Editor,
Patients with Corona Virus Disease (COVID-19) are likely to develop cold, pneumonia, or acute respiratory failure and some of them are requiring anesthesia care for emergency endotracheal intubation [1]. It would be an enormous challenge for perioperative care providers in providing optimal treatment for these patients and avoiding the cross-infection by SARS-CoV-2. We have recorded >100 critically ill patients with COVID-19 receiving emergency endotracheal intubation in Wuhan Union hospital, from Feb 1, 2020 to April 1, 2020, and the success rate of intubation was 100% with no medical staff infected by SARS-CoV-2. Here, we summarized Chinese experience about practical workflow for emergency endotracheal intubation in critically ill patients with COVID-19.
1. Emergent endotracheal intubation indications for confirmed/clinical diagnosis/suspected cases in fever clinics or isolation wards
-
1)
Under high-flow nasal catheter oxygen (HFNC) therapy, non-invasive mechanical ventilation (NIV), or 10–15 L/min via a face mask with reservoir bag, the patient's respiratory rate > 30 beats/min or hypoxemia (SpO2 < 90%), if oxygenation index (PaO2/FiO2) < 200 mmHg, endotracheal intubation can be considered; PaO2/FiO2 ≤ 150 mmHg, endotracheal intubation must be performed [2].
-
2)
Respiratory and cardiac arrest patients.
2. Patient ward preparations before endotracheal intubation
-
1)
Personnel preparation: the attending doctor or related medical staff familiar with the ventilator and the suction operation should give assistance;
-
2)
Item preparation:
-
i.
Sign on consent to the risk of endotracheal intubation;
-
ii.
Open venous access (indwelling needle above 20G) and three-way valve, connect with 0.9% physiological saline;
-
iii.
Monitor vital signs (ECG, respiratory rate, SpO2 and blood pressure);
-
iv.
Well connected threaded tube, oxygen, power supply, and invasive ventilator with properly adjusted ventilator parameters;
-
v.
Oxygen pack filled with oxygen;
-
vi.
Connect the suction device;
-
vii.
Prescribe in advance and prepare related drugs.
3. Precautions for anesthesia staff before endotracheal intubation
-
1)
After receiving the notification, the anesthesiologist re-confirms the indications for endotracheal intubation and checks the patient's basic situation;
-
2)
The anesthesiologist should check the ventilator, make sure the ventilator parameters are set properly and patient's venous access is open, and evaluate the airway condition.
4. Protection during endotracheal intubation (taking Level III protection measures)
-
1)
Personal protection should be done according to the hospital infection prevention and control requirements including hand-washing clothes or working clothes, medical protective masks, disposable work caps, disposable protective clothing, disposable latex gloves, disposable shoe covers, eye-protective medical surgical masks or goggles, medical protective masks, splash-proof screen or a full-face hood [3];
-
2)
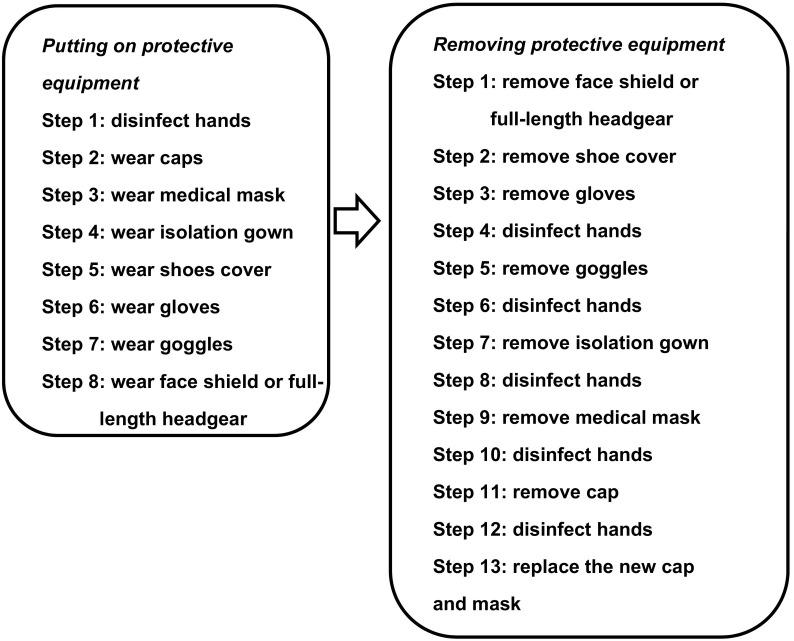
Putting on personal protective equipment or removing personal protective equipment, as shown in Flow chart 1 .
-
3)
Avoiding shaking while removing the protective equipment. After the protective clothing is taken off, it should be rolled up by the inside and put into the yellow garbage can. The protective equipment should be discarded into the double yellow garbage bags and put to the designated area.
Flow chart 1.
The steps of taking Level 3 medical protection measures.
5. Procedure of endotracheal intubation
-
1)
Before endotracheal intubation, it is necessary to check the monitoring equipment (ECG, respiratory rate, blood pressure and SpO2), intubation equipment (video laryngoscope, laryngeal mask, endotracheal tube, intubation stylet), auxiliary respiratory equipment (breathing balloon, mask), oxygen supply equipment, sputum suction equipment again, array the various instrument lines, and prepare first-aid drugs;
-
2)
Pre‑oxygenated with 100% FiO2 for 5 min through a mask via a face mask with reservoir bag, or breathing mask, or BIPAP ventilator, etc. Avoiding pressure-assisted ventilation before the patient's consciousness disappears [4].
