Abstract
The coronavirus pandemic has engulfed the nations of the world for the first five months of 2020 and altered the pace, fabric and nature of our lives. In this overview accompanying the Special Issue of Cytokine & Growth Factor Reviews, we examine some of the many social and scientific issues impacted by SARS-CoV2 – personal lives, economy, scientific communication, the environment. International members of Istituto Pasteur in Rome and INITIATE, the Marie Curie Training Network reflect on the lasting global impact of the coronavirus pandemic.
Keywords: SARS-CoV2, Covid-19, scientific response, global pandemic
1. Introduction
The World Health Organization (WHO) officially declared the SARS-CoV-2 outbreak a Public Health Emergency of International Concern on January 30, 2020 and a global pandemic on March 11, 2020. Countries were urged by WHO to adopt strict social distancing and quarantine measures to avoid virus spread and to protect public health [1]. Despite fragmented international efforts to contain the spread, SARS-CoV2 has spread to 213 countries, resulting in more than 5 million cases and deaths approaching 400,000 since its formal identification in Wuhan China in December 2019. This issue of Cytokine & Growth Factor Reviews is devoted to reviews from around the globe, describing the rapidly accumulating knowledge about the virus, the immunopathogenic consequences of severe disease, the consequences of the cytokine storm and potential therapeutic interventions that could improve morbidity and mortality until a vaccine can be developed and made available. Below, members of Istituto Pasteur in Rome and the Marie Curie ITN INITIATE (https://initiate-itn.eu) reflect on the lasting global impact of the coronavirus pandemic.
2. Warning signs
“Pestilence is in fact very common, but we find it hard to believe in a pestilence when it descends upon us. There have been as many plagues as wars in history; yet always plagues and wars take people equally by surprise.”
- Albert Camus, The Plague
‘How quickly it hit us’ – this is one of the most common sentiments about the Covid-19 pandemic. We were all caught off guard in one way or another; in an instant, an obscure outbreak of pneumonia in an exotic foreign locale - in the next, a viral outbreak jumping from China to the heart of Italy, then to all of Europe, on to America - finally a plague that stopped the world. As the pandemic hit all countries of the globe, it became indisputably clear that everyone was connected - united against a viral scourge [2].
Despite the shock, there were plenty of warning signs. Since the beginning of the 21st century, recurring outbreaks and epidemics presaged what was coming - there was the first SARS outbreak in 2003, H1N1 influenza pandemic in 2009, MERS coronavirus in 2011, Ebola in 2014−16; mosquito-borne Zika in 2016. A collage of news magazines ( Fig. 1 ) screamed out warnings of an impending pandemic but the clichéd phrase ‘it’s not a matter of if, but when’ continued to be ignored. Even the messages from political leaders (Presidents Barak Obama and George W. Bush) and scientific leaders (NIAID Director Anthony Fauci) went unheard. Below are links to their statements from 2005 to 2017.
Fig. 1.
Magazine covers from recent years announcing the arrival of new virus outbreaks around the globe.
https://abcnews.go.com/Politics/george-bush-2005-wait-pandemic-late-prepare/story?id=69979013
https://www.sciencealert.com/niaid-director-warned-us-government-of-a-surprise-outbreak-in-2017
International cooperation and a unified strategy of pandemic preparedness were not a priority. In the end, there was no united response - a global leadership void painfully revealed at a moment when it was most needed. What resulted was an international cacophony of last moment efforts, strategies and opinions to suppress the viral pandemic - after it was already upon the world.
3. Global scientific response
“I have no idea what's awaiting me, or what will happen when this all ends. For the moment I know this: there are sick people and they need curing.”
In order to tackle the Covid-19 crisis, an unparalleled international scientific response has been launched with the goal to understand viral genetics, immunopathogenesis, and therapeutic strategies. Public and private funders across the globe have launched an unprecedented number of initiatives to support multidisciplinary projects addressing the detection, treatment and prevention of SARS-CoV2 infections. Most of the calls encourage collaboration between international scientists, industry, healthcare community, and government policy makers, to facilitate a well-integrated COVID-19 response. The dramatic effects of COVID-19 outbreak taught us that similar pandemics cannot be managed solely at the national level. For this reason, alliances, consortia and networks have emerged on every continent, to connect experts in different research areas of fundamental science, clinical trials, social and behavioural sciences, engineering, and bioinformatics [3].
In the same context, it has been remarkable how research groups and companies from all over the world have been “repurposing” equipment, facilities and product lines in a joint effort for a rapid response against the ongoing pandemic. Companies that were once producing perfume switched gears to production of much-needed hand sanitizers and disinfectants; industrial companies switched to making face masks which were in short supply in many countries, and automotive companies started production of medical devices, such as ventilators. Scientists in non-virology research fields, who were required to halt their research indefinitely due to the lockdowns, turned their laboratories into diagnostic testing facilities for SARS-CoV-2 and organized into volunteer groups to help researchers on the front lines with their skills and expertise [[4], [5], [6], [7]].
This pandemic has also brought to light the importance of open science, data-sharing and new means of communication among members of the scientific community [[7], [8], [9], [10]]. Numerous data sets are available publicly, alongside literature reviews and preprint articles in bioarxiv and medarxiv portals. This openness has resulted in a massive amount of information spreading swiftly, which is an important driving force moving COVID-19 research forward in a short time. Of course, such openness comes with a cost: the surge of preprints available in bioarxiv and medarxiv has made it harder to keep up with the screening process of articles to be published in the preprint repositories. More than ever before, information needs to be scrutinized before going public to avoid the danger of inaccuracies, misinformation or even conspiracy theories. Such a situation is unprecedented, as no other pandemic in human history has been tackled in this way. Many scientists all over the world welcome this new form of communication and data-sharing and believe that eventually there will be a balance between good-quality information spreading quicker versus perfect-quality information that is unavailable until much later [8].
The EU joined forces to coordinate a common response against the coronavirus pandemic. On 30th January 2020, when the pandemic was not declared yet, European Commission mobilized a budget of €10 million for research, that was subsequently increased to €47.5 million [11]; later on, the Innovative Medicines Initiative (IMI), a partnership between the European Commission and the pharmaceutical industry, invested a total of 90 € million for research proposals to combat the COVID-19 emergency [12]. During the Coronavirus Global Response pledging event organized by the EU together with WHO (May 4th), €7.4 billion was raised from donors worldwide, to be used “for developing, producing and deploying a vaccine for all”, the European Commission President von der Leyen said [13]. In the UK, Government invested £20 million to fund new studies against coronavirus, including studies to sequence the different virus isolates as a tool to understand virus behaviour, mutation frequency, virus spread and emergence of new strains [14,15].
