Abstract
Introduction
The Pandemic caused by the SARS-CoV-2 has put a strain on the most of health systems all over the world. Many hospitals had to re-organize to deal with the emergency, so that the non-core activities have been suspended or cancelled, raising management problems. The aim of this multicentre study is to report the epidemiological orthopaedic and traumatological data between COVID and pre-COVID era and to analyse patients’ needs and their management.
Methods
We reported and compared traumatological and elective orthopaedic surgeries performed in three of the main hospital centres in Tuscany during COVID (March 2020) and pre-COVID (March 2019) era. We also reported the epidemiological data about the number of orthopaedic first aid visits at the main hub, analysing the main differences. For each centre, we reported the number, diagnosis, co-morbidities, treatment, hospital course, complications and outcomes of confirmed COVID 19 patients. We also indicated what kind of PPE were used by medical staff and patients at any visit.
Results
The scheduled surgery drastically decreased in all the centres and the most of procedures were carried out for tumours, infections and implant mobilizations during the COVID time, delaying all the other ones. Trauma activities slightly decreased between the two time points: proximal femur fractures continued to engage our hospitals at the same pre-COVID volumes, while minor traumas drastically decreased. We report a decrease of 70.95% in orthopaedic first aid, with first-aid-visits/hospitalization ratio of 13.8 in the pre-COVID time vs 5.8 in the COVID time. A total of 5 confirmed COVID patients were treated for fractures and 4 of them healed without complications. We report just one case of death among COVID patients. All the medical staff members have worn the PPE and no one have developed COVID symptoms.
Conclusions
The COVID-19 raised many important issues, such as the optimal management of patients requiring the treatment of conventional diseases during a pandemic. The flow of patients changes from one area to another during a pandemic and an integrated approach within the same geographical area could be useful to better allocate resources and manage the patients’ needs. The preventive measures put in place in our country seem to work, but this first experience with COVID-19 crisis highlighted the chronic problems of our health system and we believe that we have to “learn the lesson” to be better prepared in the future.
Keywords: COVID 19, SARS-CoV-2, Epidemiology, Orthopaedic, Surgery, Trauma
1. Text
1.1. Background
The rapid widespread of the COVID-19 disease caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS- CoV-2) drastically changed the standards of daily living among all over the word. The first changes on people’s habits due to this novel coronavirus epidemic were observed in China, starting from the report of the first case at the end of December 2019 in the city of Wuhan.1,2 The Chinese people had a great reaction trying to contain the virus in a first red zone, progressively blocking the social and work activities in whole the country and activating extraordinary health measures such as the construction of new “COVID” hospitals. Despite these measures, it was not possible to contain the spread of the virus and the WHO declared the coronavirus pandemic on March 11, 2020.3 Unfortunately, Italy was the first country reporting an established case of COVID-19 disease in Europe. The epidemic has rapidly spread all over the country and the northern areas were the most involved. The high number of infected patients, the severity of the disease, the high number of deaths and the lack of beds in the Intensive Care Units (ICUs) pushed the government to progressively stop all the unnecessary activity to slow down the epidemic advance. On March 10, 2020, Italy declared the lockdown in all the country, basing on the Chinese model. Any kind of travel has been forbidden except for work activity (if allowed) or for a necessity state (e.g. urgent medical visits, essential goods supply, drugs supply, invalid people assistance etc.).4 These strictly measures have allowed to the other regions of the country to better react to the COVID-19 disease: in Tuscany the local Health System has re-organized most of the hospitals to avoid the problems of the first involved areas of the country. The most important changes in our health system have been the delaying of elective surgeries and non-urgent ambulatory visits, the internal re-organization of hospital wards to better distribute the health workers and to create separate COVID areas and the implementations of ICUs.
In this scenario, orthopaedic and traumatological activities have changed in our departments and a new resource targeted allocation has been necessary to better face the emergency and to give the best cares to the patients, as well reported in other studies.4, 5, 6, 7, 8
The aim of the present work is to analyse the main differences in the management of traumatological and orthopaedic activities in March 2020 - in the midst of the lockdown-vs March 2019 - before the COVID-19 epidemic-in three of the main trauma and orthopaedic centres in Tuscany.
2. Materials and methods
This epidemiological multicentre study has been approved by our local ethical committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments and with the International Conference on Harmonization (ICH) guidelines for Good Clinical Practice (GCP) issued in June 1996.
