Abstract
Background:
The role of dietary inflammatory index (DII) in cardiovascular disease (CVD) risk and mortality is still controversial. This systematic review and meta-analysis of cohort studies aimed to evaluate the effect of DII, indicating a pro-inflammatory diet, on the incidence and mortality of CVD.
Methods:
A comprehensive literature search of articles published through August 2019 was performed in Medline, EMBASE, and Web of Science. The pooled relative risks (RRs) and 95% confidence intervals (CIs) for highest vs lowest DII in relation to CVD risk or mortality were estimated using a DerSimonian and Laird random effects model. The heterogeneity among studies was tested using Cochran's Q test and I2 statistic.
Results:
A total of 15 cohort studies were finally included in this meta-analysis. The highest DII score was significantly associated with a higher risk of CVD incidence (RR = 1.41, 95% CI 1.12–1.78) or mortality (RR = 1.31, 95% CI 1.19–1.44), compared with the lowest DII score. There was statistically significant heterogeneity among the studies on the association between DII and CVD mortality (P < .001; I2 = 70.8%). No obvious heterogeneity was observed among the studies on the association between DII and CVD risk (P = .160; I2 = 37.0%). In the sensitivity analysis, exclusion of any single study did not materially alter the pooled RRs.
Conclusion:
The present systematic review and meta-analysis indicates that a higher DII score is related to a higher risk of CVD. Further well-designed prospective cohort or trials are warranted to validate our preliminary findings.
Keywords: cardiovascular disease, dietary inflammatory index, dietary pattern, mortality, risk
1. Introduction
Various studies have been conducted exploring the effect of specific food items, such as red meat and vegetables, on cardiovascular disease (CVD) risk and mortality.[1] A limitation of these studies is that the dietary inter-correlations between nutrients among foods may distort the actual effects.[2] Therefore, there has recently been a shift in the focus from 1 nutrient or food group studies to dietary pattern studies (e.g., Mediterranean Diet, Healthy Eating Index and Alternative Healthy Eating Index).
The dietary inflammatory index (DII) developed and validated by researchers from the University of South Carolina is a novel scoring system to determine dietary inflammatory effect.[3] About 2000 primary research articles published through December 2010 on the association between diet and 6 inflammatory markers, including IL-1b, IL-4, IL-6, IL-10, TNF-a, and C-reactive protein, were screened and reviewed. A total of 45 food parameters have been assigned an inflammatory weight, which reflects the association of each food parameter with at least 1 of the 6 markers.[3] The DII has been validated in various studies worldwide with different measures of inflammatory biomarkers.[4,5,6] Previous studies have indicated that higher DII scores are positively associated with various health outcomes, including breast cancer,[7] colorectal cancer,[8] diabetes,[9] and cardiovascular diseases.[10]
Many epidemiological studies have investigated the association between the DII and CVD risk and mortality with inconsistent results,[11,12,13,14] highlighting the recent interest in investigating this issue. Therefore, the aim of the present study was to systematically evaluate the association between DII and CVD using a meta-analysis approach based on a total of 15 eligible cohort studies.
2. Materials and methods
2.1. Publication search
A comprehensive literature search of articles published through August 2019 was performed in Medline, EMBASE, and Web of Science with the following search algorithm: (“cardiovascular disease” OR “coronary heart disease” OR “ischemic heart disease” OR “myocardial infarction” OR “stroke” OR “heart attack” OR “hypertension”) and (“pro-inflammatory diet” OR “dietary inflammatory index” OR “anti-inflammatory diet” OR “inflammatory potential intake”). The cited references from retrieved articles and reviews/meta-analyses were also examined to identify any additional eligible studies. No publication type and language restrictions were imposed. This systematic review and meta-analysis was planned, performed, and reported according to the standards of quality for reporting meta-analyses.[15] This is a systematic review and meta-analysis, which was based on previous published studies and did not have original data. Therefore, no ethical approval and patient consent are required.
