Abstract
Many patients with COVID-19, the clinical illness caused by SARS-CoV-2 infection, exhibit mild symptoms and do not require hospitalization. Instead, these patients are often referred for 14-days of home isolation as symptoms resolve. Lung ultrasound is well-established as an important means of evaluating lung pathology in patients in the emergency department and in intensive care units. Ultrasound is also being used to assess admitted patients with COVID-19. However, data on the progression of sonographic findings in patients with COVID-19 on home isolation is lacking. Here we present a case series of a group of physician patients with COVID-19 who monitored themselves daily while in home isolation using lung point-of-care ultrasound (POCUS). Lung POCUS findings corresponded with symptom onset and resolution in all 3 patients with confirmed COVID-19 during the 14-day isolation period. Lung POCUS may offer a feasible means of monitoring patients with COVID-19 who are on home isolation. Further studies correlating sonographic findings to disease progression and prognosis will be valuable.
Keywords: Lung ultrasound, POCUS, COVID-19, Home isolation, Monitoring
1. Introduction
The spectrum of clinical illness caused by SARS-CoV-2 infection, called COVID-19, ranges from mild cold-like symptoms to acute respiratory distress syndrome (ARDS) requiring intensive care unit (ICU) hospitalization [1]. Home isolation is suggested for patients with COVID-19 with stable clinical presentations to avoid hospitalization and minimize spread of the disease. Typically, in an emergency department (ED) or inpatient setting monitoring the progression of patients' lung findings is achieved with daily chest x-rays (CXR) or intermittent computed tomography (CT) scans [[2], [3], [4]]. While helpful in inpatient settings, CXR and CT have distinct disadvantages for patients on home isolation, most notably the need to present to a hospital or healthcare setting and risk further exposure of both the patient, healthcare workers, and potentially future patients from scanner contamination. Currently there is limited information characterizing the progression of imaging findings throughout the disease course for patients in home isolation.
Point-of-care lung ultrasound (POCUS) is an important tool in evaluating patients with acute dyspnea in the ED. This tool has also shown promising results in assessing patients with COVID-19 [[5], [6], [7]]. Typical sonographic findings in patients with viral pneumonia range from minimal change in the normal aerated lung pattern to severe bilateral interstitial disease [8,9]. The most prominent findings of COVID-19 appear to be in the posterior and inferior lung zones, and, importantly, near the terminal alveoli which are subpleural and thus most amenable to POCUS [10]. In mild to moderate disease, focal or scattered B-lines replace A-lines which represent a normal lung aeration pattern. More severe disease demonstrates increased frequency of B-lines which can coalesce into a confluent pattern, as well as development of sub-pleural consolidations, irregular pleural lines, and air bronchograms [8,9].
While lung POCUS is fairly well-documented in initial evaluation of ED patients suspected of COVID-19, and in assessing critically ill patients in the ICU [11,12], little is known about the use of lung POCUS in patients with COVID-19 on home isolation. Additionally, there is a paucity of data documenting the progression of sonographic findings over an entire COVID-19 disease course. Here we present a case series of physician-patients with confirmed COVID-19 who used sequential lung POCUS for tracking pulmonary disease while in home isolation. They provided full consent to use their images and stories. We demonstrate the sonographic progression of COVID-19 in three patients with clinically stable presentations.
2. Case series
2.1. Case 1
This was a 31-year-old female with no significant past medical history who was eleven weeks pregnant at the time of symptom onset. She initially presented to the ED with a dry cough and dyspnea, subjective tachypnea, and fever to 40 °C. The previous day she experienced three episodes of diarrhea and one episode of non-bloody emesis. Prior to presenting to the ED she performed lung POCUS using Butterfly iQ portable ultrasound device (Butterfly Network -Rothberg's Inc. U.S.A.) at home. At that time, B-lines were evident in both pulmonary apices (Fig. 1A) as well as a patchy unstructured pleura in the right apex and right base.