Part of these funds will be also used to allow the rapid, large scale production of a vaccine. With more than 100 research laboratories conducting vaccine development research, and with eight vaccine candidates already moving to clinal trials, the race to develop an effective prophylactic vaccine is on [16,22]. Since the biotech firm Moderna announced plans to launch vaccine trials in humans, the US government has invested $483 million to scale up that company’s vaccine production [17]. Meanwhile, the National Institutes of Health (NIH), together with other government organizations and biotech companies, set up a partnership to coordinate efforts against the COVID-19 pandemic, giving priority to the development of an efficient vaccine and therapeutic drugs [18]. Days ago, Moderna announced the results of a small eight-person phase I trial of their spike mRNA vaccine candidate, and the preliminary results indicate that all subjects developed antibodies, even at the lowest dose of inoculum [19], encouraging the company to proceed with a phase II clinical trial that will involve 600 participants. However, scientists are cautious over the successes of such vaccine candidates since the levels of the immune response needed to grant protection against SARS-CoV-2 are not yet well understood [8].
European biotech companies are also working to develop a potential COVID-19 vaccine. In Germany, BioNTech has designed four vaccine candidates that deliver mRNA encoding four different viral antigens [20]; ReiThera in Rome, Leukocare in Munich, and Univercells in Brussels have announced the creation of a European consortium that will start the clinical trials of a COVID-19 vaccine. The two pharma giants Sanofi and GSK have recently started a collaboration finalized to the development of an adjuvanted COVID-19 vaccine [21 22]
To contribute to the pandemic effort, the COVID-19 High Performance Computing (HPC) Consortium demonstrates cooperation amongst global high tech giants Google, Microsoft, Amazon, and IBM; the HPC Consortium offers services, resources and expertise to support molecular modelling projects as the simulation of SARS-CoV2 entering in a host cell, the high throughput screening of drug candidates, and the evaluation of patients’ genomic features with prognostic values [23].
4. Lockdown & social distance
“The public lacked, in short, standards of comparison. It was only as time passed and the steady rise in the death-rate could not be ignored that public opinion became alive to the truth.”
A. Europe. As the pandemic spread throughout the world, countries took drastic measures to protect their citizens. These measures focused on achieving a fragile balance between limiting virus spread from person to person and maintaining economic activity. It was an impossible balance, although the timing of the implementation of these measures proved to be crucial, both for public health and SARS-CoV2 spread, as well as the economic impact on each country. Early lockdown and strict enforcement were the most effective strategies available to limit virus spread [24,25]. In an accompanying article in this issue, Olagnier & Mogensen describe the implementation of lockdown procedures in Denmark, a country with a remarkably rapid and effective response. The trilogy - social distance, personal hygiene, protective mask – became the mantra throughout Europe and the world.
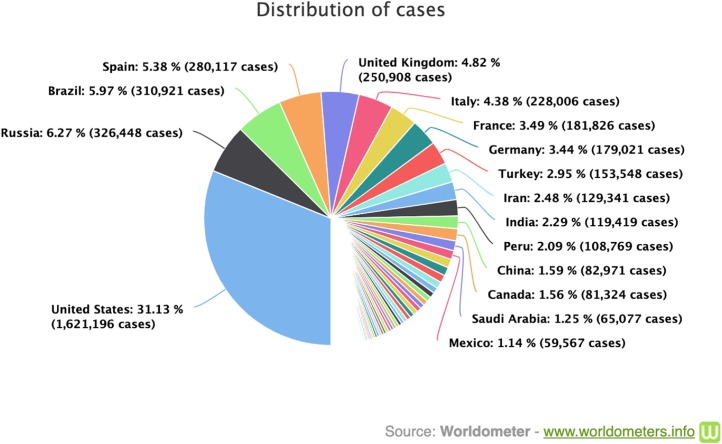
Follow the spread of Covid-19 in a worldwide cases timeline (Fig. 2 ): (https://www.worldometer.info/coronavirus/worldwide-graphs).
Fig. 2.
Global distribution of the Covid-19 cases.
Working in close cooperation with the WHO and EU Member States, the European Union took clear, strict measures, based on the best available scientific expertise. Some member countries faced a significantly limited availability of personal protective equipment (PPE) and the public health systems came close to collapse from the ever-increasing number of severe cases requiring emergency intensive care and ventilation [26]. In some cases, medical equipment destined for other countries was confiscated [27]. On the 20th of March, the EU announced a funding scheme of 1,3 billion euro for bulk purchase of PPE [28]; unfortunately, the UK missed the opportunity to join that funding scheme [29].
In Europe, health systems adapted to the crisis by mobilizing staff, increasing pharmaceutical spending on vaccine development, and optimizing space with the aim to increase the number and availability of intensive care beds capacity. The European average is currently 11.5 critical care beds per 100.000 capita of population [30]; in addition to the shortage of ICU beds and ventilators, the lack of health workers to staff the new units became critical. Countries such as France used army forces and camps to transport patients and optimize care bed capacity [31]. Germany, with the highest proportion of ICU beds per capita of population and one of the best European health systems, campaigned to obtain the medical help of foreign doctors who were living in Germany but did not yet have a license to practice medicine [32]. In Italy, the Netherlands, France and the UK, retired doctors, nurses and medical students were recruited to help [33].
Rather than impose a lockdown of its population, the UK initially followed a mitigation strategy to build population immunity but abandoned this plan after realizing it would result in ‘hundreds of thousands of deaths,’ as noted in a report from the Imperial College's COVID-19 response team [34]. The subsequent illness of the Prime Minister and his transfer to intensive care further contributed to the realization that strict lockdown measures were necessary. Despite ongoing restrictions in the UK, the number of cases continues to rise, the death rate is the highest in Europe and the curve of infections has yet to plateau – a reflection of the lag time before the start of the lockdown.
The Johns Hopkins University (JHU) Coronavirus Resource Center (http//:coronavirus.jhu.edu) provides an important live global update of the spread of SARS-CoV2 that includes world map, US map and critical trends. As of 20th May 2020, the total reported cases in Europe were 1,909,592, and the total deaths are 167,538. The UK currently has the highest number of cases & deaths (250,138 & 35,169), followed by Italy (226, 699 & 32,169), Spain (232,037 & 27,778) and France (180,933 & 25,025).
Sweden similarly followed a plan of ‘voluntary’ social distancing, with the country remaining open. With a population of 10 million, the country remains amongst the top 25 in the world in terms of total number of cases, even though testing is reserved only for those with severe symptoms. These measures have not proved to be effective, and altogether the country has registered 5–10 times more deaths than neighboring Scandinavian countries. The above examples again demonstrate that fast response and strict lockdown saved lives.
JHU lists Sweden with 30,799 cases and 3743 deaths, compared to Denmark (11,315 & 551), Finland (6399 & 301) and Norway (8267 & 233).