2.2. Inclusion criteria
The included studies must meet all the following criteria:
-
1.
the exposure of interest was DII;
-
2.
the outcome of interest was CVD risk or mortality;
-
3.
the study design was cohort or nested case-control; and
-
4.
the relative risks (RRs) with their corresponding 95% confidence intervals (CIs) were reported (or enough data were provided to calculate these values).
We excluded reviews/meta-analyses, case reports, and studies performed in animals or cells. Studies of other dietary patterns and diseases were also excluded.
2.3. Data extraction
Data extraction was performed independently by 2 reviewers with a predefined extraction form. Discrepancies between these 2 reviewers were resolved by consulting a third reviewer. The following information were extracted from each included study: the first authors surname, country, publication year, study design, study name or source, sample size (number of total participants and cases), age of participants, methods of diet assessment, fully-adjusted risk estimates, and adjusted covariates in the design or data analysis.
2.4. Study quality assessment
The methodological quality of each study was evaluated by 2 independent reviewers using the Newcastle–Ottawa Scale (NOS).[16] Discrepancies between these 2 reviewers were resolved by consulting a third reviewer. NOS awards a maximum of 9 scores to each study. High quality was defined as scores ≥7.
2.5. Statistical analysis
The combined RRs and 95% CIs for highest vs lowest DII in relation to CVD risk or mortality were estimated using a DerSimonian and Laird random effects model.[17] The heterogeneity among studies was tested using Cochran's Q test and the I2 statistic.[18] The Q statistic was used to examine the existence of heterogeneity with a significance level set at P ≤ .10. The value of I2 was used to determine the proportion of variation (I2 < 25% low heterogeneity; I2 = 25%–50% moderate heterogeneity; I2 > 50% large heterogeneity). Meta-regression analysis was further carried out to explore the potential sources of heterogeneity. Stratified analyses were performed according to study region, study quality, and number of cases. Sensitivity analysis was performed by re-calculating the pooled risk estimates after the omission of each study in turn. Potential publication bias was assessed by a visual funnel, Beggs test[19] and Eggers test.[20] All statistical analyses were performed with STATA 11.0 (StataCorp, College Station, TX), using two-sided P values.
3. Results
3.1. Study search and characteristics
The detailed process of study search and selection is shown in Figure 1. A total of 15 cohort studies[11,12,13,14,21,22,23,24,25,26,27,28,29,30,31] met the inclusion criteria. Nine studies[22,23,24,25,26,27,28,29,31] reported CVD mortality and 5 studies[11,12,13,14,21] reported CVD risk as outcome of interest, respectively. One study[30] reported both CVD risk and mortality. These studies were performed in the following geographical regions: Americas (n = 3), Europe (n = 7), Australia (n = 4), and Asia (n = 1). All of the included studies were published from 2015 to 2019. Dietary information was mainly collected by food-frequency questionnaires (FFQ). All of the included studies utilized the same methodology to assess the dietary inflammatory potential.[3] The study quality scores assessed by the NOS ranged from 7 to 9. The other study characteristics are presented in Tables 1 and 2.
Figure 1.
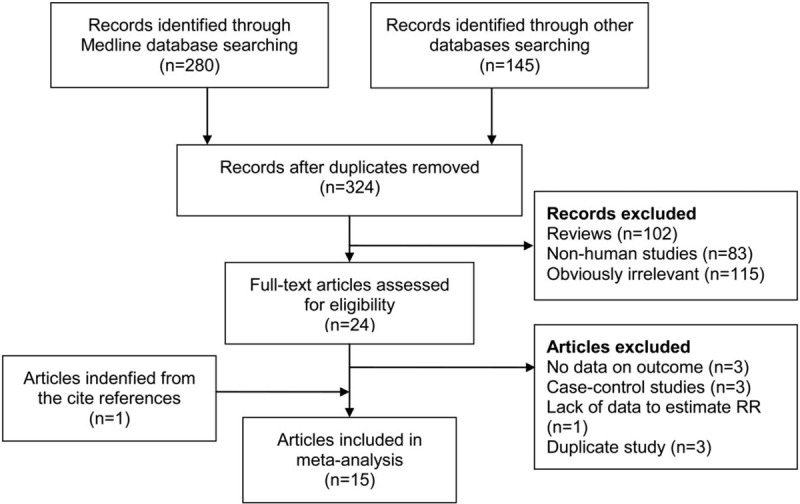
Flow of publication search and selection.