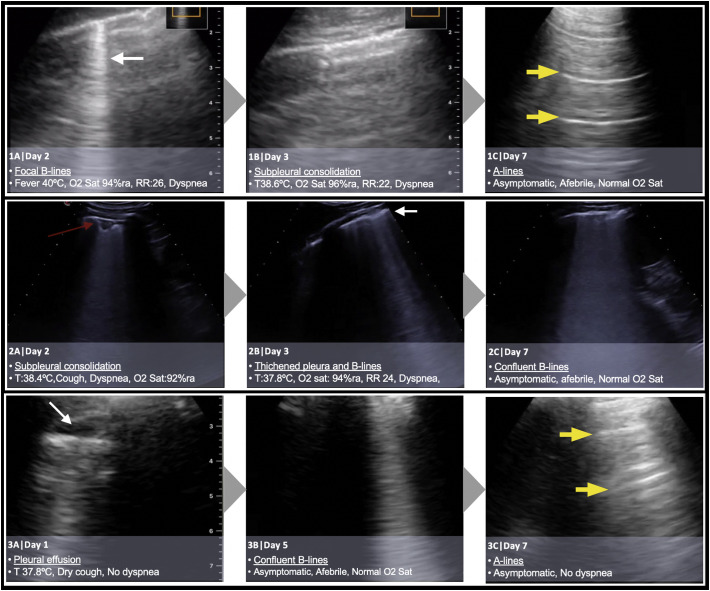
Fig. 1.
Evolving lung pathology findings during days of home isolation in patients with COVID-19.
Initial vital signs in the ED included a blood pressure of 137/40 mmHg, heart rate of 110 beats per minute (bpm), with 100% oxygen saturation on room air. On physical exam, lung auscultation was normal. A CXR was not obtained due to the patients' reassuring examination, POCUS findings and the patient being pregnant. Given her clinical stability, the patient was sent home to self-isolate for 14 days.
On day 2 of illness, reverse transcription polymerase chain reaction (RT-PCR) performed in the ED the day prior resulted as positive for SARS-CoV-2 infection. Her oxygen saturation was 96% on room air at that time, but she felt clinically improved. She continued to experience low-grade fever, dry cough and rhinorrhea, with improved dyspnea. However, repeat lung POCUS revealed ongoing B-lines in the apex, as well as greater pleural irregularity and destructuring in lung bases with small subpleural infiltrates and more B lines.
On the third day she was nearly asymptomatic with room air oxygen saturations of 98%. Lung POCUS revealed focal B-lines and subpleural consolidation in zone L3 and A-lines in the anterior zone of L1 (Fig. 1B). Lung POCUS findings did not change until the fifth day when an improvement of the pleural irregularity was observed, though B-lines at the right base persisted (video 1). The pulmonary apices began demonstrating an A-line pattern on day 7 (Fig. 1C and video 1). After 10 days, lung POCUS continued to demonstrate an A-line pattern and the patient remained asymptomatic through the end of her home isolation period.
2.2. Case 2
This was a 58-year-old physician with no significant past medical history. He began developing symptoms 48 h after contact with a patient with severe COVID-19 who ultimately required admission to the ICU. Initial presenting symptoms included low-grade fever, general malaise, headache, myalgias, and a dry cough. He did not experience dyspnea. 12 h after symptom onset, RT-PCR testing for SARS-CoV-2 was performed and resulted positive. Given his reassuring clinical presentation CXR was not obtained and he was sent home for isolation.
On day 2, symptoms had progressed to include dyspnea on exertion and cough, as well as low-grade fevers and room air oxygen saturations as low as 92%. Lung POCUS using MyLab™Gamma portable ultrasound device (Esaote Inc. Genoa Italy) demonstrated subpleural consolidations, a thickened pleural line (Fig. 2A) and focal B-lines (Fig. 2B) on days 2 and 3 (video 2). By day 6 of illness his symptoms began to improve, however by day 7 lung POCUS findings progressed to include confluent B-lines (Fig. 2C). The pathological findings were bilateral and were primarily detected in the posterior inferior lobes. Upon detecting these POCUS findings, he began taking a 1 week course of hydroxychloroquine. After two weeks of home isolation he had been asymptomatic for several days, POCUS findings had resolved, and he returned to work.
2.3. Case 3
This was a 45-year-old female physician with no significant past medical history, who had a recent close contact with a SARS-CoV-2-positive patient the week prior. She initially developed fever to 37.8 °C and a dry cough. Her physical exam at the time of presentation to the ED was unremarkable. SARS-CoV-2 RT-PCR was performed and resulted positive. Given her reassuring clinical picture, the patient was referred to home isolation. She performed daily lung POCUS using a Butterfly iQ, (Butterfly Network - Rothberg's Inc. U.S.A.) to document and monitor her clinical progression.
