Abstract
Needle arthroscopic procedures of the knee offer potential advantages over standard arthroscopic procedures. The small size of the instruments allows for surgery without the use of a scalpel or suture, potentially decreased recovery times, and potentially reduced complication rates compared with traditional arthroscopy. In some patients, the procedure can be performed without the use of either general anesthesia or sedation. The purpose of this article is to provide a standardized technique guide for needle arthroscopic partial medial meniscectomy under local anesthesia.
Partial medial meniscectomy is an effective form of management for symptomatic medial meniscus tears and tears involving the posterior root with minimal to no degenerative joint disease, joint space narrowing, and preserved joint alignment.1,2 Traditionally, this procedure is performed with standard arthroscopic instruments with the patient under general anesthesia. While this commonly performed procedure is considered safe and effective, there is still a complication rate of 0.9% to 2.0% for major adverse events, including deep vein thrombosis, pulmonary embolism, infection, or need for reoperation. These complications are primarily observed when concomitant with steroid use, diabetes, procedure time >90 minutes, American Society of Anesthesiologists classification ≥2, and dialysis-dependent renal disease.3 Using only local anesthetic for knee arthroscopy can decrease recovery time and reduce postoperative pain but historically is limited given the size of the instrumentation, patient discomfort experienced, the potential need for conversion to general anesthesia, and extent of the pathology identified.4, 5, 6 New orthopaedic equipment has been released to allow for in-office imaging through the use of needle cameras.7,8 Recent research findings indicate needle arthroscopy, when used diagnostically, as being superior in accuracy of diagnosis compared with magnetic resonance imaging (MRI) for meniscal tears, chondral defects, and other nonligamentous pathology. This is potentially advantageous to patients by reducing time from presentation to diagnosis, improved diagnostic accuracy, and avoidance of the need for advanced imaging.9, 10, 11, 12, 13 It is anticipated that with these recently documented advantages from both a diagnostic and cost-effectiveness standpoint, further therapeutic advantages may be identified in future studies with regards to the use of small-bore arthroscopic instrumentation using only local anesthetics for the definitive management of meniscus tears. The purpose of this article is to share the local anesthetic protocol and technique to perform a partial meniscectomy using needle arthroscopic instrumentation under local anesthetics.
Technique (With Video Illustration)
After obtaining informed consent from the patient, the operating room is prepared for needle arthroscopy of the knee (Video 1). The disposable kit is prepared on a sterile field, including a 20-cc syringe equal mixture of 1% lidocaine with epinephrine/0.25% bupivacaine, a separate 20-cc syringe with only 0.25% bupivacaine, a saline-filled 60-cc syringe, Chlorhexidine scrub, the needle arthroscopy (NanoScope, Arthrex, Naples, FL) hand piece, a skin marker, pump tubing, and 2 band aids. Further equipment, such as the needle-sized arthroscopic baskets and shaver (Arthrex, Naples, FL) are placed on the operative field as needed. The display from the needle arthroscope is placed in easy sight for the physician and also the patient should they wish to view the procedure.