We reported all the traumatological and the elective orthopaedic surgeries performed in three of the major centres of north-west Tuscany during March 2020 and March 2019. We also reported the epidemiological data about the number of orthopaedic first aid visits at the main centre of the area (centre no.1).
All the recorded data were obtained using the same software for the retrieval: Dedalus First Aid for the first aid data and Dedalus Ormaweb for surgical data search. Concerning trauma and elective surgeries we report, for each centre, the number of patients treated, the age and sex of the patients and the main diagnosis/procedures. For Major Surgeries we refer to invasive procedures performed on large bone segments with high risk of bleeding (limb amputations, wide soft-tissue excision, primary and revision arthroplasties, and fractures interesting the humerus, the pelvis, the thighbone, the shinbone, the knee, etc). For Minor Surgeries we refer to all the other procedures performed on small segment with a limited risk of bleeding (arthroscopic procedures, soft-tissue procedures without large vessels involvement, hardware removals, small segment fractures, hand or foot surgeries etc). Concerning orthopaedic-first aid visits data, we report the number of total visits, age and sex of patients, the kind (i.e domestic, sport, traffic, work, enclosed spaces, school and beach injuries) and the type (i.e. fractures, polytraumas, articular dislocations, sprains/contusions, others) of trauma. We also report the total number of fractures and for the most frequent fracture the kind of treatment (conservative vs surgical one).
The number of COVID patients evaluated and treated was reported for each centre. Moreover, for each COVID patient we report diagnosis, co-morbidities, treatment, hospital course, complications and outcomes.
We compared the reported data between the two different times (COVID – March 2020 - vs pre-COVID- March 2019) focusing on the main changes and trying to draw a guideline to better manage the patients’ needs.
3. Results
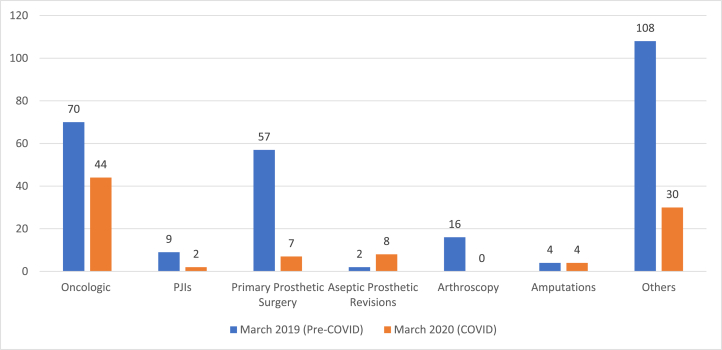
A total of 95 scheduled and 65 traumatological surgeries were performed in March 2020 at centre no. 1 versus 266 elective and 94 urgent procedures performed in March 2019 at the same institution. The number of major surgeries drastically decreased from 141 to 24 for scheduled and from 67 to 33 for trauma surgeries among the two time points (Table 1). Data related to main diagnosis and kind of surgery are reported in detail in Fig. 1 and Table 2.
Table 1.
Scheduled and Traumatological Procedures at centre 1,2 and 3 in March 2019 and March 2020. (n: number of patients; M: male; F: female).
| Scheduled Procedures |
Trauma Procedures |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Centre No. 1 |
Centre No.2 |
Centre No.3 |
Centre No. 1 |
Centre No.2 |
Centre No.3 |
|||||||
| March 2019 | March 2020 | March 2019 | March 2020 | March 2019 | March 2020 | March 2019 | March 2020 | March 2019 | March 2020 | March 2019 | March 2020 | |
| Total (n) | 266 | 95 | 110 | 21 | 68 | 23 | 94 | 65 | 95 | 82 | 81 | 71 |
| Gender (n) | 138 M, 128F | 48 M, 47F | 62F, 48 M | 7 M, 14F | 32 M, 36F | 8 M, 15F | 48 M, 46F | 32 M, 33F | 43 F, 52 M | 40 M, 42 F | 36 M, 45F | 31 M, 40F |
| Age y.o. (average) | 58.3 | 57.8 | 64.1 | 65.4 | 53.3 | 58.6 | 69.9 | 69.9 | 64.5 | 65.4 | 61.23 | 69 |
| Major Surgery (n) | 141 | 24 | 43 | 7 | 24 | 5 | 67 | 33 | 58 | 47 | 45 | 47 |
| Minor Surgery (n) | 125 | 71 | 51 | 14 | 44 | 18 | 27 | 32 | 37 | 35 | 36 | 24 |
Fig. 1.