Table 1.
Main characteristics of the studies on the association between DII and cardiovascular risk.
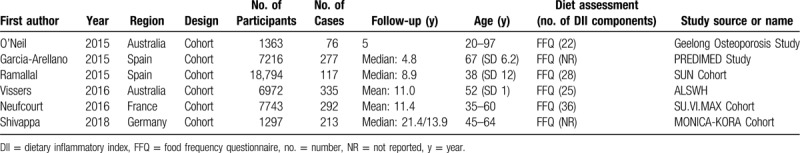
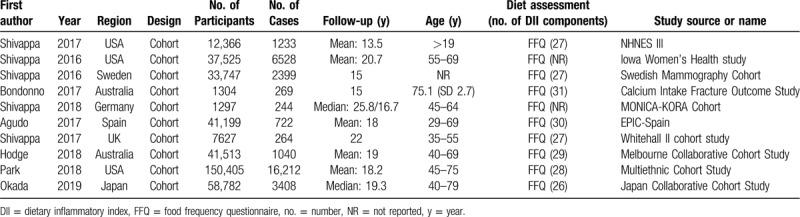
Table 2.
Main characteristics of the studies on association between DII and cardiovascular mortality.
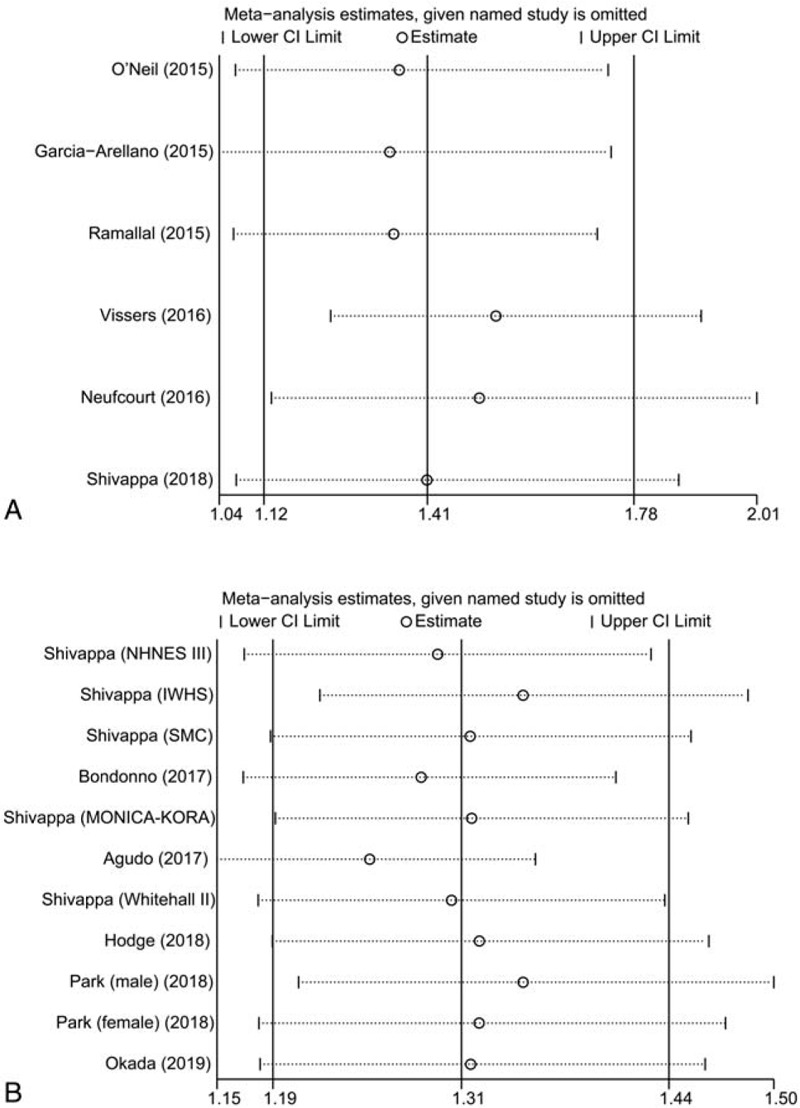
3.2. Overall analysis and subgroup analysis
The multivariable-adjusted RRs of the highest vs lowest DII scores, for each study and for the combination of all of the studies, are shown in Figures 2 and 3. The highest DII score was significantly associated with a higher risk of CVD (RR = 1.41, 95% CI 1.12–1.78) and CVD mortality (RR = 1.31, 95% CI 1.19–1.44), compared with the lowest DII score. In subgroup analyses, except for number of cases (P for interaction = .015), none of the other factors modified the association between DII and the risk of CVD incidence and mortality (Tables 3 and 4).
