Abstract
Persistent scar pain associated with healed surgical incisions after a trauma is a common and potentially debilitating type of fascial pain. At present, there is no universally effective treatment for persistent surgical or post-trauma scar pain. Herein we describe the successful objective diagnosis of debilitating scar pain by Ultrasound (US) imaging. The sonopalpation of the fasciae and subcutaneous tissues seems to be relevant to diagnose the real cause of the pain and why not to monitor the treatment.
Key Words: Ultrasonography, scar, fascia, knee, pain
Ethical Publication Statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
A scar is the natural result of the wound healing process that follows surgery or many types of trauma. Depending on their physical features, scars can deeply impact the patient’s quality of life from a functional, cosmetic, or psychological point of view. An accurate scar assessment is fundamental to identify the real reason of the scar pain and the scar evolution, helping in the selection of appropriate therapeutic options.1 Although there are numerous tools for scar assessment, there is no consensus on which is appropriate for each type of scar.2,3 Defining a specific treatment plan in the treatment of the scars requires a clear understanding of the underlying tissue. Ultrasonography is a useful tool to visualize the fascial layers4 and nowadays is widely used in daily rehabilitation practice.5 Sonopalpation is a new manner to use the probe to identify the reason of the major symptom, the pain.5 However most ultrasound machines cannot assess the mechanical properties of subcutaneous tissue such as its stiffness, i.e., the ability of the subcutaneous tissue to be compressed, elongated, stretched or manipulated, which are essential for normal movement and consequently crucial to plan a rehabilitative treatment following the regenerative process. To our knowledge, no other papers have assessed the degree of scar adherence to the fascial layers; only one scale has been developed for adherent scars (the Skin Glide Grade scale, which subjectively grades the amount of scar restriction).6 Because there is not currently a consensus on this topic, we think it would be relevant for the specialist in physical and rehabilitation medicine to assess with the ultrasound imaging these relationship with the fascial layers. This assessment could help to plan the treatment and to diagnose the real pain generator in these patients.
Case Presentation
A 30-year-old female was seen for a ragged wound on her right knee after a traffic accident (occurred 3 years earlier). She reported that she was not able to flex her knee due to severe pain and that the wound had been sutured twice for healing complications. Plain radiographs had been negative and medical treatment, including cold pack and oral/topical non-steroidal anti-inflammatory drugs, had been ineffective. The medical history was otherwise unremarkable and she was currently seen for ultrasound (US) examination of her knee. Pre-scanning physical examination of the knee joint was normal except tenderness over the scar region and mild limitations of knee flexion and extension. Comparative knee US imaging 7 - performed using a high frequency linear probe (4-16 MHz, Sonosite Edge II, FUJIFILM) - was normal. To precisely evaluate the site of maximum pain (indicated by the patient), longitudinal scanning over the patella was performed, again comparatively (Fig. 1, A and B). US imaging demonstrated thickening of the subcutaneous tissue of the injured knee (right = 2.33 mm, left = 1.31 mm) and, in particular, of the superficial fascia with hyperechoic thickening of the retinacula cutis (Fig. 1C). Sono-palpation of the scar stretched the retinacula cutis (Fig.1 D and E) and caused significant pain (Fig. 2 A, B).
Discussion
Skin tissue repair after surgical intervention can result in a broad spectrum of scar types, ranging from a fine line to a variety of abnormal and pathologic scars, which can have functional, cosmetic and psychological consequences.8,9 The assessment is fundamental for monitoring scar evolution and treatment efficacy, and quantifying its importance in clinical and forensic settings.10 Scars usually develop in 6–8 weeks after reepithelialisation, and a period of at least 6–18 months is required for their maturation.11 The European Tissue Repair Society recommends performing 3 different assessments at the end of the 1st, 2nd and 3rd month after wound closure.12 The first clinical assessment determines the general features of the scar: at this stage, color and vascularity seems the most important parameters to analyze. At the 2nd month, changes in width, height and color are more evident, while at the 3rd month possible hypertrophy is visible, and it is possible to observe trouble in pliability and texture. In the literature, scar assessment has mainly been focused on burn scars, but interest in postsurgical and post-trauma scars is increasing.13 Often the same evaluating instruments are used in both conditions, even if the two kinds of scar frequently present different features. For example, although burn scars may occupy larger surface areas with more variations present over the area, postsurgical scars are mostly linear or round-shaped and well-defined. The ideal scar assessment scale should be easy to use in daily practice, reliably quantify the magnitude of pathologic complications, monitor the effects of prevention or treatment interventions, and analyze the impact of the scar on the patient’s activities, social participation and quality of life integrating clinician observations with patient-based symptoms.13 However, the sonopalpation of the fasciae and subcutaneous tissue is not an inherent part of the instrument but should be evaluated within the context of the tests used and the specific target population. Thus, the appropriateness of these tools for postsurgical scars should be always specifically demonstrated. Pain is a common symptom during wound healing and it generally occurs in the initial phase as a result of tissue damage. Pain complaints generally fade during the phases of wound healing and cease in the maturation phase of healing when a scar has formed. If a matured scar is still painful, for Curtin et al (2009)15 one possible cause of this pain is a neuroma, which originates from a regenerating nerve trapped in fibrotic dermal scar tissue. Neuromas have a typical clinical presentation (positive Tinel sign, numbness in the innervation area of the injured nerve) and treatment can be directed to eliminate the neuroma.14 Unfortunately, some patients have painful scars without the typical symptoms accompanying a neuroma. The prevalence of pain symptoms in different scar types like hypertrophic scars and keloids and the mechanisms behind them are largely unknown. As in our case, the sensitization could be determined by an alteration of the superficial fascia; and during movements, the retinacula cutis or skin ligaments become more fibrous - stretching the skin instead of adapting.15,16
Fig 1.