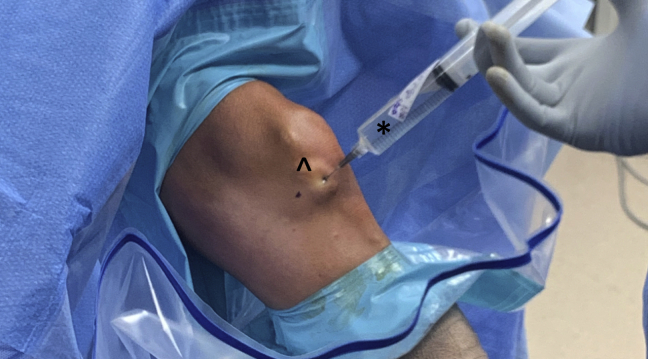
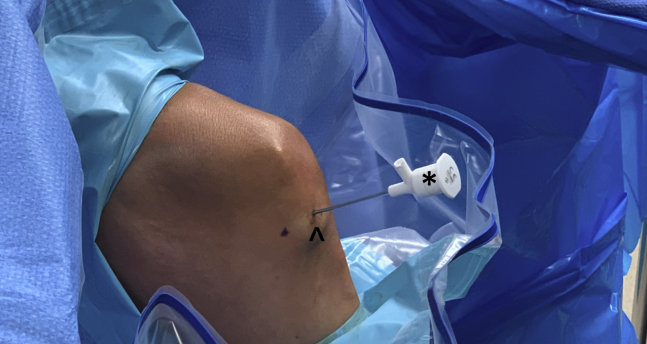
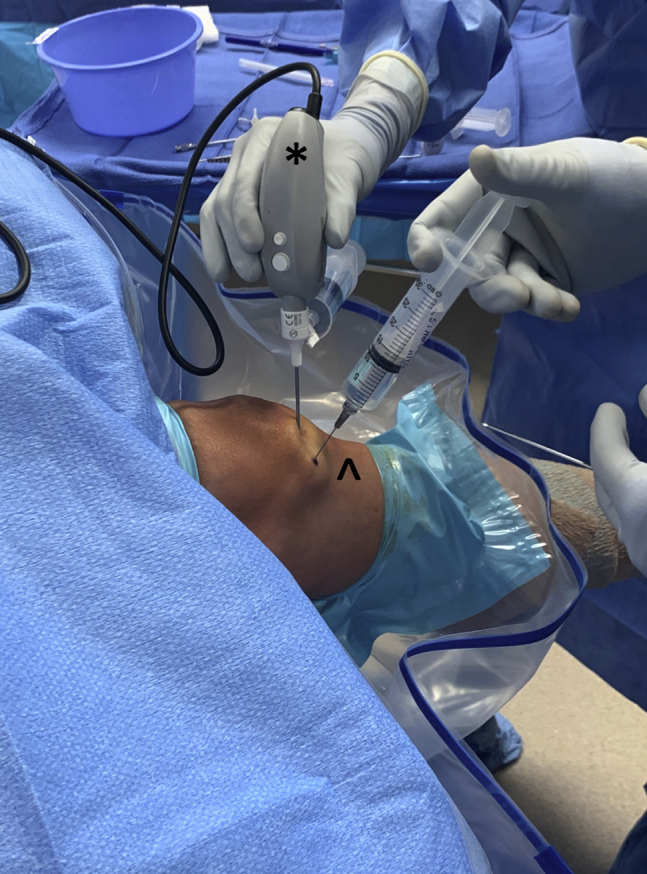
The patient is placed supine on the operating table with the operative lower extremity supported in an arthroscopic leg holder. The limb is prepped with ChloraPrep scrub (Becton, Dickinson and Company, Franklin Lakes, NJ) and then draped in standard sterile fashion to allow for access to and manipulation of the surgical site. A stockinette is placed over the foot and ankle and secured in place just distal to the tibial tuberosity with Coban wrap. The portal sites are marked on the operative extremity. These include primary medial and lateral portals, which are positioned just above the joint line 1 cm medial and lateral to the edge of the patella tendon respectively. Accessory working portals are marked at the joint line 1 to 2 cm medial to the standard medial portal and 1 to 2 cm lateral to the standard lateral portal. The 20-mL syringe with a 25-gauge needle is used to infiltrate 10 mL of the mixed local anesthetic to each portal site and the surrounding capsule to anesthetize the area (Fig 1). Subsequently, the 20 cc of 0.25% bupivacaine is then injected intra-articularly (Fig 2). The needle arthroscope is connected to the viewing tablet in sterile fashion, and a 60-mL syringe of sterile saline is attached to the inflow port of the needle arthroscopy hand piece. The arthroscopy needle is then inserted into the knee joint through the medial portal site with a posterior and lateral trajectory aimed at the intercondylar notch (Fig 3). Once the joint is entered, the needle sheath is removed to allow visualization for the optic scope. The arthroscope has a 0° viewing angle but 120° field of view. Saline can be injected to the joint with the 60-mL saline syringe to distract the joint space and remove obstructing tissue blocking the arthroscope.
Fig 1.
The 20-mL syringe (*) with a 25-gauge needle used to infiltrate 10 mL of the mixed local anesthetic to each portal site (ˆ) and the surrounding capsule to anesthetize the area of the left knee in a supine position.
Fig 2.
Intra-articular injection of 20 cc of 0.25% bupivacaine through the use of a syringe with a spinal needle to achieve intra-articular anesthesia of the left knee in the supine position.