Moreover, results from a recent antibody testing study across Spain showed that only 5% of the total number of participants tested positive for exposure to the virus and developed some level of immunity [35,36]. A modelling study, based on data obtained from French hospitals, has shown that by the 11th of May only 4.4 % of the French population had developed potential immunity against SARS-CoV-2 [37] Such numbers, even if remotely accurate, make it clear that letting the infection run its natural course will not result in protection levels high enough to satisfy the criteria of herd-immunity. On the other hand, if such data are interpreted as a low percentage of the population exposed to SARS-CoV-2 in two of the most affected countries in Europe, this showcases a massive positive impact of lockdown measures in containing the spread of the virus.
Lockdowns were not the only measures taken to protect public health. Asian countries which had experience with other viral outbreaks rapidly implemented strict movement restrictions and suspended all unnecessary activities, but in parallel ramped up testing for virus, as well as tracking and isolating cases and contacts [38]. At the same time, China in response to the surge of cases, built new, specially equipped hospitals to increase the number of intensive care beds, while in Korea, hotels were repurposed as care units exclusively for patients suffering from Covid-19. These countries were also the first to ban flights to and from other countries; borders were closed and open only for cargo trade [39,40].
JHU: Many months after the start of the outbreak in China the number of confirmed cases is more than 84,063 and the deaths are 4638; the case fatality ratio is close to 5,5%. As stated on numerous occasions, it is not clear how accurate the Chinese numbers are. Remarkably, in South Korea, the number of cases is 11,110, with only 263 deaths, numbers that reflect the positive impact of in depth efforts in testing, contact tracing and social distancing.
In the pandemic emergency, the lack of PPE and supplies like disinfectants created fear among frontline medics and staff. To draw attention to this aspect, German medical practitioners posed naked on a Twitter page; this protest was inspired by the French doctor Alain Colombié, who affirmed that doctors were being asked “to go to the front without weapons and no defences.” [41]. For the same reason protest marches involving doctors, nurses and paramedics took place in many countries - in Pakistan, they evolved into violent clashes between police and doctors, in Italy, silent flash-mobs protested the government response [42,43]
“Many continued hoping that the epidemic would soon die out and they and their families be spared. Thus, they felt under no obligation to make any change in their habits, as yet. Plague was an unwelcome visitant, bound to take its leave one day as unexpectedly as it had come.”
B. America. The first case of Covid-19 was confirmed in America on January 21 st and a few days later the White House Coronavirus Task Force was established. But with government inaction about the pandemic, weeks were lost when the government could have prepared its own response, informed the public and identified necessary medical supplies. New York City, with its dense population and hundreds of flights a day from Europe, became the epicenter of the pandemic in America. The first New York case was recognized on March 1, 2020, although reports now indicate that by March 1, there may have been as many as 10,000 cases in the state, imported from Italy and elsewhere. Mixed messages from city and state officials, essentially claiming ‘go on with your lives’ at the beginning of March further confused the response. Additional delays in announcing a lockdown and containment practices (the New York Pause was issued March 22) guaranteed the firm establishment of the virus in the city and state. New York Governor Andrew Cuomo became a daily fixture on the news, providing daily updates on the number of cases, the search for proper medical equipment and the courageous efforts of medical front line personnel. However, with more than 15,000 deaths in New York City, the critical need to recognize and respond swiftly to the virus was once again sadly reinforced by the staggering numbers. In contrast, California reacted more swiftly to the emergence of SARS-CoV2, and issued a ‘stay-at-home’ order on March 19, an important decision when hours and days mattered.
JHU: As of May 21st, New York state listed 354,370 cases with 28,636 deaths, while California registered 85,997 cases and 3497 deaths. For comparison the number of cases/deaths in New York City are 194,550 and 15,789, while in San Francisco, there are 2179 cases and 36 deaths.
By the end of March, all 50 states of the USA reported cases of Covid-19. A few weeks after the first Covid-19 case, the hospitals began reporting supply shortages - both for testing and personal protective equipment, a severe safety issue for frontline medical staff that was never addressed nationally. Rather, it was left to state governors to grapple with the purchase supplies on the international market [44]. In mid-March the army started constructing new hospital facilities [45]. As in Europe, large-scale gatherings were prohibited, schools and other educational institutions were closed, businesses shuttered and restrictions on movement were imposed.
JHU: As of 20 May 2020, the total reported cases in USA is 1,528,661, the number of deaths is more than 91,938.
5. Impact on economy
“The truth is that everyone is bored and devotes himself to cultivating habits. Our citizens work hard, but solely with the object of getting rich. Their chief interest is commerce, and their chief aim in life is, as they call it, 'doing business.'”
A. Europe. The eurozone was experiencing poor economic growth even before the shock of the pandemic, with an expansion of just 0.1% for the last three months of 2019. The economic productivity of the 19 countries of the Eurozone decreased by 3.8 % for the first three months of 2020, in the shadow of the spread of coronavirus throughout Europe. Analysts now say it is certain that the entire eurozone will experience the largest recession since its creation in the late 1990s. Germany, France and Italy, the three largest economies in the monetary union, have all entered into economic recession, with Eurostat recording an even bigger drop in gross national product (GDP) compared to what markets expected. Although countries have published data only for the first quarter of 2020, analysts predict an even greater recession for the second and third quarters of the year [[46], [47], [48]].
Of the individual Eurozone countries that published relevant data, France reported that after a recession of 0.1 % for the last quarter of 2019, its economy shrank by 5.8 % for the first 3 months of 2020, the largest recession since the country began recording data in the late 1940s. Italy has also experienced recession for the first half of the year, with the economy shrinking to 4.7 % after falling 0.3 % at the end of 2019. The effects of coronavirus pandemic on an already weak economy were enough to squash it. Spain, one of the countries hit hardest by the pandemic, reported a 5.2 % drop in the first quarter the year, while GDP in Belgium and Austria fell 3.9 % and 2.5 % respectively [46,47].
Germany’s economy shrank by 2.2 % in the first quarter of 2020, as the coronavirus pandemic pushed the eurozone's strongest economy into recession; the seasonally adjusted number of unemployed in Germany jumped by 373,000–2.64 million in April. The jobless rate climbed to 5.8 % from a low of 5% the previous month. The government also increased the number of ‘underemployed’ workers to 10.1 million during April; these part-time employment measures helped to maintain the overall employment figures in Germany [49].
According to Reuters, experts from the World Bank, the World Resources Institute (WRI) and other organizations warn that the coronavirus pandemic will leave behind about 100 million 'new poor’ living in cities around the world due to job losses and income [50,51]. In this scenario, another sad truth must be faced: coronavirus pandemic is widening the gap dividing rich and poor. As for any epidemic, poverty and inequality can exacerbate rates of transmission and mortality. The main factors that sentence poor people to illness are the lack of access to health care, plus poor and crowded living conditions. In the context of the current pandemic, a key mitigating factor in infection risk is the possibility of working remotely, but this is a luxury that a large segment of the workforce doesn’t have. For people who work outside home, the choice is between lose job, lose salary - or keep going out to work amid the pandemic. And because their financial position is more precarious, the only option is to continue to work, travelling in most cases by public transportation, despite the risk of infection for themselves and their families. A primary consequence of this phenomenon is the racial disproportion in sickness and death percentages in the US: African Americans are contracting SARS-CoV2 and dying for it at significantly higher rates compared to white Americans, and this has nothing to do with a biological or genetic predisposition toward coronavirus infection, but is more likely due to a "social predisposition” [52].
