossover trial. Acta Ophthalmologica. 2017;95(5):e415–e423. doi: 10.1111/aos.13255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Goranitis I, Coast J, Day E, Copello A, Freemantle N, Frew E. Maximizing health or sufficient capability in economic evaluation? A methodological experiment of treatment for drug addiction. Medical Decision Making. 2017;37(5):498–511. doi: 10.1177/0272989X16678844. [DOI] [PubMed] [Google Scholar]
- 113.Henderson C, Knapp M, Fernandez JL, Beecham J, Hirani SP, Cartwright M, et al. Cost effectiveness of telehealth for patients with long term conditions (Whole Systems Demonstrator telehealth questionnaire study): Nested economic evaluation in a pragmatic, cluster randomised controlled trial. BMJ. 2013;346:f1035. doi: 10.1136/bmj.f1035. [DOI] [PubMed] [Google Scholar]
- 114.Simon, J. K., Korrelboom, N., Kingdon, K., Wykes, D., Phiri, T., van der Gaag, P., Baksh, M., Steel, M. F. (unpublished manuscript). Cost-effectiveness of positive memory training (PoMeT) for the treatment of depression in schizophrenia: A within-trial economic evaluation. [DOI] [PMC free article] [PubMed]
- 115.Botes R, Vermeulen KM, Ranchor AV, Buskens E. Functional health state description and valuation by people aged 65 and over: A pilot study. BMC Geriatrics. 2018 doi: 10.1186/s12877-018-0711-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Khan MA, Richardson J. Variation in the apparent importance of health-related problems with the instrument used to measure patient welfare. Quality of Life Research. 2018;27(11):2885–2896. doi: 10.1007/s11136-018-1956-7. [DOI] [PubMed] [Google Scholar]
- 117.Simon J, Łaszewska A, Leutner E, Spiel G, Churchman D, Mayer S. Cultural and linguistic transferability of the multi-dimensional OxCAP-MH capability instrument for outcome measurement in mental health: The German language version. BMC Psychiatry. 2018 doi: 10.1186/s12888-018-1762-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Forder, J., Jones, K., Glendinning, C., Caiels, J., Welch, E., Baxter, K., et al. (2012). Evaluation of the personal health budget pilot programme.
- 119.Glendinning, C., Challis, D., Fernández, J. L., Jacobs, S., Jones, K., Knapp, M., et al. (2008). Evaluation of the Individual Budgets Pilot Programme.