Figure 2.
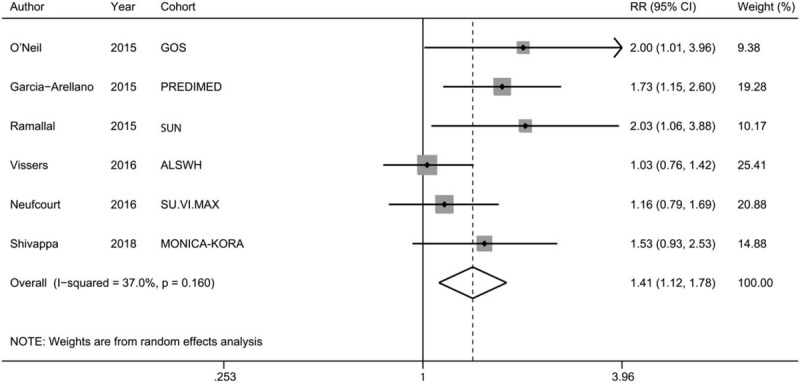
A forest plot presenting risk estimates from included studies estimating the association between DII and CVD risk.
Figure 3.
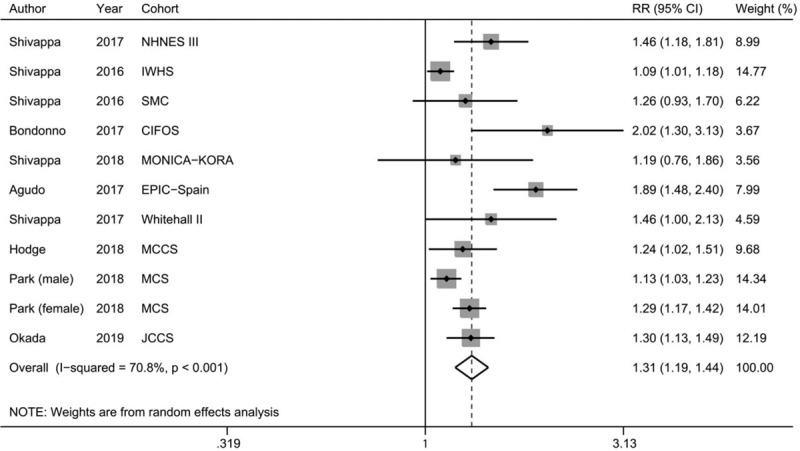
A forest plot presenting risk estimates from included studies estimating the association between DII and CVD mortality.
Table 3.
Subgroup analyses of the association between DII and cardiovascular risk.
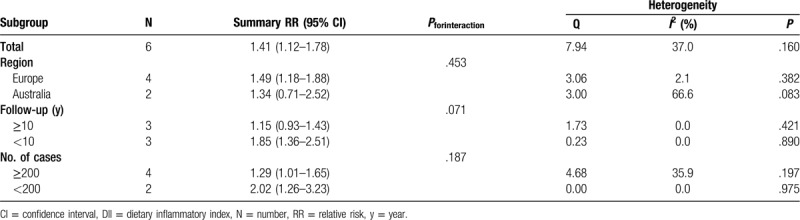
Table 4.