Number and Kind of Scheduled Procedures at Centre no. 1 in March 2019 and March 2020. PJI: Periprosthetic Joint Infection.
Table 2.
Number of Trauma Surgeries at centre 1,2 and 3 in March 2019 (Pre-COVID) and 2020 (COVID).
| Fracture site | Patients treated n, (%) |
|||||
|---|---|---|---|---|---|---|
| Centre No. 1 |
Centre No. 2 |
Centre No. 3 |
||||
| March 2019 |
March 2020 |
March 2019 |
March 2020 |
March 2019 |
March 2020 |
|
| Femoral neck/head | 17, (18) | 20, (30.8) | 7, (7.4) | 8, (9.8) | 14, (17.3) | 10, (14.1) |
| Pertrochanteric | 20, (21.3) | 19, (29.2) | 19, (20) | 12, (14.6) | 9, (11.1) | 24, (33.9) |
| Malleolar | 6, (6.4) | 13, (20.0) | 8, (8.3) | 7, (8.5) | 4, (4.9) | 0, (0) |
| Distal forearm | 8, (8.6) | 2, (3) | 4, (4.2) | 3 (3.7) | 3, (3.7) | 2, (2.8) |
| Proximal humerus | 7, (7.5) | 2, (3) | 9 (9.5) | 5, (6.1) | 7, (8.7) | 6, (8.4) |
| Tibial shaft | 4, (4.2) | 3, (4.6) | 8, (8.4) | 1, (1.2) | 2, (2.5) | 3, (4.2) |
| Femoral shaft | 4, (4.2) | 4, (6.2) | 3, (3.2) | 3, (3.6) | 5, (6.2) | 3, (4.2) |
| Other sites | 28, (29.8) | 2, (3) | 37, (39) | 43, (52.5) | 37, (45.6) | 23, (32.4) |
At the centre no. 2 the surgical procedures performed in March 2020 and March 2019 were 21 vs 110 for scheduled surgery and 82 vs 95 for trauma surgery, respectively (Table 1). Also, for this series the number of major procedures decrease both for scheduled and trauma surgeries among the two time points: 43 vs 7 and 58 vs 47 in March 2019 and March 2020, respectively. Data related to main diagnosis and kind of trauma surgery are reported in detail in Table 2.
Data related to centre no. 3 are reported in Table 1, Table 2 Scheduled surgeries decreased from 68 in March 2019 to 23 in March 2020, while trauma surgeries were 81 and 71, respectively. Also, for the centre no.3, such as for the other ones, the number of proximal femur fracture treated hasn’t significantly changed over the time.
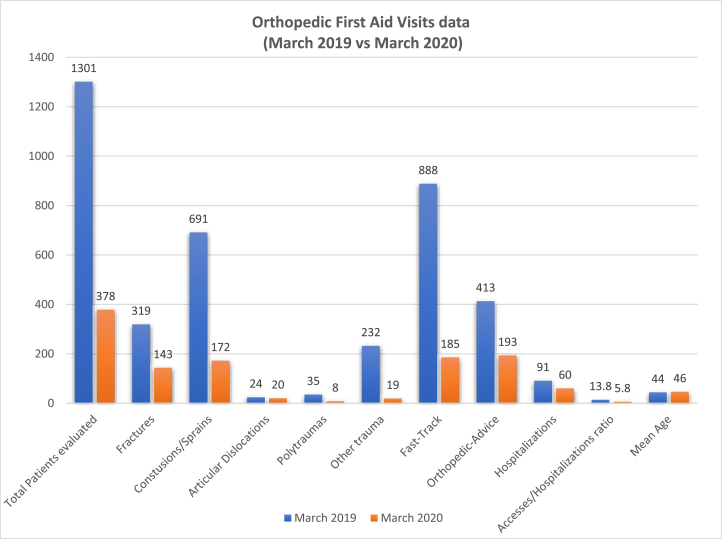
Concerning centre no. 1 orthopaedic first aid visits, we report a total of 1301 patients (644 F, 657 M) evaluated in March 2019: 888 patients were evaluated trough a “fast-track” path, without the evaluation of a general physician, and 413 were evaluated in “orthopaedic advice”. The patients treated for fractures were 319 (24.5%) and the patients requiring a hospitalization for surgical treatment were 94 (7%). The most of non-surgery patients have been treated for contusion or sprain (691–53.1%). Instead, we report a total of 378 patients (164 F, 214 M) evaluated in March 2020: 185 in “fast-track” and 193 in orthopaedic advice. The patients affected by fractures at any site were 143 (37,8%) and 65 (17.2%) patients required surgical treatment. Patients with contusion or sprain were 172 (45,5%). The decrease between COVID and pre-COVID era in the orthopaedic first aid visits is 70,95%. The ratio between the orthopaedic first aid visits and the hospitalization is 13.8 for March 2019 and 5.8 for March 2020. Fig. 2.