In the European Union, it was decided to provide financial assistance of 5% of its GDP to its member states [53, [54]. The worst affected countries can use the funds to alleviate the financial burden of the immediate response measures, including assistance to the population, medical assistance and equipment, support to vulnerable groups, and measures to contain the spread of the disease, strengthen preparedness and communication. Among the various fiscal measures adopted to contain the economic fallout, several governments have decided to defer certain payments, including taxes, loans or utility bills, to improve the liquidity positions of individuals and companies facing difficulties. But, in many cases, those measures are not sufficient.
In Italy, the EU country worst affected by coronavirus, economy has been damaged in such a severe manner that people in some regions are running short of food and money. Many of these “new poor” have turned to charities for help, and several cases of looting at supermarkets have been reported. This critical situation encouraged Italians to give a new twist to an old custom known as “suspended coffee”. In this centuries-old Neapolitan tradition, bar customers pay in advance a coffee for someone who can't afford it. The same concept is being applied to “suspended grocery shopping”: customers buy food with a long shelf-life for the needy - such as pasta and canned goods. "Those who can, put something in, those who can't, help yourself": this is the slogan written on solidarity baskets that appeared in supermarkets, local grocery shops and even on the streets throughout Italy [55]. Beyond these acts of charity, an important help will come from the government, which has designated €400 m for food vouchers to those who can no longer afford groceries [56].
“He knew quite well that it was plague and, needless to say, he also knew that, were this to be officially admitted, the authorities would be compelled to take very drastic steps. This was, of course, the explanation of his colleagues' reluctance to face the facts.”
B. America. The country with the greatest wealth and medical minds in the world failed to heed warnings from China and then Italy; refused to acknowledge the ‘emergency of international concern’ from the World Health Organization on January 31, 2020; and lacked a pandemic preparedness plan that would have mobilized the American health system to respond to the coming viral pandemic as early as February. A failure of national leadership, compounded by the political divisions, and a fragmented state by state response guaranteed the numbers - more than 1.5 million cases and counting, deaths approaching 100,000. It is impossible to imagine that the United States will emerge from this pandemic with the same perspective on its historic economic inequality.
The coronavirus pandemic has already triggered the sharpest recession in the United States since the Great Depression. For the first 2 1/2 months of 2020, the economy continued to grow at a steady pace, but suddenly halted in mid-March - when businesses, travel industries, restaurants and retail shops were abruptly closed, and tens of millions of Americans were ordered to stay home in an effort to slow the spread of SAR-CoV2.More than 35 million people were suddenly out of work and have filed unemployment claims in recent weeks. The spread of the coronavirus has threatened the social and economic fabric of American communities and revealed in a striking way the inequities of the American system – a single event threw more that 35,000,000 people into joblessness and a step closer to poverty. Expanded unemployment benefits and a one-time stimulus package were forthcoming from the US House and Senate, but these are temporary solutions to a much larger structural inequality that the pandemic has exposed. The Covid-19 pandemic highlighted the flaws in the system and revealed two economic conditions that have been left unchecked: poverty and economic insecurity. An inclusive social safety net that includes a basic income and health coverage may be the only solution to ensure that its citizens have a strong foundation for preparedness for the next pandemic.
6. Psychological impact
“Thus, each of us had to be content to live only for the day, alone under the vast indifference of the sky.”
The measures taken to avoid the spread of the new coronavirus have left their mark on the psyche of citizens around the world. At its peak, an estimated 2.6 billion people – or a third of the world’s population – was living under some kind of lockdown or quarantine, arguably the largest psychological experiment ever conducted [57]. Adapting to new, unprecedented conditions brought a change in our daily routine and our habits, and imposed adverse effects on citizens at multiple levels. Fear of death and the end of humanity, loneliness and isolation at home, sadness and anxiety for the next day and the future of our loved ones are the grounds for psychological disorders. Increases in firearm and alcohol sales have been registered in the US over the last two months, clear signs of the stress and anxiety generated by coronavirus pandemic among people [58,59]. Since the onset of social distancing, calls to domestic abuse helplines or suicide hotlines have intensified all over the world [60,61]. France offered free accommodation to victims of violence in the home and encouraged people to ask for help in pharmacies [62]. Australia announced a special phone line named “coronavirus wellbeing support line.” [63]
In late February 2020, before European countries mandated various forms of lockdown, The Lancet published a review documenting the psychological impact of quarantine (the “restriction of movement of people who have potentially been exposed to a contagious disease”). In short, and perhaps unsurprisingly, people who are quarantined are likely to develop a wide range of symptoms of psychological stress and disorder, including low mood, insomnia, stress, anxiety, anger, irritability, emotional exhaustion, depression and post-traumatic stress symptoms [64]. In China, these expected mental health effects are already being reported in the first research papers about the lockdown [65]. A study reporting on the long-term effects of SARS quarantine among healthcare workers found a long-term risk for alcohol abuse, self-medication and long-lasting “avoidance” behavior - where some hospital workers avoid being in close contact with patients by simply not showing up for work. Scientists predict that, if the pandemic continues, psychological and social effects of Covid-19 will worsen and create the “perfect storm” of conditions for suicide, especially in the most vulnerable categories, like the elderly, poor and people suffering from previous mental problems [66].
“Well, personally, I've seen enough of people who die for an idea. I don't believe in heroism; I know it's easy and I've learned that it can be murderous. What interests me is living and dying for what one loves.”
Widespread measures adopted by governments facing the pandemic crisis were social distancing, country-wide lockdown, and restriction of traffic. Numerous constitutionalists have argued that such measures violate human rights, as freedom of movement is a fundamental right directly linked to human nature. However, international human rights law does recognize that during serious public health threats and public emergencies that threaten the life of a nation, restrictions on some rights can be justified.
Various measures have been taken by the majority of the countries to protect human rights in these difficult times. Countries like Ireland, Austria and Argentina have banned the evictions and have announced measures to protect housing, recognizing its role in the crisis response. Portugal announced that people with pending residency and asylum applications will be treated as permanent residents, giving them equal access to free health care [67]. Initially several incidents of racism and xenophobia were reported towards people of Chinese and Asian descent all over the world [68]. Some politicians started to use the term “Chinese Virus” to describe the SARS-Cov-2 pandemic and received criticism for their statements. As the virus spread into European countries and Italy became an epicenter, Italians were also subjected to racism. Unfortunately, such incidents are neither extraordinary nor isolated. Socioeconomic and anthropological/archaeological studies have shown that past pandemics, like the 1918 Spanish Flu and the Black Death in the 14th century, affected societies disproportionally [69]. People at the lower end of the socioeconomic spectrum were more likely to die from infectious diseases due to different treatment practices (or lack thereof) based on their societal status. African Americans, Latinos and indigenous populations have also faced health care inequalities and discriminations during the course of past pandemics. Since the current pandemic does not yet belong to the past, it is a pivotal moment in history to prevent such discriminations and racial inequalities from leaving their social stigma in the years to come.