Subgroup analyses of the association between DII and cardiovascular mortality.
3.3. Evaluation of heterogeneity
In this meta-analysis, we used the Q statistic and the I2 index to evaluate the heterogeneity across studies. There was statistically significant heterogeneity among the studies on the association between DII and CVD mortality (P < .001; I2 = 70.8%). No obvious heterogeneity was observed among the studies on the association between DII and CVD risk (P = .160; I2 = 37.0%).
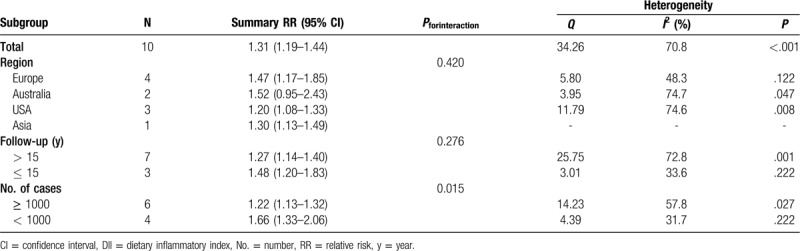
3.4. Sensitivity analysis and Publication bias
In the sensitivity analysis, the impact of each study on the pooled RR was examined by repeating the meta-analysis after removing 1 study at a time. Exclusion of any single study did not materially alter the pooled RRs (Fig. 4). There was some evidence of publication bias with Eggers test (P = .021) but not with Beggs test (P = .276). A certain degree of asymmetry was observed with a funnel plot (Fig. 5).
Figure 4.
Sensitivity analysis was performed by excluding each study in turn and then repeating the meta-analysis to determine the influence of a single study. (A) CVD risk; (B) CVD mortality.
Figure 5.
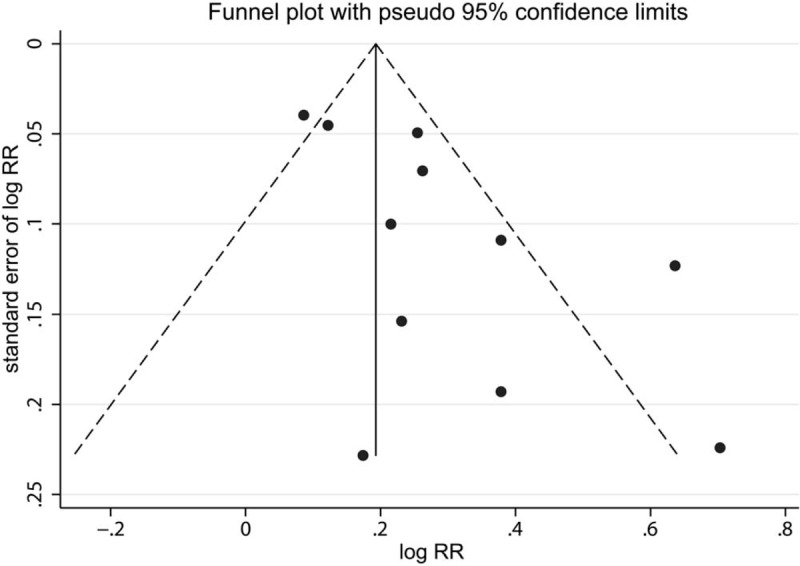
A funnel plot for the risk of CVD mortality.
4. Discussion
The present meta-analysis, which utilized existing evidence from 15 cohort studies, showed strong positive associations between DII score and CVD risk and mortality. Individuals with the highest DII scores had 41.0% and 31.0% elevated risk of CVD incidence and mortality when compared with those with the lowest DII scores.