During the following days, she experienced progressive malaise, nausea and diarrhea, as well as a persistent dry cough. She developed fever to 38.2 °C with an oxygen saturation of 98% on room air. She was started on a one-week course of hydroxychloroquine. On day 1 of isolation, lung POCUS showed a small pleural effusion and a thickened pleural line at the left lower lobe (Fig. 3A). The following day a subpleural consolidation was noticed on the left lateral thoracic wall (video 3). By day 3, the subpleural consolidations started to resolve, however by day 5 a confluent B-line pattern appeared (Fig. 3B and video 3). There was no significant changes to lung POCUS pattern with scattered B-lines in anterior zones and a confluent B-line in the right posterolatearl alveolar and/or pleural syndrome-point (at the intersection of a horizontal line at the level of the lower chest and a vertical line at the posterior axillary line). By day 7 her physical exam was normal, she was asymptomatic, and lung POCUS demonstrated an A-line pattern (Fig. 3C and video 3). The remainder of her 14-day home isolation was completed uneventfully.
3. Discussion
3.1. Lung POCUS progression in COVID-19
Lung POCUS is a widely recognized means of assessing patients with respiratory distress in the ED and ICU [7,11,13]. Early studies have suggested lung POCUS may play a similarly important role in evaluating patients with COVID-19. Data from cases in Spain, Italy, and China describes characteristic lung ultrasound findings in COVID-19 patients, most commonly posterior and inferior B-lines with sub-pleural consolidations [8,9].
While existing literature describes use of lung POCUS in COVID-19 cases in the ED and inpatient settings [14], reports on POCUS use for patients in home isolation are limited. Additionally, though POCUS is often used as a tool for initial assessment of dyspneic patients, there remains little information demonstrating the progression of sonographic findings over the entire COVID-19 illness. Here, we present a case series documenting progression of lung POCUS findings over the clinical course for three stable patients on home isolation. As has been previously identified, our series reaffirms that B-lines are present in early illness, and we also demonstrate that resolution of sonographic findings likely lags behind symptomatic improvement.
POCUS, particularly when performed with portable handheld devices, offers an inexpensive, accessible, user-friendly, and easy-to-disinfect method for assessing cardiopulmonary pathology. Unfortunately, correlation between sonographic imaging findings and COVID-19 disease course or prognosis has yet to be established. However, should future studies identify prognostic or diagnostic value in the changes seen on lung ultrasound in COVID-19 cases, several important potential uses for daily lung POCUS in patients on home isolation may emerge. Under these conditions, serial lung POCUS may play a role in home monitoring for early identification of clinical deterioration, or patient reassurance of clinical improvement. Thus, the prospect of repeat imaging assessments with POCUS over the course of COVID-19 illness may have important implications for future patients.
Another potential future role for serial lung POCUS exams would be to identify safe timing to discontinue isolation or return to work. Currently, the decision to discontinue home isolation is dictated by the either a time-based strategy, test-based strategy, or symptom-based strategy as outlined by the Centers for Disease Control [15,16]. Unfortutnely, lung POCUS findings have not been correlated with viral load or infectivity. As this gap in knowledge represents a major hurdle to using POCUS to dictate disposition, it remains an important focus for future studies.
3.2. Limitations
While our series is among the first to document serial progression of lung POCUS findings in patients with COVID-19, it does have some limitations. All patients in this work were clinically well, and their symptoms resolved over the course of several days to weeks. Collecting serial lung POCUS images on patients who were either clinically less well, or who required repeat medical examinations during their illness course would likely have been informative regarding the variability of POCUS progression and findings. Additionally, none of our patients had repeat RT-PCR tests performed once clinical symptoms or POCUS findings resolved. Establishing the timing of RT-PCR clearance to correlate with either symptomatic or sonographic progression might have been revealing. Finally, the lung POCUS findings seen in COVID-19 which are described here and in other studies are not specific to SARS-CoV-2 infection. Rather, these findings can be seen in cases of interstitial syndrome triggered by various causes. While our patients all had RT-PCR testing confirming SARS-CoV-2 infection, in situations where testing is not available lung POCUS can only suggest COVID-19 however other sources of interstitial syndrome must be diagnostically considered.
4. Conclusions
In this case series we present serial lung POCUS findings from patients with COVID-19 while on home isolation. This study identifies B-lines as one of the earliest sonographic findings in SARS-CoV-2 infection and demonstrates that improvement in lung POCUS changes lag behind resolution of clinical symptoms. Lung POCUS may have an important role in monitoring patients with COVID-19 in the future, however further work correlating POCUS findings with infectivity, viral clearance, disease progression, and prognosis are needed.
The following are the supplementary data related to this article.