7. Misinformation
“There comes a time in history when the man who dares to say that two and two do make four is punished with death.”
WHO has repeatedly stated the urgency of adhering to the measures and positions of the scientific community – social distance, personal hygiene and the use of protective masks. But such invasive measures also opened the floodgates of misinformation, with social and mass media spreading a range of questionable information; conspiracy theories, misinformation or non-scientific views regarding the virus, its origin and spread that endanger public health have acquired a criminal character in several countries.
One of the most difficult issues concerned reports that U.S. officials were investigating the possibility that the coronavirus was secretly ‘manufactured’ and/or ‘escaped’ from a Chinese lab in Wuhan, specifically the Wuhan Institute of Virology. There is no scientific evidence to support these theories. The sequencing and analysis of coronavirus genomes have already dispelled these rumors and instead demonstrate that bats are the likeliest source, suggesting that COVID-19 was created by nature, not humans. At its molecular level, the viral genome most closely resembles an isolate that already exists in horseshoe bats in Hunan province. Supported by several studies, bats have an unusually high capacity to harbor viruses and have been linked to past outbreaks, including SARS, MERS and Ebola. The virus may have spread from bats to an intermediary animal before infecting humans; this remains unclear. The fact that the earliest cases of COVID-19 were linked to a live animal market in Wuhan that sold exotic species only bolsters these observations.
In a recent study from Nature Medicine, researchers concluded "Our analyses clearly show that SARS-CoV-2 is not a laboratory construct or a purposefully manipulated virus” [70]. It is well known that the Wuhan Institute of Virology and other Institutes have been studying coronaviruses and bats ever since the SARS outbreak of the early 2000s, but there is no evidence that this research was malicious, rather it was a response to the need to understand the pathogenesis and epidemiology of SARS. High containment research was essential, given earlier outbreaks, as well as warnings from former Presidents and scientific leaders (see above).
In 2003 the Chinese government was legitimately criticized for their attempted cover-up of the original SARS outbreak, leading to skepticism amongst its critics about the openness of its response to the SARS-CoV2 outbreak of 2019. Calls from over 100 nations for an investigation into the origins of SARS-CoV2 and the pandemic have been recognized by Premier Xi of China, with his qualification that the review take place ‘after the virus is under control’. There remains much to learn from the early days of the pandemic and the Chinese response, as well as the pandemic response of other countries. From an epidemiologic perspective, these were critical days; understanding the nature and necessity of the immediate response will only prepare the global community for the next outbreak.
8. An environmental surprise
“What’s true of all the evils in the world is true of plague as well. It helps men to rise above themselves.”
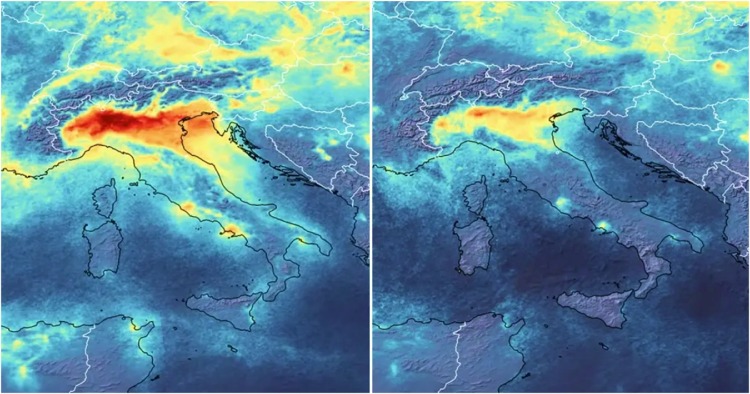
The massive shutdown of industry, business, global travel, farming and personal movement produced an unanticipated beneficial effect on the environment. All over the world, the levels of air pollution dropped [71]; in China, a 25 % reduction in carbon emissions has been reported [72], while in New York, air pollution dropped by 50 %. In northern Italy and central Europe, nitrogen dioxide (NO2) emissions decrease by 5o% (Fig. 3) [73,74].
Fig. 3.
Reduction of NO2 emissions over Northern Italy – January (left) & March (right). https://www.esa.int/ESA_Multimedia/Videos/2020/03/Coronavirus_nitrogen_dioxide_emissions_drop_over_Italy.
To observe statistics and videos of the impact of the coronavirus lockdown on environmental emissions, please visit: https://www.visualcapitalist.com/coronavirus-lockdowns-emissions/
And, in perhaps the most symbolic evidence of the impact of the global pause on the environment, the canals of Venice have cleared; in this video [75] a jelly fish swims in the canal, while Venetian buildings are reflected in the clear water.
9. Conclusion
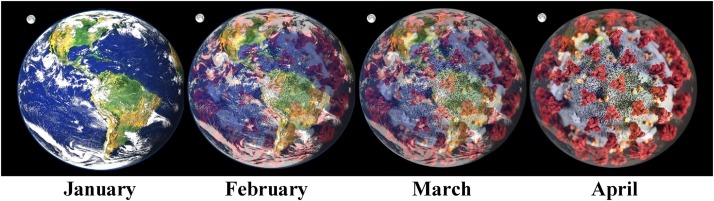
We have reached May 2020 and the lockdown efforts in most countries are winding down. At the time of writing, the population in Italy has moved forward with re-opening the economy; restaurants, stores and businesses are active once again, although the tourists have yet to return. Germany, Spain and France are moving forward with the re-opening their countries after reducing the number of cases and deaths through strict lockdown enforcement. The United States pushes ahead with re-opening business, travel, beaches and bars, despite the continued rise in cases and deaths. And new regions of concern are emerging; Brazil and Russia report massive daily increases in the number of cases and are now becoming the new epicenters, with the second and third highest rates of infection in the world. Singapore and China are carefully evaluating spikes in new cases - using testing, contact tracing and isolation to prevent a ‘second wave’ of coronavirus cases. Research and vaccine development are moving at ‘warp speed’ in the hopes of finding a treatment that will restore us to a new normal. In the first four months of 2020, Covid-19 has engulfed the world; it remains to be seen if global efforts during the next four months will unwrap our planet (Fig. 4 ).
Fig. 4.
Wrapped in Corona. A schematic view of the world as SARS-CoV-2 engulfs the planet.