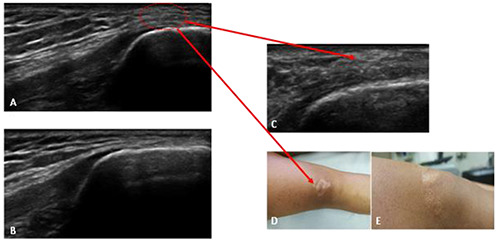
Longitudinal scanniong. A, Right knee: thickening of the subcutaneous tissue. B, Left knee. Normal profile of subcutaneous tissue. C, Reorganization of the subcutaneous tissue on the surface of the patella. D, E, Scar tissue at physical exam, respectively and from side.
Fig 2.
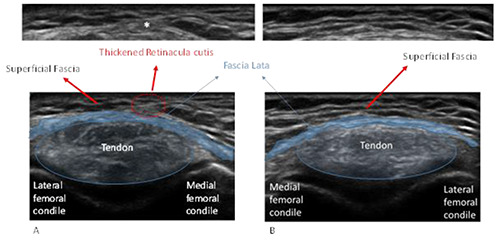
Transversal scanning. A, Right knee with thickening of retinacula cutis and superficial fascia. B, Left knee, normal organization of subcutaneous tissue. *,Thickening of retinacula cutis and superficial fascia
The entire subcutaneous tissue is transformed into fibrous tissue that creates a rigid connection between skin and deep fascia. Every time mechanical stress is applied to scar tissue the deep fascia is also stressed causing activation of its receptors. This may explain why stressing scars can result in a disorganized afferentation and probable overstimulation of certain receptors resulting in over sensitive and painful scar tissue areas.17 On US imaging, it was evident that the epidermis became irregular as it was pulled up by retinacula cutis in our patient. Normally, separated from the deep fascia, the superficial fascia is seen as a hyperechoic line that divides the subcutaneous tissue into two distinct parts. It is more evident in other topographic regions where it is sometimes composed of two layers. Being close to the upper region of the knee where the superficial and deep fasciae are fused; in our case, it was likely that the pain had ensued due to hypersensitivity of these tissues after the scar. Yet, while the course and innervation of the fascial layers are different than those of the skin; close to the joints they are common.18 Probably, during the healing process, the reorganization of the subcutaneous tissue caused stress and traction on the fascial layers in our patient. Herein, we wish to underscore the importance of US examination especially for different layers of the skin and subcutaneous tissues. Of note, the possibility of adding ‘sono-palpation’ to the examination is invaluable either for the initial diagnosis or the follow up of relevant patients.
In conclusion, assessment and treatment of pathologic scars should be part of the routine management of postsurgical and trauma conditions of the locomotor system and their relationship with the fasciae as generator of pain. In order to generate an effective treatment against painful scars we need to know the extent of the problem, the underlying mechanisms causing pain and underlying state of tissues. To date, US imaging with the tool of the sonopalpation could be considered in the daily practice of the specialist in physical and rehabilitation medicine, being particularly objective because it takes into account the importance of the pain generator in patients with scar.
Acknowledgments
The Authors thank colleagues of the Department of Neurosciences, University of Padova, Italy and of the A&C M-C Foundation for Translational Myology, Padova, Italy for discussions and critical readings.
List of acronyms
- US imaging
Ultrasound imaging
Funding Statement
Funding: None
Contributor Information
Antonio Stecco, Email: antonio.stecco@nyumc.org.
Caterina Fede, Email: caterina.fede@unipd.it.