Fig 3.
The needle arthroscope (*) is inserted into the knee joint through the primary medial portal site (ˆ) with a posterior and lateral trajectory aimed at the intercondylar notch of the left knee in a supine position.
After insertion of the scope, a standard diagnostic arthroscopy is performed. The diagnostic procedure is started by first examining the patellofemoral joint to include the articular surface of the trochlear groove of the femur and the medial and lateral facets of the patella for any signs of chondral wear and inflammation. The scope and operative limb are then manipulated to allow visualization of the lateral gutter to assess the lateral joint capsule and the deep fibers of the lateral collateral ligament, as well as the lateral borders of the lateral femoral condyle and tibial plateau. The scope is then placed in the lateral compartment of the joint to assess the lateral meniscus for tears, the lateral femoral condyle, and lateral tibial plateau for any defects or signs of chondral wear and the deep fibers of the popliteus tendon posteriorly. Next, the intercondylar compartment is visualized to assess the anterior and posterior cruciate ligaments, along with the anterior and posterior meniscofemoral ligaments, for any signs of fraying or tearing.
The scope is then switched to an established medial cannula for further visualization of the medial compartment. The medial meniscus, femoral condyle, and tibial plateau are inspected in the same manner as the lateral compartment. The scope is then taken to the medial gutter to visualize the deep fibers of the medial collateral ligament and the medial borders of both the medial femoral condyle and tibial plateau (Fig 4). This diagnostic process is similar to the standardized approach described by McMillan et al.11 Upon examination and identification of meniscal pathology, the accessory medial portal is established with the needle trochar-cannula. The camera may be switched in between the standard and accessory medial portals as needed to better visualize and address the pathology and fluid pump and inflow connected to the camera system. The small-sized arthroscopy basket (NanoBiter; Arthrex) is then inserted through the accessory medial portal and used until the meniscal tear is balanced and smoothed (Fig 5 A and B). An arthroscopic shaver is then placed in the same portal to clear the joint of meniscal debris and further refine the meniscus tear (Fig 6). Once the procedure has been completed, an empty 60-mL syringe is placed into the inflow port of the handheld device to aspirate the saline that was injected into the joint during the procedure to aid with distraction and visualization. It is important to aspirate as much saline as possible out of the joint before the removal of the device to minimize the patient’s post-procedure discomfort (Table 1). The needle arthroscope is then removed from the joint and the needle site is covered with band-aids or a compressive dressing. Following the placement of dressings, removal of sterile drapes and transport to the postoperative holding area, the patient is able then to range the knee and weight bear as tolerated and is instructed to ice the area and take nonsteroidal anti-inflammatory drugs as needed.
Fig 4.
The needle arthroscope (*) is inserted into the knee joint through the primary medial portal site with a posterior and lateral trajectory aimed at the intercondylar notch of the left knee in a supine position. An additional 0.25% bupivacaine is then injected into the accessory medial portal (ˆ).
Fig 5.