The pandemic continues. Although it is not clear whether the virus will continue to smolder and ignite in different global regions during the summer, or perhaps retreat, only to return to new peaks in the fall and winter, most experts agree that Covid-19 is not going away anytime soon, and will probably be with us for the next two years [76]. On May 21st, the WHO reported 106,000 new cases of Covid-19 globally, the highest one day total since the pandemic began. As new knowledge about the virus accumulates, new complications of the disease arise, including the recent recognition of a serious Kawasaki-like disorder in children, termed multi-system inflammatory syndrome (MIS). And new modelling research states that had the lockdown of America been imposed two weeks earlier - March 9 vs March 23 - over 80 % of the cases and deaths could have been prevented. This sobering estimate brings us to another unsettling fact; throughout this crisis, efforts have been made to mute and even ridicule the response of scientific leadership to the pandemic. If Covid-19 ushers in a ‘new normal’ for citizens around the world, we hope that new reality will include the recognition that the voice of science, reason and experience must be heard.
Acknowledgements
The authors wish to thank Michaela Muscolini, Evelyne Tassone and Enrico Palermo for critical reading and comments. The authors also thank the students of INITIATE, the Marie Curie International Training Network for their scientific perspectives and writings during this pandemic period. Quotations in italics from Albert Camus, The Plague. This project was supported by funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 813343 for the Marie Curie ITN INITIATE program.
References
- 1.World Health Organization . 2020. WHO Announces COVID-19 Outbreak a Pandemic. [Online] Available at: http://www.euro.who.int/en/heps//:coronavirus.jhu.edu/map.alth-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (Accessed 1 May 2020) March 12. [Google Scholar]
- 2.Ciulla M.M. History repeating. The plague of 1630 in Milan and the COVID-19 pandemia. Acta Biomed. 2020;91(2):234–235. doi: 10.23750/abm.v91i2.9553. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collins F.S., Stoffels P. Accelerating COVID-19 therapeutic interventions and vaccines (ACTIV): an unprecedented partnership for unprecedented times. JAMA. 2020 doi: 10.1001/jama.2020.8920. [DOI] [PubMed] [Google Scholar]
- 4.Baker N. These cancer scientists turned their lab into a coronavirus-testing facility. Nature. 2020;580(7804):441. doi: 10.1038/d41586-020-01109-x. [DOI] [PubMed] [Google Scholar]
- 5.Gewin V. On the front lines of the coronavirus-vaccine battle [published online ahead of print, 2020 Apr 16] Nature. 2020 doi: 10.1038/d41586-020-01116-y. [DOI] [PubMed] [Google Scholar]
- 6.Betti F., Heinzmann T. 2020. World Economic Forum. From Perfume to Hand Sanitiser, TVs to Face Masks: How Companies Are Changing Track to Fight COVID-19. [Online] https://www.weforum.org/agenda/2020/03/from-perfume-to-hand-sanitiser-tvs-to-face-masks-how-companies-are-changing-track-to-fight-covid-19/ Accessed on 21 May. [Google Scholar]
- 7.Viglione G. Tens of thousands of scientists are redeploying to fight coronavirus [published online ahead of print, 2020 Mar 27] Nature. 2020 doi: 10.1038/d41586-020-00905-9. [DOI] [PubMed] [Google Scholar]
- 8.Kupferschmidt K. Preprints bring’ firehose’ of outbreak data. Science. 2020;367(6481):963–964. doi: 10.1126/science.367.6481.963. [DOI] [PubMed] [Google Scholar]
- 9.Kupferschmidt K. Coronavirus outbreak changes how scientists communicate. Science. 2020 doi: 10.1126/science.abb4761. [DOI] [Google Scholar]
- 10.Zastrow M. Open science takes on the coronavirus pandemic. Nature. 2020;581(7806):109–110. doi: 10.1038/d41586-020-01246-3. [DOI] [PubMed] [Google Scholar]
- 11.European Commission COVID-19: Commission steps up research funding and selects 17 projects in vaccine development. treatment and diagnostics. 2020;(6 March) [Online] https://ec.europa.eu/commission/presscorner/detail/en/ip_20_386 accessed on 6 May 2020. [Google Scholar]
- 12.European Commission, COVID-19: Horizon . 2020. Partly Funding Innovative Medicines Initiative Fast Track Call, 3 March 2020. [Online] https://ec.europa.eu/info/news/covid19-horizon-2020-partly-funding-innovative-medicines-initiative-fast-track-call-2020-mar-03_en accessed on 6 May 2020. [Google Scholar]
- 13.European Commission . 2020. Coronavirus Global Response: €7.4 Billion Raised for Universal Access to Vaccines. 4 May, [Online] https://ec.europa.eu/commission/presscorner/detail/en/ip_20_797 Accessed on 6 May 2020. [Google Scholar]
- 14.UK research and innovation . 2020. UK Launches Whole Genome Sequence Alliance to Map Spread of Coronavirus. 23 March [Online] https://www.ukri.org/news/uk-launches-whole-genome-sequence-alliance-to-map-spread-of-coronavirus/ accessed on 6 May 2020. [Google Scholar]
- 15.UK research and innovation . 2020. COVID-19 Vaccine & Therapy Research Boosted by Six New Projects in Rapid Response. 23 March, [Online] https://www.ukri.org/news/covid-19-vaccine-therapy-research-boosted-by-six-new-projects-in-rapid-response/ accessed on 6 May 2020. [Google Scholar]
- 16.Le T.T., Andreadakis Z., Kumar A., Roman R.G., Tollefsen S., Saville M., Mayhew S. The COVID-19 vaccine development landscape. Nat. Rev. Drug Discov. 2020;19:305–306. doi: 10.1038/d41573-020-00073-5. [DOI] [PubMed] [Google Scholar]
- 17.Khuroo M., Khuroo M., Sofi A., Khuroo N. COVID-19 Vaccines: A Race Against Time in the Middle of Death and Devastation! Preprints. 2020 doi: 10.20944/preprints202005.0223.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institutes of Health . 2020. NIH To Launch Public-private Partnership to Speed COVID-19 Vaccine and Treatment Options. 17 April, [Online] https://www.nih.gov/news-events/news-releases/nih-launch-public-private-partnership-speed-covid-19-vaccine-treatment-options, Accessed on 6 May 2020. [Google Scholar]
- 19.Moderna Announces Positive Interim Phase . 2020. 1 Data for Its mRNA Vaccine (mRNA-1273) Against Novel Coronavirus – 18 May 2020. [Online] https://investors.modernatx.com/news-releases/news-release-details/moderna-announces-positive-interim-phase-1-data-its-mrna-vaccine/ Accessed on 21 May. [Google Scholar]
- 20.Mahase Elisabeth. Covid-19: what do we know so far about a vaccine? BMJ. 2020:369. doi: 10.1136/bmj.m1679. [DOI] [PubMed] [Google Scholar]