Raffaele De Caro, Email: r.decaro@unipd.it.
Carla Stecco, Email: carla.stecco@unipd.it.
Levent Özçakar, Email: lozcakar@yahoo.com.
References
- 1.Franchignoni F, Giordano A, Vercelli S, et al. Rasch Analysis of the Patient and Observer Scar Assessment Scale in Linear Scars: Suggestions for a Patient and Observer Scar Assessment Scale v2.1. Plast Reconstr Surg 2019;144:1073e-1079e. [DOI] [PubMed] [Google Scholar]
- 2.Vercelli S, Ferriero G, Sartorio F, et al. Clinimetric properties and clinical utility in rehabilitation of postsurgical scar rating scales: A systematic review. Int J Rehabil Res 2015;38:279–86. [DOI] [PubMed] [Google Scholar]
- 3.Van der Wal MB, Verhaegen PD, Middelkoop E, van Zuijlen PP. A clinimetric overview of scar assessment scales. J Burn Care Res 2012;33:e79–e87. [DOI] [PubMed] [Google Scholar]
- 4.Pirri C, Stecco C, Fede C, Macchi V, Özçakar L. Ultrasound Imaging of the Fascial Layers: You See (Only) What You Know. J Ultrasound Med 2019. Oct 23. doi:10.1002/jum.15148. [DOI] [PubMed] [Google Scholar]
- 5.Özçakar L, Kara M, Chang KV, et al. Nineteen reasons why physiatrists should do musculoskeletal ultrasound: EURO-MUSCULUS/USPRM recom menddations. Am J Phys Med Rehabil 2015;94(6):e45-9. doi: 10.1097/PHM.000000000 0000223. [DOI] [PubMed] [Google Scholar]
- 6.Silverberg R, Johnson J, Moffat M. The effects of soft tissue mobilization on the immature burn scar: Results of a pilot study. J Burn Care Rehabil 1996;17:252–9. [DOI] [PubMed] [Google Scholar]
- 7.Özçakar L, Kara M, Chang KV, et al. EURO-MUSCULUS /USPRM basic scanning protocols for knee. Eur J Phys Rehabil Med 2015;51:641-6. [PubMed] [Google Scholar]
- 8.Mustoe TA, Cooter RD, Gold MH, et al. International clinical recommendations on scar management. Plast Reconstr Surg 2002;110:560–71. [DOI] [PubMed] [Google Scholar]
- 9.Vercelli S, Ferriero G, Sartorio F, et al. How to assess postsurgical scars: a review of outcome measures. Disabil Rehabil 2009;31:2055-63. [DOI] [PubMed] [Google Scholar]
- 10.Roques C, Te´ot L. A critical analysis of measurements used to assess and manage scars. Int J Low Extrem Wounds 2007;6:249–53. [DOI] [PubMed] [Google Scholar]
- 11.Atiyeh BS. Nonsurgical management of hypertrophic scars: evidence-based therapies, standard practices, and emerging methods. Aesth Plast Surg 2007;31:468–92. [DOI] [PubMed] [Google Scholar]
- 12.Te´ot L. Scar evaluation and management: recommendations. Eur Tissue Repair Soc Bull 2005;12:1–11. [Google Scholar]
- 13.Truong PT, Lee JC, Soer B, et al. Reliability and validity testing of the Patient and Observer Scar Assessment Scale in evaluating linear scars after breast cancer surgery. Plast Reconstr Surg 2007;119:487–94. [DOI] [PubMed] [Google Scholar]
- 14.Powers PS, Sarkar S, Goldgof DB, et al. Scar assessment: current problems and future solutions. J Burn Care Rehabil 1999;20:54–60. [DOI] [PubMed] [Google Scholar]
- 15.Curtin C, Carrol I. Cutaneous neuroma physiology and its relationship to chronic pain. J Hand Surg (USA) 2009;34:1334-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lancerotto L, Stecco C, Macchi V, et al. Layers of the abdominalwall: anatomical investigation of subcutaneous tissue and superficial fascia. Surg Radiol Anat 2011;33: 835–42. [DOI] [PubMed] [Google Scholar]
- 17.Stecco C. Functional Atlas of the Human Fascial System. UK: Elsevier Health Sciences; 2015. [Google Scholar]
- 18.Stecco C, Pirri C, Fede C, et al. Dermatome and fasciatome. Clin Anat 2019. May 14. doi:10.1002/ca.23408. [DOI] [PubMed] [Google Scholar]
- 19.Barford A, Dorling D, Smith G, Shaw M. Life expectancy: women now on top everywhere. BMJ 2006;332(7545):808. [DOI] [PMC free article] [PubMed] [Google Scholar]