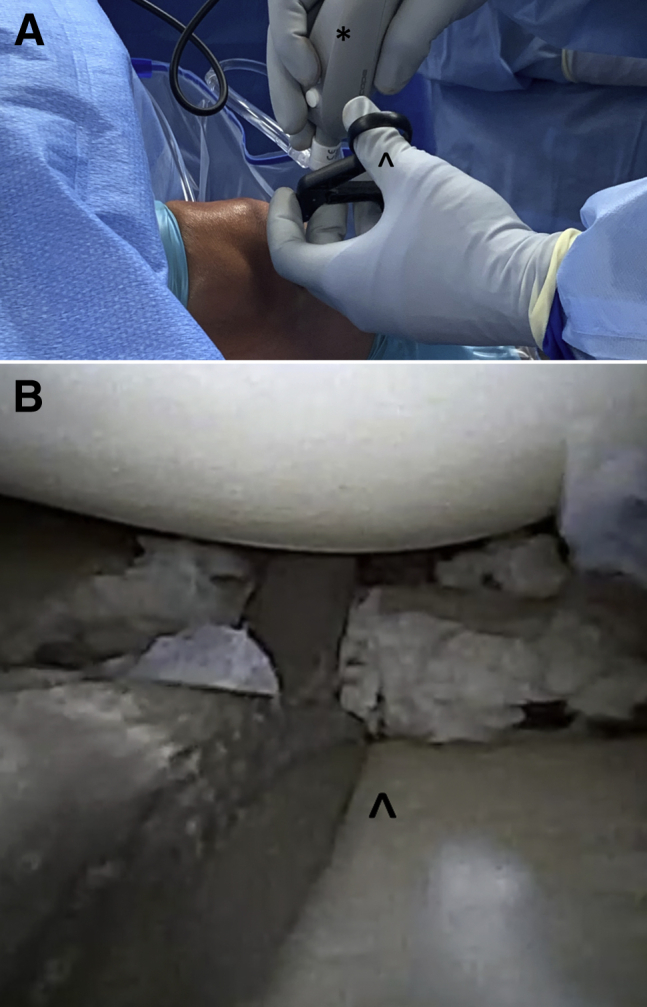
(A) The needle-sized arthroscopy basket (ˆ) (NanoBiter; Arthrex) is inserted through the accessory medial portal under visualization of the needle scope (*) to perform a partial medial meniscectomy of this left knee in the supine position. (B) Arthroscopic view of a partial medial meniscectomy using the needle-sized arthroscopic basket (ˆ) (NanoBiter) of the left knee in the supine position.
Fig 6.

The arthroscopic shaver (ˆ) is placed under visualization of the needle scope (*) through the accessory medial portal site to clear the joint of meniscal debris and further refine the meniscus tear during partial medial meniscectomy of the left knee in the supine position.
Table 1.
Pearls and Pitfalls of Partial Medial Meniscectomy Using Needle Arthroscopy and a Standardized Local Anesthetic Protocol
| Criteria | Pearls | Pitfalls |
|---|---|---|
| Patient comfort | Ensure patients are comfortable, educated, and have expectations on the process of the procedure. Additional local anesthetic or general can be used if needed. | Patient anxiety can be increased upon entering the operating or procedure rooms. Lack of education on the procedure and process and increase this anxiety. |
| Bleeding | Bleeding can impede visualization and be challenging to treat. Minimize resection, especially of the fat pad. Using epinephrine can decrease bleeding encountered. | Excessive resection of tissue can cause increased bleeding. |
| Compartment access | Use of the instrumentation across compartments can be challenging. Accessory portals in the same compartment can alleviate these challenges. | Spacing accessory compartment portals too close can impede visualization. |
Discussion
Our technique demonstrates the use of needle arthroscopy instrumentation to perform a partial meniscectomy with the patient under local anesthesia. Using only local anesthetics has demonstrated decreased recovery time and postoperative pain with equivocal patient satisfaction when compared with performing the same technique under general anesthesia.4, 5, 6 Forssblad and Weidenhielm5 also found no difference in the rate of repeat arthroscopy in patients who had undergone primary knee arthroscopic procedures under local anesthetics compared with general anesthesia. The use of 0.25% bupivacaine has long been established as a safe and effective form of local anesthesia, with more recent studies examining the effectiveness of adjuvants to the commonly used 0.25% bupivacaine both applied both intra-articularly and peri-incisional.14, 15, 16 Patel et al.17 acknowledge that arthroscopic visualization is the gold standard for diagnosis of intra-articular knee pathology; thus, most of the focus of needle arthroscopy has been placed on its use as a diagnostic tool thus far. Multiple studies have reported that in-office diagnostic needle arthroscopy is equally accurate and safe as compared to standard diagnostic arthroscopic procedures, and is superior compared to MRI in its ability to diagnose intra-articular, non-ligamentous knee pathology.18,19 MRI may be limited by the presence of previously placed orthopaedic hardware or scar tissue causing distortion of the images produced.10 Patel et al.17 report a false-positive finding of meniscal pathology in 20% of MRI interpretations, as well as false-negative interpretations in 10%. Amin et al.12 recently supported this reporting needle arthroscopy of the knee was more cost efficient with similar outcomes when compared with MRI for the diagnosis of meniscus pathology. Voigt et al.20 compared MRI with an office-based diagnostic needle arthroscopy of the knee and a cost analysis determined that needle arthroscopy has the potential to save $177 million annually in health care costs for patients presenting with medial meniscus pathology. The economic impact of using needle arthroscopy for treating conditions of the knee has not yet been studied, but significant savings may exist in the reduction in imaging costs, costs for sterile processing for many instruments, the elimination of general anesthesia, reduced postanesthesia care unit recovery time, reduced staff requirement, and reduced overall recovery time for the patient.