- 21.2020. Biopharma Products in Development for COVID-19. [Online] https://www.bioworld.com/COVID19products#vac Accessed on 6 May. [Google Scholar]
- 22.Vabret N., Britton G.J., Gruber C., Hegde S., Kim J., Kuksin M., Levantovsky R., Malle L., Moreira A., Park M.D., Pia L., Risson E., Saffern M., Salomé B., Selvan M.E., Spindler M.P., Tan J., van der Heide V., Gregory J.K., Alexandropoulos K., Bhardwaj N., Brown B.D., Greenbaum B., Gümüş Z.H., Homann D., Horowitz A., Kamphorst A.O., Curotto de Lafaille M.A., Mehandru S., Merad M., Samstein R.M. The sinai immunology review project, immunology of COVID-19: current state of the science. Immunity. 2020 doi: 10.1016/j.immuni.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.COVID-19 HPC Consortium . 2020. The COVID-19 High Performance Computing Consortium. [Online], https://covid19-hpc-consortium.org/, Accessed on 6 May 2020. [Google Scholar]
- 24.Guzzetta G., Riccardo F., Marziano V. 2020. The Impact of a Nation-wide Lockdown on COVID-19 Transmissibility in Italy. Submitted on 26 Apr. Arxiv.org arXiv:2004.12338. [Google Scholar]
- 25.Cheng S.O., Khan S. Europe’s response to COVID-19 in March and April 2020 - A letter to the editor on “World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19)” (Int J Surg 2020;76:71-76) [published online ahead of print, 2020 Apr 14] Int. J. Surg. 2020;78:3–4. doi: 10.1016/j.ijsu.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feuer W., News C.N.B.C. 2020. WHO Officials Warn Health Systems Are “collapsing” Under Coronavirus: This Isn’t Just a Bad Flu Season. March 20) [Online] Available at: https://www.cnbc.com/2020/03/20/coronavirus-who-says-health-systems-collapsing-this-isnt-just-a-bad-flu-season.html (Accessed 1 May 2020) [Google Scholar]
- 27.BBC News . 2020. Coronavirus: US Accused of “piracy” Over Mask “confiscation”. April 4) [Online] Available at: https://www.bbc.com/news/world-52161995 (Accessed 1 May 2020) [Google Scholar]
- 28.European Council . 2020. Personal Protective Equipment (PPE) [Online] Available at: https://ec.europa.eu/growth/sectors/mechanical-engineering/personal-protective-equipment_en (Accessed 1 May 2020) [Google Scholar]
- 29.Boffey D., Booth R. 2020. The Guardian (2020, April 13), UK Missed Three Chances to Join EU Scheme to Bulk-buy PPE. [Online] Available at: https://www.theguardian.com/world/2020/apr/13/uk-missed-three-chances-to-join-eu-scheme-to-bulk-buy-ppe (Accessed 1 May. [Google Scholar]
- 30.Rhodes A., Ferdinande P., Flaatten H. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38:1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 31.News Wires, France24 . 2020. French Military to Support Public Services As Country’s Coronavirus Toll Rises. [Online], March 26)Available at: https://www.france24.com/en/20200326-french-military-to-support-public-services-as-country-s-coronavirus-toll-grows (Accessed 1 May 2020) [Google Scholar]
- 32.Connolly K. 2020. The Guardian 2020, Germany Calls on Migrant Medics to Help Tackle Coronavirus. [Online] April 14)Available at: https://www.theguardian.com/world/2020/apr/14/germany-calls-on-migrant-medics-to-help-tackle-coronavirus (Accessed 1 May. [Google Scholar]
- 33.Kottasova I., CCN . 2020. Thousands of Medical Students Are Being Fast-tracked Into Doctors to Help Fight the Coronavirus. [Online] March 20)Available at: https://edition.cnn.com/2020/03/19/europe/medical-students-coronavirus-intl/index.html (Accessed 1 May 2020) [Google Scholar]
- 34.Walker P. 2020. Report 12: the Global Impact of COVID-19 and Strategies for Mitigation and Suppression. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.[Online] https://www.lamoncloa.gob.es/serviciosdeprensa/notasprensa/sanidad14/Documents/2020/130520-ENE-COVID_Informe1.pdf.Study from Carlos III Institute of Health and the National Statistics Institute, Spain, regarding the first round of antibody testing which showed only 5% of the population tested had been infected with SARS-CoV-2.
- 36.Salje H. Estimating the burden of SARS-CoV-2 in France. Science. 2020 doi: 10.1126/science.abc3517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Covid-19 Wise J. Surveys indicate low infection level in community. BMJ. 2020;369(May 18):m1992. doi: 10.1136/bmj.m1992. Published 2020. [DOI] [PubMed] [Google Scholar]
- 38.En Tan G.S., Hou A., Manauis C.M., Chua J.M., Gao C.Q., Kiat Ng F.K., Wong C.S., Ng O.T., Marimuthu K., Chan M., Leo Y.S., Vasoo S. Reducing hospital admissions for COVID-19 at a dedicated Screening Centre in Singapore. Clin. Microbiol. Infect. 2020 doi: 10.1016/j.cmi.2020.05.005. S1198-743X(20)30282-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sohrabi Catrin. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee V.J., Chiew C.J., Khong W.X. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. J. Travel Med. 2020 doi: 10.1093/jtm/taaa039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Woodyatt Amy. 2020. German Doctors Pose Naked to Protest Protective Equipment Shortages CNN. 28 April 2020, [Online] https://edition.cnn.com/2020/04/28/europe/german-doctors-naked-protest-intl-scli-grm/index.html accessed on 6 May. [Google Scholar]
- 42.Ilyas Khan M. 2020. Coronavirus: Why Pakistan’s Doctors Are so Angry, BBC News. 10 April 2020, [Online] https://www.bbc.com/news/world-asia-52243901, accessed on 6 May. [Google Scholar]
- 43.Poletto L., Romano P. 2020. Coronavirus, la rivolta di medici e infermieri: “Eroi nei titoloni, trattati da straccioni”, La Stampa. 30 April 2020, [Online] https://www.lastampa.it/torino/2020/04/30/news/coronavirus-la-rivolta-di-medici-e-infermieri-eroi-nei-titoloni-trattati-da-straccioni-1.38788301 Accessed on 6 May. [Google Scholar]
- 44.Schlanger Z. 2020. Begging for Thermometers, Body Bags, and Gowns: U.S. Health Care Workers Are Dangerously Ill-Equipped to Fight COVID-19. [Online] Available at: https://time.com/5823983/coronavirus-ppe-shortage/ (Accessed 1 May 2020) Time (April 20) [Google Scholar]
- 45.Babb C., News Voa. 2020. US Army Hard-Pressed to Build Temporary Hospitals Before COVID-19. [Online] Available at: https://www.voanews.com/science-health/coronavirus-outbreak/us-army-hard-pressed-build-temporary-hospitals-covid-19-peak (Accessed 1 May 2020) (, April 8) [Google Scholar]
- 46.European Council . 2020. Coronavirus Global Response. [Online] Available at: https://ec.europa.eu (Accessed 1 May 2020) [Google Scholar]