Previous studies have been performed to examine various dietary patterns and indices in relation to CVD risk and mortality. A systematic review and meta-analysis by Rosato et al[32] reported that that Mediterranean diet exerted a protective effect on the risk of CVD based on 29 observational studies. Onvani et al[33] found that high adherence to the Healthy Eating Index (HEI) and Alternative Healthy Eating Index (AHEI) was significantly associated with a reduced risk of cardiovascular mortality. The DII is a novel dietary index that is grounded in peer reviewed articles focusing specifically on dietary inflammation. Many studies have reported a significant association between DII and various health outcomes[34,35] since the DII was firstly proposed by Shivappa et al in 2014.[3]
The mechanism underlining the association between a pro-inflammatory diet (high DII score) and a high risk of CVD is still not clear. One possible explanation is that a pro-inflammatory diet is able to increase the levels of cytokines like TNF-α, IL-1, and IFN-γ,[36,37] which may cause attraction and migration of inflammatory cells into vascular tissue. Camargo-Ramos et al[38] reported that an increased inflammatory potential of diet was negatively associated with an improved cardiometabolic risk parameters. Correa-Rodriguez et al[39] found that DII was significantly associated with cardiovascular risk factors in Spanish children and adolescents. Finally, Garcia-Calzon et al[40] observed a potential association between the inflammatory potential of the diet and telomere shortening in subjects with a high cardiovascular disease risk. All of these studies indicated that the dietary inflammatory potential would contribute to the CVD risk and mortality.
Our study had some strength. First, compared with previous studies on the same topic, this updated meta-analysis has the largest sample size and thus may enhance the statistical power. Second, our study only included cohort studies, which avoided the recall and selective bias. Third, sensitivity analysis indicated that the pooled risk estimates were stable and not dominated by any single study, which suggested that findings of our study were steady. Finally, the method used to calculate the DII score in each study was generally consistent,[3] which made these studies highly comparable.
This meta-analysis also had some limitations that should be acknowledged. First, the DII was mainly derived from self-administrated FFQ in most included studies and the food parameters used for calculation of DII were not completely consistent across studies, which may cause the exposure misclassification and heterogeneity. Second, only 6 cohorts were eligible for the analysis of CVD risk, which was relatively small. Third, substantial heterogeneity was detected with Q and I2 score, which may be attributed to the different demographic characteristics across studies. The meta-regression analysis indicted that the number of cases was the potential source of heterogeneity. Finally, although we have performed a comprehensive literature search, a certain degree of publication bias was observed with a visual funnel and Eggers test.
5. Conclusion
In summary, the present systematic review and meta-analysis indicates that a higher DII score is related to a higher risk of CVD. However, due to the large heterogeneity and other limitations as discussed above, further well-designed prospective cohort or trials are warranted to validate our findings.
Author contributions
Conceptualization: Mingxia Ji, Xiaofei Hong, Mengyan Chen, Tiejiang Chen, Jiao Wang, Ning Zhang.
Data curation: Mingxia Ji, Xiaofei Hong, Mengyan Chen.
Formal analysis: Mingxia Ji, Xiaofei Hong, Tiejiang Chen, Jiao Wang.
Funding acquisition: Ning Zhang.
Investigation: Mingxia Ji, Xiaofei Hong, Jiao Wang, Ning Zhang.
Methodology: Mingxia Ji, Ning Zhang.
Project administration: Mingxia Ji, Ning Zhang.
Resources: Mingxia Ji, Xiaofei Hong, Mengyan Chen, Tiejiang Chen, Jiao Wang, Ning Zhang.
Software: Mingxia Ji.
Supervision: Ning Zhang.
Validation: Mingxia Ji, Xiaofei Hong, Mengyan Chen.
Visualization: Tiejiang Chen, Jiao Wang, Ning Zhang.
Writing – original draft: Mingxia Ji, Xiaofei Hong.
Writing – review & editing: Mengyan Chen, Ning Zhang.
Footnotes
Abbreviations: CI = confidence interval, CVD = cardiovascular disease, DII = dietary inflammatory index, RR = relative risk.
How to cite this article: Ji M, Hong X, Chen M, Chen T, Wang J, Zhang N. Dietary inflammatory index and cardiovascular risk and mortality: a meta-analysis of cohort studies. Medicine. 2020;99:20(e20303).