There are limitations in performing partial meniscectomy using needle arthroscopy (Table 2). A primary limitation to the performance of a diagnostic knee arthroscopy and partial meniscectomy using needle arthroscopic instrumentation is ensuring the patient is not just obtaining a good outcome but also a good experience. The operating room setting and an increased length of the procedure can increase anxiety for the patient, and it is crucial that the patient is fully prepared and educated before the procedure. Another limitation is the instrumentation. Currently, there is limited instrumentation available to perform these procedures, and some pathology cannot be treated with the available small-bore arthroscopic tools. There is always also the risk that other intra-articular pathology is identified at the time of surgery that requires more extensive treatment, and conversion to general anesthesia is necessary. We recommend that further studies be performed comparing needle arthroscopic procedures with standard arthroscopic procedures, as the scope of this treatment modality continues to broaden.
Table 2.
Risks and Limitations of Partial Medial Meniscectomy and Methods to Minimize These Risks
| Risks/Complication | Ways to Minimize This Risk |
|---|---|
| Patient anxiety before procedure | Preoperative education and patient preparation is essential to identifying the right patient candidate. |
| Patient discomfort during the procedure | Always have additional anesthetic available and be prepared to convert to general anesthetic if needed. |
| Additional intraoperative pathology identified | There are currently limitations to needle instrumentation. Preoperative education on potential other procedures needed is essential. |
| Inability to effectively treat with needle instrumentation | Always have standard arthroscopic instruments available in case they are needed to address specific pathology. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.D. and E.M. are consultants with Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates the use of needle arthroscopy and needle instruments to perform a partial medial meniscectomy of the left knee in the supine position using a standardized local anesthetic protocol.
References
- 1.Kim J-Y, Bin S-I, Kim J-M, et al. Partial meniscectomy provides the favorable outcomes for symptomatic medial meniscus tear with an intact posterior root [published online July 22, 2019]. Knee Surg Sport Traumatol Arthrosc. 10.1007/s00167-019-05634-9. [DOI] [PubMed]
- 2.Lee B.S., Bin S.I., Kim J.M., Park M.H., Lee S.M., Bae K.H. Partial meniscectomy for degenerative medial meniscal root tears shows favorable outcomes in well-aligned, nonarthritic knees. Am J Sports Med. 2019;47:606–611. doi: 10.1177/0363546518819225. [DOI] [PubMed] [Google Scholar]
- 3.Degen R.M., Lebedeva Y., Birmingham T.B. Trends in knee arthroscopy utilization: A gap in knowledge translation. Knee Surg Sport Traumatol Arthrosc. 2020;28:439–447. doi: 10.1007/s00167-019-05638-5. [DOI] [PubMed] [Google Scholar]
- 4.Barroso Rosa S., James D., Matthews B.D. Is knee arthroscopy under local anaesthetic a patient-friendly technique? A prospective controlled trial. Eur J Orthop Surg Traumatol. 2016;26:633–638. doi: 10.1007/s00590-016-1799-2. [DOI] [PubMed] [Google Scholar]
- 5.Forssblad M., Weidenhielm L. Knee arthroscopy in local versus general anaesthesia the incidence of rearthroscopy. Knee Surg Sport Traumatol Arthrosc. 1999;7:323–326. doi: 10.1007/s001670050171. [DOI] [PubMed] [Google Scholar]
- 6.Lintner S., Shawen S., Lohnes J., Levy A., Garrett W. Local anesthesia in outpatient knee arthroscopy: A comparison of efficacy and cost. Arthroscopy. 1996;12:482–488. doi: 10.1016/s0749-8063(96)90044-4. [DOI] [PubMed] [Google Scholar]