- 47.European Council, Eurostat . 2020. GDP Down by 3.8% in the Euro Area and by 3.5% in the EU. [Online] Available at: https://ec.europa.eu/eurostat/documents/2995521/10294708/2-30042020-BP-EN.pdf/526405c5-289c-30f5-068a-d907b7d663e6 (Accessed 1 May 2020) (April 30) [Google Scholar]
- 48.McKee M., Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat. Med. 2020 doi: 10.1038/s41591-020-0863-y. [DOI] [PubMed] [Google Scholar]
- 49.Financial Times . 2020. Germany Braced for Jobless Surge As Companies Rush for State Funds. [Online] Available at: https://www.ft.com/content/5486b247-c73e-4887-a2b2-528b23e301a6 (Accessed 1 May 2020) [Google Scholar]
- 50.Moloney A. 2020. Cities Face 100 Million “new Poor” in Post-pandemic World: Experts. [Online] Available at: https://www.reuters.com/article/us-health-coronavirus-cities-trfn/cities-face-100-million-new-poor-in-post-pandemic-world-experts-idUSKBN22B3GG (Accessed 1 May 2020) Reuters (2020, April 30) [Google Scholar]
- 51.Anser M.K., Yousaf Z., Khan M.A., Nassani A.A., Alotaibi S.M., Qazi Abro M.M., Vo X.V., Zaman K. Does communicable diseases (including COVID-19) may increase global poverty risk? A cloud on the horizon. Environ. Res. 2020;187 doi: 10.1016/j.envres.2020.109668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yancy C.W. COVID-19 and african americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 53.Press Release, European Council . 2020. Report on the Comprehensive Economic Policy Response to the COVID-19 Pandemic. [Online] Available at: https://www.consilium.europa.eu/el/press/press-releases/2020/04/09/report-on-the-comprehensive-economic-policy-response-to-the-covid-19-pandemic/ (Accessed 1 May 2020) (, April 9) [Google Scholar]
- 54.European Union . 2020. EU Solidarity Fund for COVID-19. [Online] Available at : https://ec.europa.eu/regional_policy/en/funding/solidarity-fund/covid-19 (Accessed 1 May 2020) [Google Scholar]
- 55.Sannino C., Repubblica, 1 April 2020 [Online] https://rep.repubblica.it/pwa/rubrica/omissis/2020/04/01/news/chi_puo_metta_chi_non_puo_prenda-252773346/ Accessed on 6 May 2020.
- 56.Giuffrida A., Tondo L. 2020. The Guardian. [Online] https://www.theguardian.com/world/2020/apr/01/singing-stops-italy-fear-social-unrest-mount-coronavirus-lockdown Accessed on 6 May 2020, 1 April. [Google Scholar]
- 57.Jankowicz M. 2020. More People Are Now in’ Lockdown’ Than Were Alive During World War II. [Online] https://www.sciencealert.com/one-third-of-the-world-s-population-are-now-restricted-in-where-they-can-go Accessed:-05-19. [Google Scholar]
- 58.Brauer J., U . 2020. .S. Firearms Sales: March 2020 Unit Sales Show Anticipated covid-19-related Boom. [Online] http://smallarmsanalytics.com/v1/pr/2020-04-01.pdf accessed on 4 April. [Google Scholar]
- 59.Polakovic G., USC news, 14 april 2020, [Online] https://news.usc.edu/168549/covid-19-alcohol-sales-abuse-stress-relapse-usc-experts/ (accessed on 19 May 2020).
- 60.Boserup B., McKenney M., Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am. J. Emergency Med. 2020;28(April) doi: 10.1016/j.ajem.2020.04.077. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Campbell A.M. An increasing risk of family violence during the Covid-19 pandemic: strengthening community collaborations to save lives. Forensic Sci. Int. Reports. 2020;2 doi: 10.1016/j.fsir.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kottasova I., Di Donato V. 2020. Women Are Using Code Words at Pharmacies to Escape Domestic Violence During Lockdown. [Online] Available at :https://edition.cnn.com/2020/04/02/europe/domestic-violence-coronavirus-lockdown-intl/index.html (Accessed 1 May 2020) CNN (, April 6) [Google Scholar]
- 63.Herniques-Gomes L., Smee B. 2020. The Guardian (2020, April 27), Australia Launches Covid-19 Contact Tracing App, As WA and Qld Announce Plans to Relax Restrictions – As It Happened. [Online] Available at : https://www.theguardian.com/australia-news/live/2020/apr/26/australia-coronavirus-update-latest-scott-morrison-economy-health-nsw-victoria-queensland-schools-live-news (Accessed 1 May. [Google Scholar]
- 64.Brooks Samantha K. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(February 26 (10227)):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations [published correction appears in Gen Psychiatr. 2020 Apr 27;33(2):e100213corr1] Gen Psychiatr. 2020;33(2):e100213. doi: 10.1136/gpsych-2020-100213. Published 2020 Mar 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Brown S., Schuman D.L. Suicide in the time of COVID-19: a perfect storm. J. Rural. Health. 2020;(03 May) doi: 10.1111/jrh.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schengen Visa Info . 2020. Portugal Grants Migrants and Asylum Seekers Full Citizenship Rights During COVID-19 Outbreak. [Online] Available at : https://www.schengenvisainfo.com/news/portugal-grants-migrants-and-asylum-seekers-full-citizenship-rights-during-covid-19/ (Accessed 1 May 2020) (, April 2) [Google Scholar]
- 68.Devakumar D., Shannon G., Bhopal S.S., Abubakar I. Racism and discrimination in COVID-19 responses. Lancet. 2020 doi: 10.1016/S0140-6736(20)30792-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wade L. An unequal blow. Science. 2020;368(6492):700–703. doi: 10.1126/science.368.6492.700. [DOI] [PubMed] [Google Scholar]
- 70.Andersen K.G., Rambaut A., Lipkin W.I. The proximal origin of SARS-CoV-2. Nat. Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chauhan A., Singh R.P. Decline in PM2.5 concentrations over major cities around the world associated with COVID-19. Environ. Res. 2020;187(May 5):109634. doi: 10.1016/j.envres.2020.109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bao R., Zhang A. Does lockdown reduce air pollution? Evidence from 44 cities in northern China. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.139052. https://doi.org/10.1016/j.scitotenv.2020.139052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.[Online] https://www.visualcapitalist.com/coronavirus-lockdowns-emissions/.
- 74.Collivignarelli M.C., Abbà A., Bertanza G., Pedrazzani R., Ricciardi P., Carnevale Miino M. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci. Total Environ. 2020;732(May 8):139280. doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.[Online] https://www.youtube.com/watch?v=5zDqYvjld18.
- 76.Jones D.S. History in a crisis-Lessons for Covid-19. New Eng. J. Med. 2020;382:1681–1683. doi: 10.1056/NEJMp2004361. [DOI] [PubMed] [Google Scholar]