MJ and XH contributed equally to this work.
This study was not supported by any grant.
The authors declare that there are no conflicts of interest.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Kwok CS, Gulati M, Michos ED, et al. Dietary components and risk of cardiovascular disease and all-cause mortality: a review of evidence from meta-analyses. Eur J Prev Cardiol 2019;26:1415–29. [DOI] [PubMed] [Google Scholar]
- [2].Ocke MC. Evaluation of methodologies for assessing the overall diet: dietary quality scores and dietary pattern analysis. Proc Nutr Soc 2013;72:191–9. [DOI] [PubMed] [Google Scholar]
- [3].Shivappa N, Steck SE, Hurley TG, et al. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr 2014;17:1689–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Tabung FK, Steck SE, Zhang J, et al. Construct validation of the dietary inflammatory index among postmenopausal women. Ann Epidemiol 2015;25:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Shivappa N, Hebert JR, Rietzschel ER, et al. Associations between dietary inflammatory index and inflammatory markers in the Asklepios Study. Br J Nutr 2015;113:665–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wirth MD, Shivappa N, Davis L, et al. Construct validation of the dietary inflammatory index among African Americans. J Nutr Health Aging 2017;21:487–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wang L, Liu C, Zhou C, et al. Meta-analysis of the association between the dietary inflammatory index (DII) and breast cancer risk. Eur J Clin Nutr 2019;73:509–17. [DOI] [PubMed] [Google Scholar]
- [8].Shivappa N, Godos J, Hebert JR, et al. Dietary inflammatory index and colorectal cancer risk-a meta-analysis. Nutrients 2017;9:E1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Laouali N, Mancini FR, Hajji-Louati M, et al. Dietary inflammatory index and type 2 diabetes risk in a prospective cohort of 70,991 women followed for 20 years: the mediating role of BMI. Diabetologia 2019;62:2222–32. [DOI] [PubMed] [Google Scholar]
- [10].Ruiz-Canela M, Bes-Rastrollo M, Martinez-Gonzalez MA. The role of dietary inflammatory index in cardiovascular disease, metabolic syndrome and mortality. Int J Mol Sci 2016;17:E1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Garcia-Arellano A, Ramallal R, Ruiz-Canela M, et al. Dietary inflammatory index and incidence of cardiovascular disease in the predimed study. Nutrients 2015;7:4124–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ramallal R, Toledo E, Martinez-Gonzalez MA, et al. Dietary inflammatory index and incidence of cardiovascular disease in the sun cohort. PLoS One 2015;10:e0135221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Neufcourt L, Assmann KE, Fezeu LK, et al. Prospective association between the dietary inflammatory index and cardiovascular diseases in the supplementation en vitamines et mineraux antioxydants (su.vi.max) cohort. J Am Heart Assoc 2016;5:e002735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Vissers LE, Waller MA, van der Schouw YT, et al. The relationship between the dietary inflammatory index and risk of total cardiovascular disease, ischemic heart disease and cerebrovascular disease: Findings from an Australian population-based prospective cohort study of women. Atherosclerosis 2016;253:164–70. [DOI] [PubMed] [Google Scholar]
- [15].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [17].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [18].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [19].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [20].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].O’Neil A, Shivappa N, Jacka FN, et al. Pro-inflammatory dietary intake as a risk factor for CVD in men: a 5-year longitudinal study. Br J Nutr 2015;114:2074–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Shivappa N, Blair CK, Prizment AE, et al. Association between inflammatory potential of diet and mortality in the Iowa Women's Health study. Eur J Nutr 2016;55:1491–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Shivappa N, Harris H, Wolk A, et al. Association between inflammatory potential of diet and mortality among women in the Swedish Mammography Cohort. Eur J Nutr 2016;55:1891–900. [DOI] [PubMed] [Google Scholar]