- 7.Deirmengian CA, Dines JS, Vernace JV, Schwartz MS, Creighton RA, Gladstone JN. Use of a small-bore needle arthroscope to diagnose intra-articular knee pathology: Comparison with magnetic resonance imaging [published online February 4, 2018]. Am J Orthop (Belle Mead NJ). 10.12788/ajo.2018.0007. [DOI] [PubMed]
- 8.Voigt JD, Mosier M, Huber B. In-office diagnostic arthroscopy for knee and shoulder intra-articular injuries its potential impact on cost savings in the United States [published online May 5, 2014]. BMC Health Serv Res. 10.1186/1472-6963-14-203. [DOI] [PMC free article] [PubMed]
- 9.Zhang K., Crum R.J., Samuelsson K., Cadet E., Ayeni O.R., de Sa. In-office needle arthroscopy: A systematic review of indications and clinical utility. Arthroscopy. 2019;35:2709–2721. doi: 10.1016/j.arthro.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 10.Chapman GL, Amin NH. The benefits of an in-office arthroscopy in the diagnosis of unresolved knee pain [published online January 21, 2018]. Case Rep Orthop. 10.1155/2018/6125676. [DOI] [PMC free article] [PubMed]
- 11.McMillan S., Schwartz M., Jennings B., Faucett S., Owens T., Ford E. In-office diagnostic needle arthroscopy: Understanding the potential value for the US healthcare system. Am J Orthop (Belle Mead NJ) 2017;46:252–256. [PubMed] [Google Scholar]
- 12.Amin N., McIntyre L., Carter T., Xerogeanes J., Voigt J. Cost-effectiveness analysis of needle arthroscopy versus magnetic resonance imaging in the diagnosis and treatment of meniscal tears of the knee. Arthroscopy. 2019;35:554–562. doi: 10.1016/j.arthro.2018.09.030. e13. [DOI] [PubMed] [Google Scholar]
- 13.McMillan S., Saini S., Alyea E., Ford E. Office-based needle arthroscopy: A standardized diagnostic approach to the knee. Arthrosc Tech. 2017;6:e1119–e1124. doi: 10.1016/j.eats.2017.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaeding C.C., Hill J.A., Katz J., Benson L. Bupivacaine use after knee arthroscopy: Pharmacokinetics and pain control study. Arthroscopy. 1990;6:33–39. doi: 10.1016/0749-8063(90)90094-t. [DOI] [PubMed] [Google Scholar]
- 15.Moeen S.M., Ramadan I.K., Elkady H.A. Dexamethasone and dexmedetomidine as an adjuvant to intraarticular bupivacaine for postoperative pain relief in knee arthroscopic surgery: A randomized trial. Pain Physician. 2017;20:671–680. [PubMed] [Google Scholar]
- 16.Devi M.M., Gupta S., Amaravathi R., Udupa S., Hedge A., Ghosh S. Comparison of intra-articular dexmedetomidine and magnesium in postoperative pain. https://clinicaltrials.gov/show/NCT03479216 Accessed September 8, 2019. [DOI] [PMC free article] [PubMed]
- 17.Patel K.A., Hartigan D.E., Makovicka J.L., Dulle D.L., Chhabra A. Diagnostic evaluation of the knee in the office setting using small-bore needle arthroscopy. Arthrosc Tech. 2017;7:e17–e21. doi: 10.1016/j.eats.2017.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xerogeanes J.W., Safran M.R., Huber B., Mandelbaum B.R., Robertson W., Gambardella R.A. A prospective multi-center clinical trial to compare efficiency, accuracy and safety of the visionscope imaging system compared to MRI and diagnostic arthroscopy. Orthop J Sport Med. 2014;2 2325967114S00100(suppl 2) [Google Scholar]
- 19.Gill T.J., Safran M., Mandelbaum B., Huber B., Gambardella R., Xerogeanes J. A prospective, blinded, multicenter clinical trial to compare the efficacy, accuracy, and safety of in-office diagnostic arthroscopy with magnetic resonance imaging and surgical diagnostic arthroscopy. Arthroscopy. 2018;34:2429–2435. doi: 10.1016/j.arthro.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Voigt J.D., Mosier M., Huber B. Diagnostic needle arthroscopy and the economics of improved diagnostic accuracy: A cost analysis. Appl Health Econ Health Policy. 2014;12:523–535. doi: 10.1007/s40258-014-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the use of needle arthroscopy and needle instruments to perform a partial medial meniscectomy of the left knee in the supine position using a standardized local anesthetic protocol.