Fig. 2.
The diagram shows the difference between orthopaedic-first aid visits data in March 2019 (pre-COVID) and March 2020 (COVID) at Centre no.1.
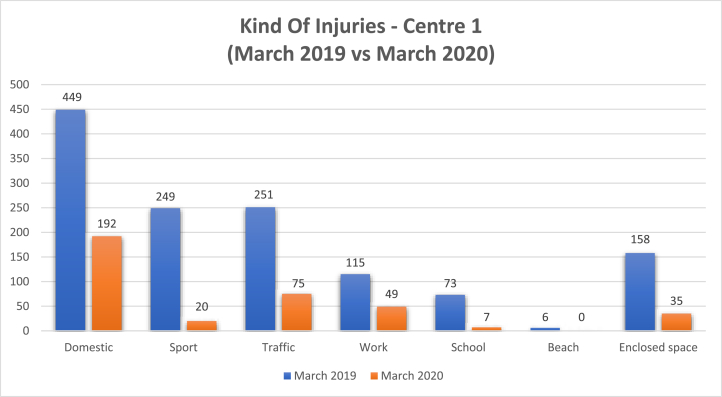
The kind of trauma evaluated at orthopaedic-first aid of centre 1 among the two time points are reported in detail in Fig. 3. In March 2019, the patients were evaluated mainly for domestic (34.5%), traffic (19.3%) and sport trauma (19.1), followed by work injuries (8.9%), injuries occurred in enclosed spaces (12.1%), school trauma (5.6%) and beach ones (0.5%). Also, in March 2020 the most of patients were evaluated for domestic accidents (50.8), even if the percentage was higher than March 2019. The traffic accidents rate continued to be high also during COVID era (21.6%), while all the other kind of trauma drastically decreased as reported in Fig. 3.
Fig. 3.
The diagram shows the difference in the kind of trauma evaluated at centre 1 orthopaedic-first-aid between March 2019 (pre COVID) and March 2020 (COVID).
The kind of treatment for each type of fracture evaluated at centre 1 between the two time points is reported in detail in Table 3. The main conservative treatments at orthopaedic-first aid consisted of plaster casts or braces positioning, depending on the type of fracture and patients’ compliance. The surgical treatment was performed in all cases according to AO Trauma guidelines.9
Table 3.
Kind of treatment (conservative vs surgical) for each type of fracture diagnosed at centre 1 orthopaedic-first aid during March 2019 (pre-COVID) and March 2020 (COVID).
