Abstract
Background
The covid-19 pandemic has presented unprecedented professional and personal challenges for the oncology community. Under the auspices of the Canadian Association of Medical Oncologists, we conducted an online national survey to better understand the impact of the pandemic on the medical oncology community in Canada.
Methods
An English-language multiple-choice survey, including questions about demographics, covid-19 risk, use of personal protective equipment (ppe), personal challenges, and chemotherapy management was distributed to Canadian medical oncologists. The survey was open from 30 March to 4 April 2020, and attracted 159 responses.
Results
More than 70% of medical oncologists expressed moderate-to-extreme concern about personally contracting covid-19 and about family members or patients (or both) contracting covid-19 from them. Despite that high level of concern, considerable variability in the use of ppe in direct cancer care was reported at the time of this survey, with 33% of respondents indicating no routine ppe use at their institutions and 69% indicating uncertainty about access to adequate ppe. Of the respondents, 54% were experiencing feelings of nervousness or anxiety on most days, and 52% were having feelings of depression or hopelessness on at least some days. Concern about aging parents or family and individual wellness represented the top personal challenges identified. The management of cancer patients has been affected, with adoption of telemedicine reported by 82% of respondents, and cessation of clinical trial accrual reported by 54%. The 3 factors deemed most important for treatment decision-making were
■ cancer prognosis and anticipated benefit from treatment,
■ risk of treatment toxicity during scarce health care access, and
■ patient risk of contracting covid-19.
Conclusions
This report describes the results of the first national survey assessing the impact of the covid-19 on Canadian medical oncologists and how they deliver systemic anticancer therapies. We hope that these data will provide a framework to address the challenges identified.
Keywords: covid-19, camo, surveys, medical oncology
INTRODUCTION
On 11 March 2020, the World Health Organization declared the rapidly spreading novel coronavirus sars-cov-2 to be a pandemic. At that time, 118 countries had reported 118,000 cases of covid-19, the disease associated with the virus. By 11 April, 1,800,791 cases had been reported in 185 countries, with 23,717 cases being reported in Canada1.
Early information indicated that older individuals and those with underlying comorbidities, including cancer, were more vulnerable to severe illness2. Based on more recent data from Hubei, China, patients with cancer who contract covid-19 have been recognized to have outcomes significantly inferior to those in patients with non-cancer conditions, with higher observed mortality [odds ratio (or): 2.88; 95% confidence interval (ci): 1.20 to 6.89; p = 0.02], rates of admission to the intensive care unit (or: 2.38; 95% ci: 1.23 to 4.61; p = 0.01), rates of at least 1 severe or critical symptom (or: 2.60; 95% ci: 1.53 to 4.41; p < 0.01), and likelihood of requiring mechanical ventilation (or: 4.75; 95% ci: 1.60 to 14.41; p = 0.01)3.
The pandemic has presented unprecedented professional and personal challenges for the oncology community as it endeavours to continue to treat patients with cancer while recognizing the high risk for covid-19 and associated severe illness for its members. Cancer care in Canada is accessed through a universal, publicly funded health care system, with oncology care delivered under the governance of individual provinces. We conducted an online survey to better understand the impact of the pandemic on the medical oncology community in Canada.
METHODS
The Canadian Association of Medical Oncologists (camo) is a national specialty society of the Royal College of Physicians and Surgeons of Canada. Membership is representative of certified medical oncologists across the country and is voluntary—that is, a certified medical oncologist can choose to be a member of camo, but is not required to do so. An English-language survey consisting of 23 multiplechoice questions was developed on the SurveyMonkey platform (SurveyMonkey, San Mateo, CA, U.S.A.), including questions about demographics, covid-19 risk, use of personal protective equipment (ppe), personal challenges, and systemic therapy management. An invitation to participate in the survey was circulated by e-mail to practising medical oncologists across Canada through the camo membership (n = 323) and, to extend the reach of the survey, through provincial practice groups within the authors’ network. The survey was open from 30 March to 4 April 2020. Analyses are descriptive, with frequency distributions reported. No formal statistical analyses were planned.
RESULTS
During the 6-day survey window, 159 responses were received. Of the respondents, 60% were camo members, 87% practised in a comprehensive cancer centre, and 13% were in community practice. Table I presents respondent distribution by province and years of practice.
