To the Editor:
The city of Hangzhou is a metropolis with a population of greater than 12 million. Since the onset of the coronavirus disease 2019 (COVID-19) pandemic in China at the end of December 2019, the municipal government adopted a strict policy to control the epidemic, including locking the whole city down on January 24, 2020. This lockdown time was even earlier than that for Wuhan. We tried to determine whether there was a considerable effect on the out-of-hospital system with patients with out-of-hospital cardiac arrest during the COVID-19 outbreak in one city in China.
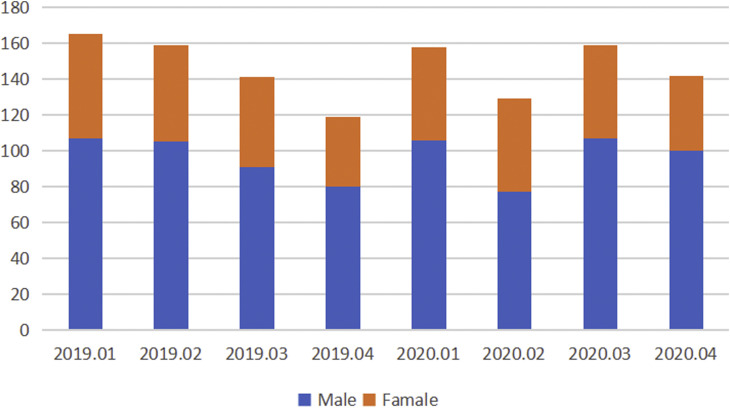
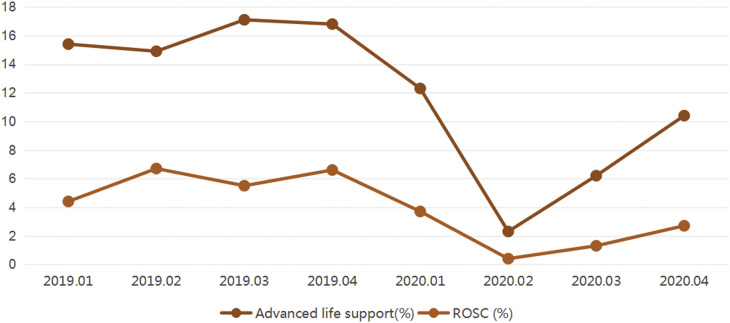
In Hangzhou, the management of emergency patients is based on an out-of-hospital system; more than 7,000 patients need out-of-hospital medical care, including approximately 140 to 160 patients with out-of-hospital cardiac arrest every month. The return of spontaneous circulation (ROSC) rate of patients with out-of-hospital cardiac arrest was approximately 4.5% before the COVID-19 outbreak in Hangzhou. Although only 181 cases have been confirmed in the city to date, COVID-19 has greatly influenced the out-of-hospital system and significantly affected out-of-hospital management of patients with cardiac arrest. We analyzed data from the Hangzhou out-of-hospital medical care system database. As shown in Figure 1 , the number of patients with out-of-hospital cardiac arrest has not significantly decreased since the pandemic began. However, the ROSC rate decreased to only 0.4% and advanced life support for patients with out-of-hospital cardiac arrest and with out-of-hospital emergency physicians was only 2.3% in February 2020 (Figure 2 ); the ROSC rate was still low even when the city reopened.
Figure 1.
Cases variation of out-of-hospital cardiac arrest during the epidemic
Figure 2.
Comparison of the management of cardiac arrest during the COVID-period (January to April 2020) and the reference period (2019).
There are 3 possible reasons for the significant decrease. First, COVID-19 patients were not spread across the city of Hangzhou, but the out-of-hospital medical system had the task of transferring patients with confirmed and suspected cases to a designated hospital, which overloaded systems operations. Second, the World Health Organization has categorized cardiopulmonary resuscitation as an aerosol-generating procedure, requiring the wearing of respirator masks and other personal protective equipment.1 Health care workers in the out-of-hospital system were provided with FFP2/FFP3 protective face masks before evaluation of or contact with any subject. Additionally, surgical gowns and eye protection were used if the patient’s symptoms were suggestive of respiratory disease. Delaying the delivery of chest compressions and defibrillation for up to several minutes so that health care workers can don personal protective equipment reduces the likelihood of patient survival.2 , 3 Our physicians chose to transfer the patients to the hospital as soon as possible, with only chest compressions and drug therapy for them, and with no ventilation to avoid aerosol generation. Third, patients with out-of-hospital cardiac arrest tend to be older than other patients; many of them stayed in their home alone and would not have been found if they had had a cardiac arrest. Some of the relatives of such patients decided not to have them resuscitated after the out-of-hospital medical staff arrived during the COVID-19 outbreak.
Footnotes
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
References
- 1.World Health Organization Global research on coronavirus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on425novel-coronavirus-2019-ncov Available at:
- 2.Tran K., Cimon K., Severn M. Canadian Agency for Drugs & Technologies in Health; Ottawa, Canada: 2011. Aerosol-Generating Procedures and Risk of Transmission of Acute Respiratory Infections: A Systematic Review.https://www.cadth.ca/sites/default/files/pdf/M0023__Aerosol_Generating_Procedures_e.pdf Available at: at. [PubMed] [Google Scholar]
- 3.Alhazzani W., Moller M.H., Arabi Y.M. Surviving Sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020;46:854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]