Supplemental Digital Content is available in the text
Keywords: adductor canal block, length of hospital stay, nausea and vomiting, opioid consumption, range of motion, total knee arthroplasty
Abstract
Background:
The adductor canal block (ACB) has emerged as an alternative to the femoral nerve block (FNB) after total knee arthroplasty. This meta-analysis was conducted to investigate which ACB method provides better pain relief and functional recovery after total knee arthroplasty
Methods:
We conducted a meta-analysis to identify randomized controlled trials involving single-shot adductor canal block (SACB) and continuous catheter ACB (CACB) after TKA up to December 2019 by searching databases including the PubMed, Web of Science, Embase, Cochrane Controlled Trials Register, Cochrane Library, CBM, CNKI, VIP, and Wanfang databases. Finally, we included 8 randomized controlled trials involving 702 knees in our study. We used Review Manager Software and Grading of Recommendations Assessment, Development, and Evaluation profiler to perform the meta-analysis.
Results:
Compared with SACB, CACB can achieve better postoperative pain relief at 24 and 48 h both at rest and after mobilization, lower amount of opioid consumption at 72 h, a shorter length of hospital stay (LOH) and larger range of motion (ROM). In addition, the Timed Up and Go (TUG) test results; quadriceps strength; and incidence of complications, including postoperative nausea and vomiting, DVT, catheter-related infections, catheter dislodgement and neurologic deficits, showed no significant difference between the two ACB methods.
Conclusion:
The results of this study demonstrate that CACB is an effective alternative to SACB and can provide better pain relief, a shorter LOH, more degrees of maximum flexion and a lower amount of opioid consumption over time, but it provides a comparable level of recovery of quadriceps strength and mobility with a similar risk of catheter-related complications. Thus, CACB may be a better analgesia strategy than SACB after TKA at present.
1. Introduction
While the femoral nerve block (FNB) has traditionally been the gold standard for analgesia following TKA, the adductor canal block (ACB), which is almost a pure sensory nerve block, has emerged as an alternative to the FNB after total knee arthroplasty (TKA).[1,2,3] Compared with the FNB, the ACB provides at least equal if not superior analgesia and is better at sparing the motor nerve supply to most of the quadriceps muscle, thereby allowing early mobilization and decreasing the risk for falls.[2,4,5] Therefore, increasingly more individuals agree that the ACB should be integrated into a multimodal pain protocol to improve pain management after TKA. However, the optimal duration to maintain the ACB is unknown. Both the single-shot adductor canal block (SS-ACB) and continuous catheter ACB (CACB), which maintains the infusion for 24 or 48 h after surgery, have been shown to provide excellent postoperative analgesia and to improve postoperative knee rehabilitation in TKA patients.[6,7,8,9] However, there is no consensus regarding which way is more effective in relieving pain after TKA. Some people think a continuous blockade of the adductor canal via a catheter is a more logical choice since the average duration of severe pain after TKA spans 2 to 3 days.[10] However, other people have drawn different conclusions; they have reported that a similar analgesia effect can be achieved with the single-shot ACB when the duration of the single-shot block is extended over 12 h. Moreover, the continuous catheters may be technically challenging to insert, require additional expertise to both place and manage, and have a high risk of inherent foreign body bacterial colonization (53%)[11] and premature dislodgement before the end of the analgesia process. Another argument against continuous infusion is that longer blocks may lead to quadriceps weakness and an increased risk of falls after TKA.[12,13] Therefore, we performed a meta-analysis to evaluate the evidence from all of the highest-level evidence-based (level I) studies that compared the SACB with CACB for patients undergoing primary TKA.
The outcomes included
-
1.
the visual analog scale (VAS) pain score/NRS score at rest and mobilization at 12, 24, and 48 h;
-
2.
amount of opioid consumption at 24, 48, and 72 h;
-
3.
rates of complications, including postoperative nausea and vomiting (PONV), deep venous thrombosis (DVT), catheter-related infections, catheter dislodgement and neurologic deficits; and
-
4.
other outcomes including quadriceps strength, ambulation ability, range of motion (ROM), and length of hospital stay (LOH) to assess the efficiency and safety of SACB and CACB in patients undergoing TKA.
Furthermore, we also proposed recommendations for clinicians using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system.
2. Methods
2.1. Search strategy
Our systematic review and meta-analysis has been reported in line with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)[14] and AMSTAR (Assessing the methodological quality of systematic reviews) Guidelines. The systematic review and meta-analysis were prospectively registered on PROSPERO (International Prospective Register of Systematic Reviews), and the registration number was CRD42019130766. The GRADE system[15] and Cochrane Handbook[16] were used to assess the quality of the results published in all included studies to ensure that the results of our meta-analysis were reliable and valid. We identified randomized controlled trials up to December 2019 by searching databases, including the Web of Science, Embase, PubMed, Cochrane Controlled Trials Register, Cochrane Library, CBM, CNKI, VIP, and Wanfang databases, using the following terms: (TKA or total knee replacement) AND (single ACB) AND (CACB). A flow chart of the trial selection process is presented in Figure 1
Figure 1.
