To the Editors:
Recent studies have reported cardiac abnormalities in patients with coronavirus disease 2019 (COVID-19).1 Echocardiography remains an essential diagnostic tool in this climate, particularly with emerging data that myocardial injury appears to be associated with adverse prognosis2 and that echocardiography may add important prognostic information.3 , 4 We present our institutional experience with echocardiography in the current pandemic with the goal of assessing the prevalence and reversibility of left ventricular (LV) dysfunction.
Requests for echocardiograms in patients with COVID-19 were screened for appropriateness by echocardiography laboratory physicians; all performed studies (n = 125 patients over 49 days, all hospitalized) were included in this report. Studies were performed on standard (EPIQ; Philips Healthcare, Andover, MA), laptop-sized (Vivid I; GE Healthcare, Milwaukee, WI), or tablet (Lumify; Philips Healthcare) machines. Echocardiographic measurements were made according to society guidelines.5 Echocardiographic data were extracted from the clinical report and clinical information from the medical record.
Average patient age was 64 ± 15 years, and 50 (40%) were women. The most common comorbidities included hypertension (60%), diabetes mellitus (41%), and obesity (50%; mean body mass index, 31 ± 7 kg/m2). The majority (n = 85 [69%]) of patients were in the intensive care unit at time of echocardiography, with 75 (88%) requiring mechanical ventilation and 60 (71%) vasopressor support.
LV ejection fraction was normal or hyperdynamic in 97 patients (78%) and impaired (<50%) in 28 (22%). Wall motion abnormalities, evaluable in 115 patients, were present in 16 (14%). Combined, a total of 33 patients (26%) had LV dysfunction, defined as either LV ejection fraction < 50% or segmental wall motion abnormalities; LV dysfunction was preexisting in six of 33. Follow-up echocardiograms were obtained after a median of 14 days in 11 of 33 patients with LV dysfunction (including one patient with prior LV dysfunction), revealing resolution of abnormalities (improvement in wall motion abnormalities and/or LV ejection fraction normalization) without procedural intervention in nine of 11 (82%) and persistent LV dysfunction in two of 11 (18%), including the aforementioned individual with preexisting LV dysfunction.
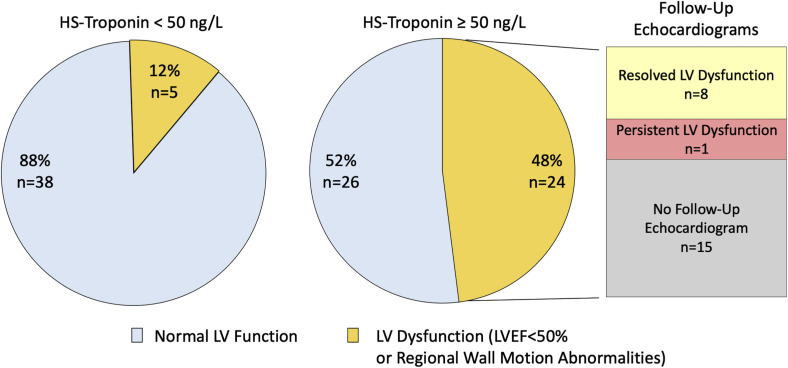
Among patients with cardiac biomarkers measured within 3 days before echocardiography (n = 93), median peak high-sensitivity troponin was 51 ng/L (interquartile range, 24–139 ng/L) and median peak N-terminal pro–brain natriuretic peptide 1,643 pg/mL (interquartile range, 374–8,278 pg/mL). In the subset (n = 50) with troponin ≥ 50 ng/L, 24 patients (48%) had evidence of LV dysfunction (Figure 1 ). Nine patients in this group (LV dysfunction and troponin ≥ 50 ng/L) underwent follow-up echocardiography, with resolution of LV abnormalities in eight (with the sole exception noted above with previously documented LV dysfunction). Median peak troponin was 613 ng/L (interquartile range, 251–1,585 ng/L) among those with LV recovery, compared with 280 ng/L in the patient without improvement.
Figure 1.
LV dysfunction in patients with COVID-19 stratified by high-sensitivity (HS) troponin level. The presence or absence of LV dysfunction, defined by LV ejection fraction (LVEF) < 50% or regional wall motion abnormalities, is shown in the group of patients with high-sensitivity troponin < 50 ng/L (left; n = 43) and ≥50 ng/L (right; n = 50). Of the 24 patients with some form of LV dysfunction in the elevated troponin group, nine underwent follow-up echocardiography, with the majority (n = 8) demonstrating resolution of LV abnormalities with the exception of one patient with previously documented LV dysfunction.
We describe here our initial experience with echocardiography during the COVID-19 pandemic and highlight two important findings. First, LV dysfunction was common, affecting 26% overall and 48% of those with troponin ≥ 50 ng/L. Second, although follow-up echocardiography was limited, resolution of LV dysfunction was noted in nine of 11 cases and in eight of nine with troponin ≥ 50 ng/L. We acknowledge that the screening process for echocardiography requests creates important selection bias, and we do not suggest that these findings apply across all patients with COVID-19. Prospective studies, and correlation of echocardiographic data with disease severity, biomarkers, and clinical outcomes, will be required to understand the range of cardiovascular involvement in COVID-19.
Footnotes
Conflicts of interest: None.
Alan S. Pearlman, MD, FASE, served as guest editor for this report.
References
- 1.Clerkin K.J., Fried J.A., Raikhelkar J., Sayer G., Griffin J.M., Masoumi A. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 2.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. https://jamanetwork.com/journals/jamacardiology/fullarticle/2763524 Available at: [DOI] [PMC free article] [PubMed]
- 3.Li Y., Li H., Zhu S., Xie Y., Wang B., He L. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. JACC Cardiovasc Imaging. https://imaging.onlinejacc.org/content/early/2020/04/20/j.jcmg.2020.04.014 Available at: [DOI] [PMC free article] [PubMed]
- 4.Argulian E., Sud K., Vogel B., Bohra C., Garg V.P., Talebi S. Right ventricular dilation in hospitalized patients with COVID-19 infection. JACC Cardiovasc Imaging. https://imaging.onlinejacc.org/content/early/2020/05/13/j.jcmg.2020.05.010?download=true Available at: [DOI] [PMC free article] [PubMed]
- 5.Lang R.M., Badano L.P., Mor-Avi V., Afilalo J., Armstrong A., Ernande L. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28 doi: 10.1016/j.echo.2014.10.003. 1-39.e14. [DOI] [PubMed] [Google Scholar]