- [24].Agudo A, Masegu R, Bonet C, et al. Inflammatory potential of the diet and mortality in the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain). Mol Nutr Food Res 2017;61:1600649. [DOI] [PubMed] [Google Scholar]
- [25].Bondonno NP, Lewis JR, Blekkenhorst LC, et al. Dietary inflammatory index in relation to sub-clinical atherosclerosis and atherosclerotic vascular disease mortality in older women. Br J Nutr 2017;117:1577–86. [DOI] [PubMed] [Google Scholar]
- [26].Shivappa N, Hebert JR, Kivimaki M, et al. Alternative Healthy Eating Index 2010, Dietary Inflammatory Index and risk of mortality: results from the Whitehall II cohort study and meta-analysis of previous Dietary Inflammatory Index and mortality studies. Br J Nutr 2017;118:210–21. [DOI] [PubMed] [Google Scholar]
- [27].Shivappa N, Steck SE, Hussey JR, et al. Inflammatory potential of diet and all-cause, cardiovascular, and cancer mortality in national health and nutrition examination survey iii study. Eur J Nutr 2017;56:683–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hodge AM, Bassett JK, Dugue PA, et al. Dietary inflammatory index or Mediterranean diet score as risk factors for total and cardiovascular mortality. Nutr Metab Cardiovasc Dis 2018;28:461–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Park SY, Kang M, Wilkens LR, et al. The Dietary inflammatory index and all-cause, cardiovascular disease, and cancer mortality in the multiethnic cohort study. Nutrients 2018;10:E1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Shivappa N, Schneider A, Hebert JR, et al. Association between dietary inflammatory index, and cause-specific mortality in the MONICA/KORA Augsburg Cohort Study. Eur J Public Health 2018;28:167–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Okada E, Shirakawa T, Shivappa N, et al. Dietary Inflammatory Index is associated with risk of all-cause and cardiovascular disease mortality but not with cancer mortality in middle-aged and older Japanese adults. J Nutr 2019;149:1451–9. [DOI] [PubMed] [Google Scholar]
- [32].Rosato V, Temple NJ, La Vecchia C, et al. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr 2019;58:173–91. [DOI] [PubMed] [Google Scholar]
- [33].Onvani S, Haghighatdoost F, Surkan PJ, et al. Adherence to the Healthy Eating Index and Alternative Healthy Eating Index dietary patterns and mortality from all causes, cardiovascular disease and cancer: a meta-analysis of observational studies. J Hum Nutr Diet 2017;30:216–26. [DOI] [PubMed] [Google Scholar]
- [34].Phillips CM, Chen LW, Heude B, et al. Dietary Inflammatory Index and non-communicable disease risk: a narrative review. Nutrients 2019;11:E1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hebert JR, Shivappa N, Wirth MD, et al. Perspective: The Dietary Inflammatory Index (DII)-lessons learned, improvements made, and future directions. Adv Nutr 2019;10:185–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Wirth MD, Burch J, Shivappa N, et al. Association of a dietary inflammatory index with inflammatory indices and metabolic syndrome among police officers. J Occup Environ Med 2014;56:986–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Shivappa N, Wirth MD, Hurley TG, et al. Association between the dietary inflammatory index (DII) and telomere length and C-reactive protein from the National Health and Nutrition Examination Survey-1999-2002. Mol Nutr Food Res 2017;61:1600630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Camargo-Ramos CM, Correa-Bautista JE, Correa-Rodriguez M, et al. Dietary Inflammatory Index and cardiometabolic risk parameters in overweight and sedentary subjects. Int J Environ Res Public Health 2017;14:E1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Correa-Rodriguez M, Gonzalez-Jimenez E, Rueda-Medina B, et al. Dietary inflammatory index and cardiovascular risk factors in Spanish children and adolescents. Res Nurs Health 2018;41:448–58. [DOI] [PubMed] [Google Scholar]
- [40].Garcia-Calzon S, Zalba G, Ruiz-Canela M, et al. Dietary inflammatory index and telomere length in subjects with a high cardiovascular disease risk from the PREDIMED-NAVARRA study: cross-sectional and longitudinal analyses over 5 y. Am J Clin Nutr 2015;102:897–904. [DOI] [PMC free article] [PubMed] [Google Scholar]