TABLE I.
Respondent characteristics
| Characteristic | Value (%) |
|---|---|
| Practice setting | |
| Comprehensive cancer centre | 87 |
| Community practice, urban | 11 |
| Community practice, rural | 2 |
|
| |
| Years in practice | |
| <5 Years | 25 |
| 5–10 Years | 19 |
| 10–15 Years | 15 |
| >15 Years | 41 |
|
| |
| Province | |
| British Columbia | 26 |
| Alberta | 24 |
| Saskatchewan or Manitoba | 9 |
| Ontario | 28 |
| Quebec | 6 |
| Newfoundland and Labrador | 3 |
| Maritimesa | 4 |
New Brunswick, Nova Scotia, Prince Edward Island.
Perceived Risk of COVID-19
Only 1 respondent (0.6%) reported a confirmed diagnosis of covid-19. A covid-19 exposure was reported by 7 respondents [4% (3 at work, 4 outside of work)], and 5 respondents (3%) were in self-isolation at the time of the survey. Of the responding medical oncologists, 79% were moderately-to-extremely concerned about contracting covid-19, 82% were moderately-to-extremely concerned that a family member would contract covid-19 from them, and 71% were moderately-to-extremely concerned that a patient would contract covid-19 from them.
Personal Protective Equipment
At the time of the survey, 33% of medical oncologists reported that no form of ppe was being routinely used in clinical practice. Another 13% reported very sporadic use of ppe, often citing that protective measures outside of handwashing and physical distancing (such as a surgical mask) were discouraged in their local institution. Of the remaining 54% who reported routine use of ppe, all specified use of a surgical mask; 52%, gloves; 51%, eye protection; and 28%, use of scrubs or a gown. N95 respirator masks were routinely used by 7 respondents (4%). With respect to ppe access, 69% of medical oncologists were either uncertain or did not believe that they would have adequate access to ppe at work during the course of the pandemic.
Personal Challenges
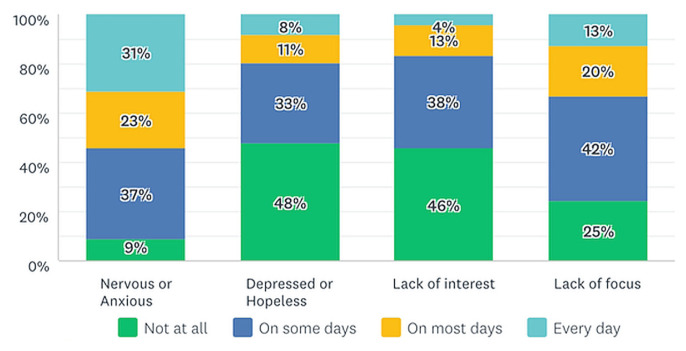
To assess mental well-being, respondents were asked to report the frequency of selected emotions or feelings (Figure 1). Emotions experienced on most days or every day were reported at these frequencies: nervousness or anxiety, 54%; lack of focus or attention, 33%; depression or hopelessness, 19%; and lack of interest, 17%. The 3 top challenges faced by medical oncologists outside of work were concern about aging parents and family members, 60%; personal wellness, 57%; and generalized anxiety, 52%. Concerns about social isolation (27%) and childcare (20%) were less commonly noted, and only 8% reported financial worry. When asked about institutional support and resources, only 39% reported moderate-to-high levels of confidence that their organization would help support them through the pandemic.
FIGURE 1.
Results of survey respondents being asked whether, over the preceding 14 days, they had experienced certain emotions or feelings.
Impact on Cancer Management
Within mere weeks of covid-19 restrictions, 82% of responding medical oncologists reported the use of some form of telemedicine for most of their cancer patients (Figure 2). The forms most commonly used were telephone (100%), videoconferencing (42%), and e-mail (12%). Cancellation or deferral of all follow-up visits was reported by 14%, with 64% reporting cancellation of some visits, and only 22% reporting no change in the frequency of follow-ups. More than half the respondents (59%) expressed moderate-to-extreme concern that their cancer patients would not receive adequate health care if they became seriously ill from a non-covid illness.
FIGURE 2.