| Fracture site |
Number of fractures evaluated at Center 1 orthopaedic-first aid |
|||||
|---|---|---|---|---|---|---|
| March 2019 |
March 2020 |
|||||
| Conservative | Surgical | Total | Conservative | Surgical | Total | |
| Distal forearm | 54 | 8 | 62 | 18 | 2 | 20 |
| Hand phalange | 39 | 4 | 43 | 10 | 0 | 10 |
| Foot phalange | 23 | 2 | 25 | 3 | 0 | 3 |
| Ankle | 15 | 6 | 21 | 4 | 13 | 17 |
| Proximal humerus | 14 | 7 | 21 | 8 | 2 | 10 |
| Pertrochanteric | 1 | 17 | 18 | 0 | 20 | 20 |
| Metatarsal | 11 | 3 | 14 | 5 | 0 | 5 |
| Femoral Neck/Head | 0 | 20 | 20 | 0 | 19 | 19 |
| Metacarpal | 10 | 3 | 13 | 5 | 1 | 6 |
| Pelvic | 10 | 2 | 12 | 5 | 0 | 5 |
| Tibial shaft | 4 | 8 | 12 | 2 | 3 | 5 |
| Femoral shaft | 3 | 8 | 11 | 1 | 4 | 5 |
| Foot | 10 | 1 | 11 | 4 | 0 | 4 |
| Clavicle | 8 | 0 | 8 | 5 | 0 | 5 |
| Calcaneus | 6 | 0 | 6 | 1 | 0 | 1 |
| Tibial plateau | 1 | 5 | 6 | 0 | 1 | 1 |
| Other sites | 16 | 0 | 16 | 7 | 0 | 7 |
Concerning SARS-CoV-2 patients we report variable data. At centre no. 1, during March 2020, we evaluated in the orthopaedic-first aid just 2 COVID patients. The first one was a 34 years old man with a displaced fracture of the basis of second finger proximal phalanx treated with a Herbert’s screw. At the first time visit the patient didn’t show COVID-19 disease symptoms, so he was evaluated by the orthopaedic surgeon and before the hospitalization he had been buffered. The swab was positive for SARS-CoV-2 and the patient was admitted in a dedicate medical COVID ward and operated in a dedicated COVID surgical room. The patient suffered from Buerger’s and Raynaud’s diseases and presented an history of alcohol and drugs addiction. His post-operative course was uneventful, he didn’t developed symptoms and, after two consecutive negative swabs (3 days apart each other), he was discharged home. He returned to the 1-month follow-up visit and he was well. The second case was a female 84 years old patient suffering from arterial hypertension, atrial fibrillation and chronic renal failure. She fell down on the floor at home causing a great-trochanter un-displaced fracture. In this case we didn’t choose an operative treatment and the patient was discharged home with the indication to stay at rest in the bed or chair for 1 month. The day after the visit the swabs results became available and she was found positive to the virus. The patient has been quarantined at home and she has been followed by the dedicated COVID-19 home service. She never developed symptoms and she returned to 1-month follow-up.
In the centre no. 2 just one COVID patient was evaluated and treated by the orthopaedic team: a 69 years old man with a Colles’ fracture treated with a plaster cast in a COVID-dedicated first-aid room. In this case the patient presented mild respiratory symptoms with mild fever before he had the fracture. So, a specific procedure was activated and the healthcare staff was adequately equipped with the Personal Protective Equipment - PPE (ffp2 mask, double pair of gloves, insulating gown and the protective visor). The patient presented some comorbidities: artery hypertension, type two diabetes mellitus and COPD. He was discharged home and he continued to be monitored by the dedicated COVID home team. Also, in this case the patients returned to 45-days follow-up with negative swabs and without any symptoms.
In the centre no.3 there were two patients affected by COVID 19. The first one, a 79 years old man presented a femoral neck fracture successfully treated with a Total Hip Arthroplasty (THA) in a dedicated surgical room. The patient didn’t have COVID 19 symptoms during the first aid visit and he was buffered before had been admitted at the hospital. The swab was positive for the virus and he was admitted in a medical COVID ward. The patient didn’t developed complications during his hospitalization course, and he was discharged home once the swabs resulted negative. He suffered from artery hypertension and atrial fibrillation as comorbidities. Also, in this case the healthcare staff used specific PPE, once the COVID 19 was diagnosed. The patient returned to the successive follow-up visit and didn’t show respiratory symptoms. The other case in centre no. 3 was a female 75 years old patient treated with an external fixator for a tibial fracture. She was urgently treated and the swab result wasn’t still available at time of surgery. So she was treated as a positive patient in the dedicated operative room and then transferred in a COVID ward, once the swab result was available. Unfortunately, the patient died for cardio-respiratory arrest 43 days after surgery. The patient already suffered from artery hypertension, second type diabetes mellitus, COPD and had a story of heart stroke treated with a coronary stent. During her hospitalization she was treated with supportive therapy in the medical ward and then transferred to an ICU to better manage her respiratory problems. She was buffered several times, but the swab never became negative.