-
3)
Anesthesia induction (requiring at least one assistant throughout the process):
-
i.
Patients in fever clinics, with unknown medical history, are treated as full stomach;
-
ii.For patients in the ICU, because most of them are performed with a BIPAP ventilator, airway assessment cannot be performed. It is recommended not to remove the patients' breathing mask for airway assessment, and treat them as the difficult airway patients. Taking propofol 1.0–1.5 mg/kg i.v., and then rocuronium 1–1.5 mg/kg i.v., fentanyl 2–4 μg/kg i.v.;
-
4)60–90 s after drug administration and the patient's spontaneous breathing completely disappears, quickly remove the respiratory oxygen mask or BIPAP ventilator mask at the end of expiration, insert a video laryngoscope and complete the endotracheal intubation. The whole process should be done by one anesthesiologist as much as possible. If necessary, the assistant can provide appropriate assistance (deliver the endotracheal tube, pull the tube stylet, hand bite block, etc) to ensure the successful completion of endotracheal intubation;
-
5)Judgment of endotracheal tube depth: It is not easy to judge the tube depth of patients with severe pulmonary lesions by auscultation of respiratory sounds. It is recommended to observe the bilateral chest relief, ventilator breathing waveform and respiratory parameters for comprehensive judgment. Besides, end-respiratory carbon dioxide or fiberoptic bronchoscopy can also determine the position of the tube, or indirect judgment by bedside ultrasound to check whether the endotracheal tube has entered the esophagus by mistake [5];
-
6)For patients with oral secretions, if there is no airway obstruction, airway sunction is recommended after completion of endotracheal intubation;
-
7)If repeated endotracheal intubation is not successful and the patient's SpO2 is extremely low, it is recommended to quickly place the laryngeal mask for mechanical ventilation [6]. After the oxygenation improves, anesthesiologist can decide whether to re-intubate again.
-
4)
6. Management after endotracheal intubation
-
1)
Complete relevant prescription and endotracheal intubation records;
-
2)
Routine sedation is recommended to prevent the tube from being bitten, collapsed or even prolapsed by the patient's struggle, and avoid unnecessary secondary intubation. If necessary, using muscle relaxants to eliminate spontaneous breathing. Protect cornea with 0.5% erythromycin ointment;
-
3)
Lung protective ventilation strategy: low tidal volume (6–8 mL/kg, ideal body weight) and low inspiration pressure (platform pressure < 30 cmH2O) for mechanical ventilation to reduce ventilator-related lung injury; breathing parameters can be adjusted by the result of arterial blood gas [7]. The whole workflow recommendations for emergency endotracheal intubation are shown in.
Although more data is needed to support our workflow, we do hope the frontline experience about emergency endotracheal intubation in critically ill patients with COVID-19 can help keep healthcare workers safe and provide optimal care to patients.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81701887; No. 81571075) and the National Key Research and Development Project (No. 2018YFC2001802).
Contributors
Not applicable.
CRediT authorship contribution statement
Haifa Xia:Writing - original draft, Validation.Shiqian Huang:Writing - original draft, Validation.Weimin Xiao:Writing - review & editing, Validation.Yun Lin:Writing - review & editing, Validation.Xiaomin Hu:Writing - review & editing, Validation.Bingqing Nie:Writing - review & editing, Validation.Ken Lin:Writing - review & editing, Validation.Dongshi Lu:Writing - review & editing, Validation.Xueyin Chen:Investigation, Validation.Limin Song:Investigation, Validation.Li Wang:Investigation, Validation.Yuhong Zhang:Investigation, Validation.Shanglong Yao:Writing - review & editing, Validation.Xiangdong Chen:Writing - original draft, Writing - review & editing, Validation.
Declaration of competing interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81701887; No. 81571075) and the National Key Research and Development Project (No. 2018YFC2001802).
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 Novel Coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fan E., Brodie D., Slutsky A.S. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319:698–710. doi: 10.1001/jama.2017.21907. [DOI] [PubMed] [Google Scholar]
- 3.Chen X., Liu Y., Gong Y., Guo X., Zuo M., Li J., et al. Perioperative management of patients infected with the novel coronavirus: recommendation from the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology. 2020;132:1307–1316. doi: 10.1097/ALN.0000000000003301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanouz J.L., Lhermitte D., Gérard J.L., Fischer M.O. Comparison of pre-oxygenation using spontaneous breathing through face mask and high-flow nasal oxygen: a randomised controlled crossover study in healthy volunteers. Eur J Anaesthesiol. 2019;36:335–341. doi: 10.1097/EJA.0000000000000954. [DOI] [PubMed] [Google Scholar]
- 5.Ahn J.H., Kwon E., Lee S.Y., Hahm T.S., Jeong J.S. Ultrasound-guided lung sliding sign to confirm optimal depth of tracheal tube insertion in young children. Br J Anaesth. 2019;123:309–315. doi: 10.1016/j.bja.2019.03.020. [DOI] [PubMed] [Google Scholar]
- 6.Higgs A., McGrath B.A., Goddard C., Rangasami J., Suntharalingam G., Gale R., et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323–352. doi: 10.1016/j.bja.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 7.Fan E., Del Sorbo L., Goligher E.C., Hodgson C.L., Munshi L., Walkey A.J., et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]