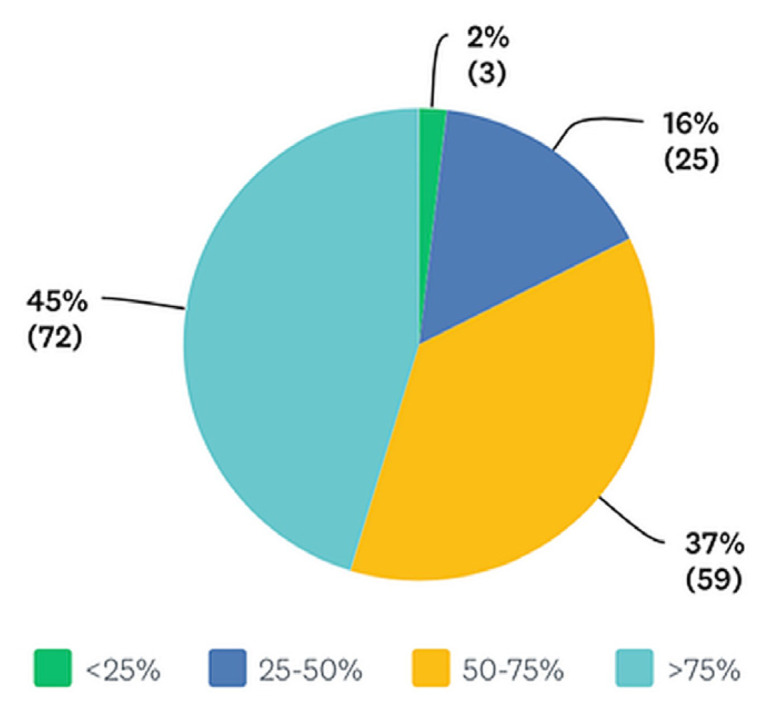
Results of survey respondents being asked about the proportion of their cancer patients now being managed by some form of telemedicine.
Accrual to cancer clinical trials in Canada was significantly affected by covid-19, with 54% of respondents reporting complete cessation of new patient accrual at their centres, and 35% reporting new patient accrual restrictions affecting only selected clinical trials.
With respect to treatment allocation and decisionmaking, 26% of responding medical oncologists reported no changes in the current chemotherapy management of their patients. Changes in treatment plans for a few patients (<20%) were reported by 38%; for some patients (20%–40%), by 25%; and for many patients (>40%), by less than 10%. Respondents were then asked to rank the relative importance of the factors that they would consider when changing a chemotherapy treatment plan during the covid-19 pandemic (Table II). The 3 factors deemed most important for treatment decision-making were
TABLE II.
Top factors in chemotherapy treatment decision-making, ranked
| Factor | Rank order (%)a | Combined rank score | |||
|---|---|---|---|---|---|
| 1–2 | 3–4 | 5–6 | 7–9 | ||
| Cancer prognosis and anticipated treatment benefit | 60 | 26 | 11 | 3 | 7.50 |
| Risk of treatment toxicity during scarce health care access | 35 | 30 | 22 | 13 | 6.19 |
| Patient risk of getting COVID-19 | 33 | 30 | 21 | 16 | 6.05 |
| Presence of other comorbidities | 16 | 31 | 35 | 18 | 5.36 |
| Patient preference | 17 | 24 | 24 | 34 | 4.96 |
| Patient age | 10 | 24 | 37 | 29 | 4.65 |
| Demand on centre or hospital resources | 15 | 19 | 23 | 43 | 4.46 |
| Institutional policy | 15 | 11 | 14 | 60 | 3.57 |
| Patient distance from cancer centre | 0 | 4 | 13 | 83 | 2.26 |
Most important (1) to least important (9).
■ cancer prognosis and anticipated benefit from treatment,
■ risk of treatment toxicity during scarce access to health care, and
■ patient risk of contracting covid-19.
Demand on centre resources, institutional policy, and patient distance from the cancer centre were identified as least important. Finally, 45% of respondents believed that covid-19–related restrictions would continue to affect their practice for at least another 18 weeks or more.
DISCUSSION
Our survey was conducted during the first 4 weeks of covid-19 restrictions in Canada and provides an early description of the Canadian medical oncologist experience.