We didn’t report additional confirmed cases of COVID 19 during March 2020. Concerning the PPE, in all the three centres taken into account, the same rules were observed. At the first visit, in absence of a confirmed positivity to the SARS-CoV-2, both the patients and the orthopaedic surgeon dressed a common surgical mask while during surgery (with undetermined or positive swab) the healthcare staff dressed a ffp2 mask, the surgical cap, the surgical gown and a protective visor. Nobody of the medical staff developed any symptoms after these visits or treatments and no-one was therefore buffered or quarantined, according to national COVID rules for medical staff.
4. Discussion
The pandemic COVID-19 disease has caused a devastating impact on the standards of daily living limiting social, work and sport activities all over the world. These changes have been made necessary to avoid a wider spread of SARS-CoV-2 and its related morbidity.4,8 The current health care providers have never faced before such a dramatic epidemic wave and the most of health care systems all over the word aren’t sufficiently equipped to manage this serious disease. In Italy, as well as in China before, the COVID-19 containment has been possible thanks to an imposing effort by the health care givers, the government and all the citizens. The central government has laid down the guidelines that local regional health systems has to follow, even if there are some management differences from one region to another and also from a hospital to another in the same region. These differences are mainly due to the local trend of the epidemic and the available hospital resources.4,5 Regarding our study, in all the three Hospital took into account, dedicated COVID paths have been created to separate non-COVID patients to the COVID ones. At centre no.1 the orthopaedic wards have been moved, and the number of beds has been reduced to re-allocate nursing staff. The elective procedures have been delayed or suspended except for priority diseases, where a delay in surgery could have aggravated the patients’ clinical condition. Trauma activities have been carried out routinely except for the safety measures necessary do detect and treat COVID patients; the ones that have to be hospitalized are buffered, transferred to a protected area and then, once the result of the swab is available, they are hospitalized to a COVID or non-COVID ward. Moreover a “COVID” surgical room has been set up to treat the surgical emergencies with an undetermined or positive swab. Similarly, in the other two centres elective surgery has been delayed or suspended, if possible, and trauma activities have been carried out as at centre no.1. However, the epidemic spread in centre no. 2 area has been higher and a part of orthopaedic ward has been closed and became a COVID area, so that some trauma patients, the healthier ones, have been moved to other facilities. In centre no. 3 area, the epidemic spread has been lower than the other ones areas, so that the orthopaedic activities have been reduced, but the ward hasn’t been moved or closed.
From the reported data we can see how the orthopaedic and traumatological activities have changed over the time. The scheduled surgery drastically decreased in all the three centres in March 2020 than March 2019, while the traumatological activities slightly decreased among the same time points. In particular for centres no. 2 and 3, the scheduled activities have been almost entirely cancelled or postponed. This data may be due to the types of surgery performed at centre no.1 than the other ones: the most of scheduled surgeries in March 2020 were performed for tumours, infections or implant aseptic mobilizations. The spread of scheduled surgeries for centres no. 2 and 3 between COVID and pre-COVID era could be wider because of many of these surgeries are routinely carried out in other external facilities, affiliated with National Health System. Moreover, although within the same limited geographical area (north-western Tuscany), the three centres had to face with a different volume of COVID 19: in particular the centre no.1 area has been hit hard and all the activities have been reduced to the bare minimum to make room for adequately equipped COVID areas inside the orthopaedic ward itself. The analysis of the other epidemiological data doesn’t show great differences about age and gender of the patients treated among the two time points, but there are differences in the kind of fractures treated. The proximal femur fractures, typically affecting the elderly and following domestic trauma, doesn’t change over the time, while in the COVID time the other kind of fractures drastically decreased, probably for a decrease in road, sport and work traumas due to the lockdown of the country.
The analysis of data related to orthopaedic first aid visits revealed a drastically decrease in March 2020 than March 2019 (70,95%), in particular related to minor traumas. Moreover, the number of total visits has been so lower than the pre-COVID time that the lockdown can’t be addressed as the only cause. The ratio between the orthopaedic first aid visits and the trauma surgeries performed in March 2020 is drastically lower than March 2019 (6.3 vs 14.3) and these data suggest an improper standard use of the orthopaedic first aid, probably due to an inadequate efficiency of the public health system. A further problem raised during COVID 19 epidemic is the management of patients requiring a delayed surgery, as well as the patient treated with a temporary external fixator and discharged at home waiting to have the appropriate local conditions for a definitive osteosynthesis. These patients shouldn’t keep in hospital, but the lack of beds available for elective surgery makes difficult to re-admit these patients for final treatment. It would be advisable to have in mind these considerations for the future and to create special paths for these patients, leaving a certain number of beds available for intermediate care.