Patient 1 - Dynamic changes in lung POCUS findings from a thickened pleural line, focal B-lines and mild subpleural consolidation on day 2 to complete resolution with multiple A-lines on day 7.
Patient 2 - Lung POCUS findings of subpleural consolidation on day 2 associated with focal B-lines that progressed to confluent B-lines on day 6.
Patient 3 - Progress of lung POCUS findings from a pleural effusion and thickened pleural line on day 1 to a focal B-line and mild subpleural consolidation on day 3 which persisted for a week and improved in second week of home isolation to a normal A-line pattern on day 14.
Presentations
None.
Financial support
None.
CRediT authorship contribution statement
Hamid Shokoohi: Conceptualization, Data curation, Investigation, Supervision, Writing - review & editing. Nicole M. Duggan: Writing - original draft, Writing - review & editing. Gonzalo García-de-Casasola Sánchez: Investigation, Writing - review & editing. Marta Torres-Arrese: Investigation, Writing - review & editing. Yale Tung-Chen: Investigation, Writing - review & editing, Supervision.
Declaration of competing interest
The authors report no conflict of interest.
References
- 1.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. Apr 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. Feb 26, 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295(3) doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buhumaid R.E., St-Cyr Bourque J., Shokoohi H., Ma I.W.Y., Longacre M., Liteplo A.S. Integrating point-of-care ultrasound in the ED evaluation of patients presenting with chest pain and shortness of breath. Am J Emerg Med. 2019;37(2):298–303. doi: 10.1016/j.ajem.2018.10.059. Feb. [DOI] [PubMed] [Google Scholar]
- 6.Cortellaro F., Colombo S., Coen D., Duca P.G. Lung ultrasound is an accurate diagnostic tool for the diagnosis of pneumonia in the emergency department. Emerg Med J. Jan 2012;29(1):19–23. doi: 10.1136/emj.2010.101584. [DOI] [PubMed] [Google Scholar]
- 7.Zanobetti M., Scorpiniti M., Gigli C., Nazerian P., Vanni S., Innocenti F. Point-of-care ultrasonography for evaluation of acute dyspnea in the ED. Chest. Jun 2017;151(6):1295–1301. doi: 10.1016/j.chest.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Huang Y., Wang S., Liu Y., Zhang Y., Zheng C., Zheng Y. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19) February 26, 2020. https://ssrn.com/abstract=3544750 Available at SSRN:
- 9.Peng Q.Y., Wang X.T., Zhang L.N. Findings of lung ultrasound of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. May 2020;46(5):849–850. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bai H.X., Hsieh B., Xiong Z., Halsey K., Choi J.W., Tran T.M.L. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. Mar 10, 2020 doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brogi E., Bignami E., Sidoti A., Shawar M., Gargani L., Vetrugno L. Could the use of bedside lung ultrasound reduce the number of chest x-rays in the intensive care unit? Cardiovasc Ultrasound. Sep 13, 2017;15(1):23. doi: 10.1186/s12947-017-0113-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soldati G., Smargiassi A., Inchingolo R., Buonsenso D., Perrone T., Briganti D.F. Is there a role for lung ultrasound during the COVID-19 pandemic? J Ultrasound Med. Mar 20, 2020 doi: 10.1002/jum.15284. [doi: 10.1002/jum.15284] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lichtenstein D.A. BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill. Chest. 2015;147(6):1659–1670. doi: 10.1378/chest.14-1313. Jun. [DOI] [PubMed] [Google Scholar]
- 14.Complete GUIDE to LUNG ultrasound in COVID-19 (coronavirus) patients. https://pocus101.com/complete-guide-to-lung-ultrasound-in-covid-19-coronavirus-patients/ Website:
- 15.CDC Criteria for return to work for healthcare personnel with suspected or confirmed COVID-19 (interim guidance) 3 May 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/return-to-work.html Website.
- 16.CDC Symptom-based strategy to discontinue isolation for patients with COVID-19. 3 May 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/strategy-discontinue-isolation.html Website:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient 1 - Dynamic changes in lung POCUS findings from a thickened pleural line, focal B-lines and mild subpleural consolidation on day 2 to complete resolution with multiple A-lines on day 7.
Patient 2 - Lung POCUS findings of subpleural consolidation on day 2 associated with focal B-lines that progressed to confluent B-lines on day 6.
Patient 3 - Progress of lung POCUS findings from a pleural effusion and thickened pleural line on day 1 to a focal B-line and mild subpleural consolidation on day 3 which persisted for a week and improved in second week of home isolation to a normal A-line pattern on day 14.