Most medical oncologists (>70%) expressed moderate-to-extreme concern about personally contracting covid-19 and about family members or patients (or both) contracting covid-19 from them. There remains considerable variability in the use of ppe by medical oncologists in cancer care, with approximately one third of medical oncologists reporting no routine use of ppe at the time of the present survey. The most commonly used ppe during direct patient care included surgical masks with eye protection and gloves. Almost 70% of surveyed medical oncologists are concerned about adequate access to ppe during the pandemic. That sentiment is consistent with the results of a recent Canadian Medical Association survey conducted between 30 and 31 March 2020, in which 3 of 4 physicians were uncertain about access to a supply of ppe4. Continued advocacy for increased efforts both to procure ppe and to keep health care workers apprised of the stock of supplies is encouraged.
When considering coping strategies, the covid-19 pandemic has often been described as a marathon, not a sprint. It is anticipated that physicians will experience escalating stress during this extraordinary time. Even in this early phase of the pandemic, 54% of respondents were already experiencing feelings of nervousness or anxiety on most days within the 2 weeks preceding the survey, and 52% were experiencing feelings of depression or hopelessness on at least some days. Personal wellness was reported by 57% as one of their biggest personal challenges during this time, and 61% did not feel confident that their institution would support them during this time. Physician burnout was already a recognized concern among oncologists before the advent of covid-195. These data highlight the need for early intervention strategies to proactively support personal and mental well-being, and to build resilience in the oncology medical community.
Oncologists must now face the dilemma of balancing the recognized increased risk of serious covid-19 illness in cancer patients against the downstream consequences of deciding to modify, delay, or cancel systemic therapy6. Not surprisingly, the highest-ranked factor influencing treatment decision-making by our survey respondents was the expected prognosis of cancer and the potential benefit from systemic treatment. That result is consistent with a framework proposed by Hanna et al.7 for prioritizing cancer treatment during the pandemic, which is based largely on therapeutic intent and treatment benefit.
Limitations of our survey include underrepresentation from certain provinces, particularly Quebec (being a French-language province), and from medical oncologists in community or rural practices. We acknowledge that the present work represents a cross-sectional description at a single time point during a highly dynamic situation. Hence, it is our intent to conduct serial surveys during the course of the pandemic to assess for temporal trends and to describe the evolution of the impact of covid-19 on cancer care in Canada. Future surveys will be disseminated in English and French.
SUMMARY
This report describes the results of the first national survey assessing the impact of the covid-19 pandemic on Canadian medical oncologists and how they deliver systemic cancer therapies. We hope that these data will provide a framework to help cancer organizations proactively address the challenges identified. The Canadian Association of Medical Oncologists is committed to supporting its membership and cancer patients through these difficult times. Given that the landscape of, and information about, covid-19 and cancer is rapidly evolving, camo has created an online repository of resources for medical oncologists (https://camo-acom.ca/COVID-19-Resources) and will continue to monitor the concerns of medical oncologists during this pandemic in an effort to better understand and address the changing needs of the community.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) [Web resource] Baltimore, MD: Johns Hopkins University; 2020. [Available at: https://coronavirus.jhu.edu/map.html; cited 11 April 2020] [Google Scholar]
- 2.Guan W, Ni Z, Hu Y, et al. on behalf of the China Medical Treatment Expert Group for covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to sars-cov-2: a multi-center study during the covid-19 outbreak. Cancer Discov. 2020 doi: 10.1158/2159-8290.CD-20-0422. pii:CD-20-0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canadian Medical Association (cma) CMA Rapid Poll on the Supply of Personal Protective Equipment. Ottawa, ON: CMA; 2020. [Available online at: https://www.cma.ca/sites/default/files/pdf/Survey/CMA-Survey-Supply-of-PPE_E.pdf; cited 10 April 2020] [Google Scholar]
- 5.Nguyen TP, Tam VC, Lester RE, et al. Burnout among Canadian oncologists and oncology residents [abstract 6549] J Clin Oncol. 2014;32 doi: 10.1200/jco.2014.32.15_suppl.6549. [Available online at: https://ascopubs.org/doi/abs/10.1200/jco.2014.32.15_suppl.6549; cited 14 April 2020] [DOI] [Google Scholar]
- 6.Lewis MA. Between Scylla and Charybdis—oncologic decision making in the time of covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMp2006588. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Hanna TP, Evans GA, Booth CM. Cancer, covid-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol. 2020 doi: 10.1038/s41571-020-0362-6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]