Concerning the total number of confirmed COVID patients evaluated and treated we have to make some clarification. We report just 5 confirmed case because of the modalities of buffering expected in the first phase of the epidemic in our country. Usually at general first aid just patients with fever or respiratory symptoms were buffered. These patients were treated as COVID (and isolated in dedicated first-aid areas) ones until the result of the swab was available and the healthcare staff used all the provided PPE (ffp2 mask, double pair of gloves, insulating gown and the protective visor). Then if the positivity has been confirmed, they were transferred to dedicated COVID wards to be treated. If a patient didn’t show respiratory symptoms of fever, he wasn’t buffered even if he needed to be hospitalized. So at the first visit the medical staff didn’t wear specific PPE for COVID, but just a surgical mask as well as for the visit of patient that didn’t need to be hospitalized, but just conservative treated. Also, the patients in these cases wore the surgical musk.
These kinds of measures were necessary in the first phase of the epidemic wave because of the lack of large number of PPE and swabs reagents. However, we don’t report confirmed COVID infection over the healthcare staff and no one developed COVID-19 symptoms. So, we can state the preventive measures and social distancing rules had been effective to manage the epidemic in our hospitals.
Concerning the difference from one area to another in the epidemic spread we believe that an integrated approach and a shared protocol could be beneficial to better manage the emergency and to avoid the overload of the health system, according to other authors.5, 6, 7, 8
5. Conclusion
The COVID-19 raised many important issues, such as the optimal management of patients requiring the treatment of conventional diseases during a highly contagious infectious pandemic disease. As underlined by our epidemiologic study, the flow of patients changes from one area to another during a pandemic and an integrated approach within the same geographical area could be useful to better allocate resources and manage the patients’ needs. Moreover, the this first experience with COVID-19 crisis highlighted the chronic problems of our health system in term of human, and economic resources. On the other hand, the preventive measures and social distancing rules seem to work in limiting disease diffusion, but we believe that we have to “learn the lesson” to be better prepared in the future.
Authors contributions
Design and Methods: MG, MS, Data retrieval: MG, GB, MV, Writing original draft: MG, EB, Reviewing: MS, MM.
Declaration of competing interest
All authors declare that they have no conflict of interest. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Michele Giuntoli, Email: michelegiuntoli87@gmail.com.
Enrico Bonicoli, Email: enrico.bonicoli@gmail.com.
Giulia Bugelli, Email: bugeposta@hotmail.it.
Massimo Valesini, Email: massimovalesini@gmail.com.
Mario Manca, Email: mario.manca@uslnordovest.toscana.it.
Michelangelo Scaglione, Email: michelangelo.scaglione@gmail.com.
References
- 1.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020 Mar;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang L.S., Wang Y.R., Ye D.W., Liu Q.Q. A review of the 2019 Novel Coronavirus (COVID-19) based on current evidence”. Int J Antimicrob Agents. 2020 Mar;19:105948. doi: 10.1016/j.ijantimicag.2020.105948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Who.int.
- 4.Placella G., Salvato D., Delmastro E., Bettinelli G., Salini V. CoViD-19 and ortho and trauma surgery: the Italian experience. Injury. 2020 Apr 15;(20):S0020–S1383. doi: 10.1016/j.injury.2020.04.012. 30343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Randelli P.S., Compagnoni R. Management of orthopaedic and traumatology patients during the Coronavirus disease (COVID-19) pandemic in northern Italy. Knee Surg Sports Traumatol Arthrosc. 2020 Apr 25 doi: 10.1007/s00167-020-06023-3. 2020 Apr 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in lombardy, Italy. Jama. 2020;323(16):1545. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 7.Bettinelli G., Delmastro E., Salvato D., Salini V., Placella G. Orthopaedic patient workflow in CoViD-19 pandemic in Italy. J Orthop. 2020;22:158–159. doi: 10.1016/j.jor.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jain V.K., Vaishya R. COVID-19 and orthopaedic surgeons: the Indian scenario. Trop Doct. 2020;50(2):108–110. doi: 10.1177/0049475520921616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buckley R.E., Moran C.G., Apivatthakakul T. Place of publication not identified; THIEME: 2018. AO Principles of Fracture Management. [Google Scholar]