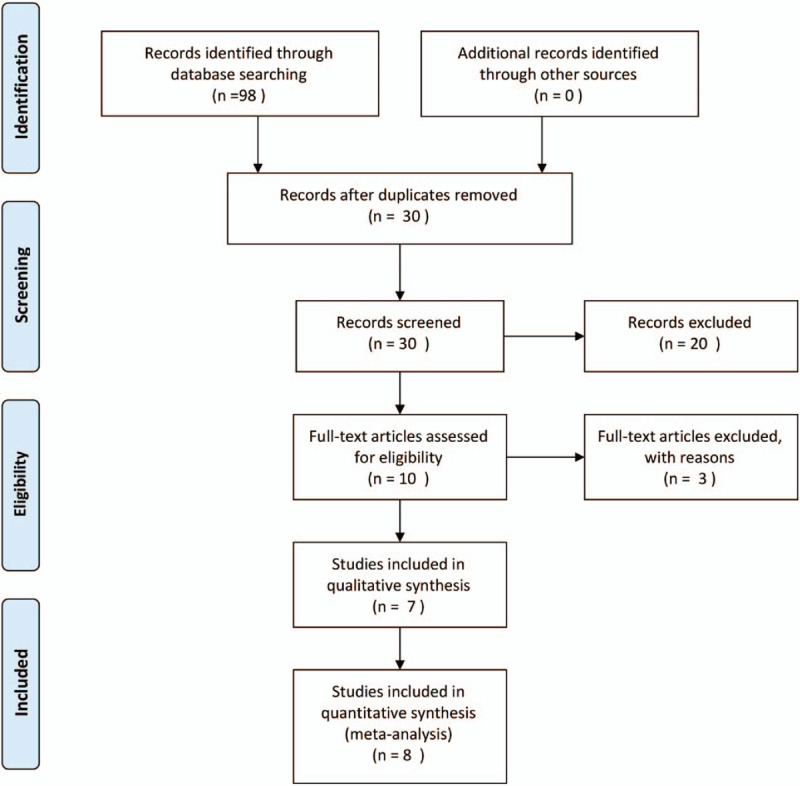
The search results and selection procedure.
2.2. Inclusion criteria
RCTs were included in our meta-analysis if they met the following PICOS (patients, intervention, comparator, outcome, and study design) criteria:
-
1.
Patients: patients had received primary TKA.
-
2.
Intervention: Patients received a single-shot ACB for TKA.
-
3.
Comparator: Patients received a CACB for TKA.
-
4.
Outcomes: The primary outcomes included the following: VAS/NRS pain score[17] at rest and mobilization at 12, 24, and 48 h; amount of opioid consumption (all opioids given were converted to morphine equivalents) at 24, 48 and 72 h; rates of complications, including PONV, DVT, catheter-related infections, catheter dislodgement and neurologic deficits. Secondary outcomes included the following: quadriceps muscle strength, TUG test,[18] LOH, and degrees of maximum flexion.
-
5.
Study design: RCTs.
We only included published clinical studies; the included studies were required to have reported at least one outcome.
The exclusion criteria included observational studies, non-RCTs, review articles, and studies with insufficient outcome data.
2.3. Data extraction
Two authors independently reviewed all titles and abstracts of studies identified by the above searches. Full texts of any potentially useful studies were reviewed, and disagreements were resolved by discussion. We extracted the following data from the included articles: authors, publication date, number of patients in each group, demographic data of the participants including age, sex, dosages, and kinds of anesthesia drug administered.
2.4. Risk of bias and quality assessment
Two authors independently assessed the risk of bias of the included studies. According to the Cochrane Handbook for Systematic Reviews of Interventions, we assessed the methodological quality and basis of the included literature as follows: randomization, allocation concealment, blinding method, selective reporting, group similarity at baseline, incomplete outcome data, compliance, timing of outcome assessments, and intention-to-treat analysis (Figs. 2 and 3). Disagreements were resolved by the third author. The quality of evidence of the outcomes was judged according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria. Two authors independently evaluated five factors (risk of bias, inconsistency, indirectness, imprecision, and publication bias) that may decrease the quality level of the evidence. The recommendation level of evidence was classified into four categories: high, moderate, low, or very low. The results of the GRADE analysis are presented in supplemental Figure 1.
Figure 2.
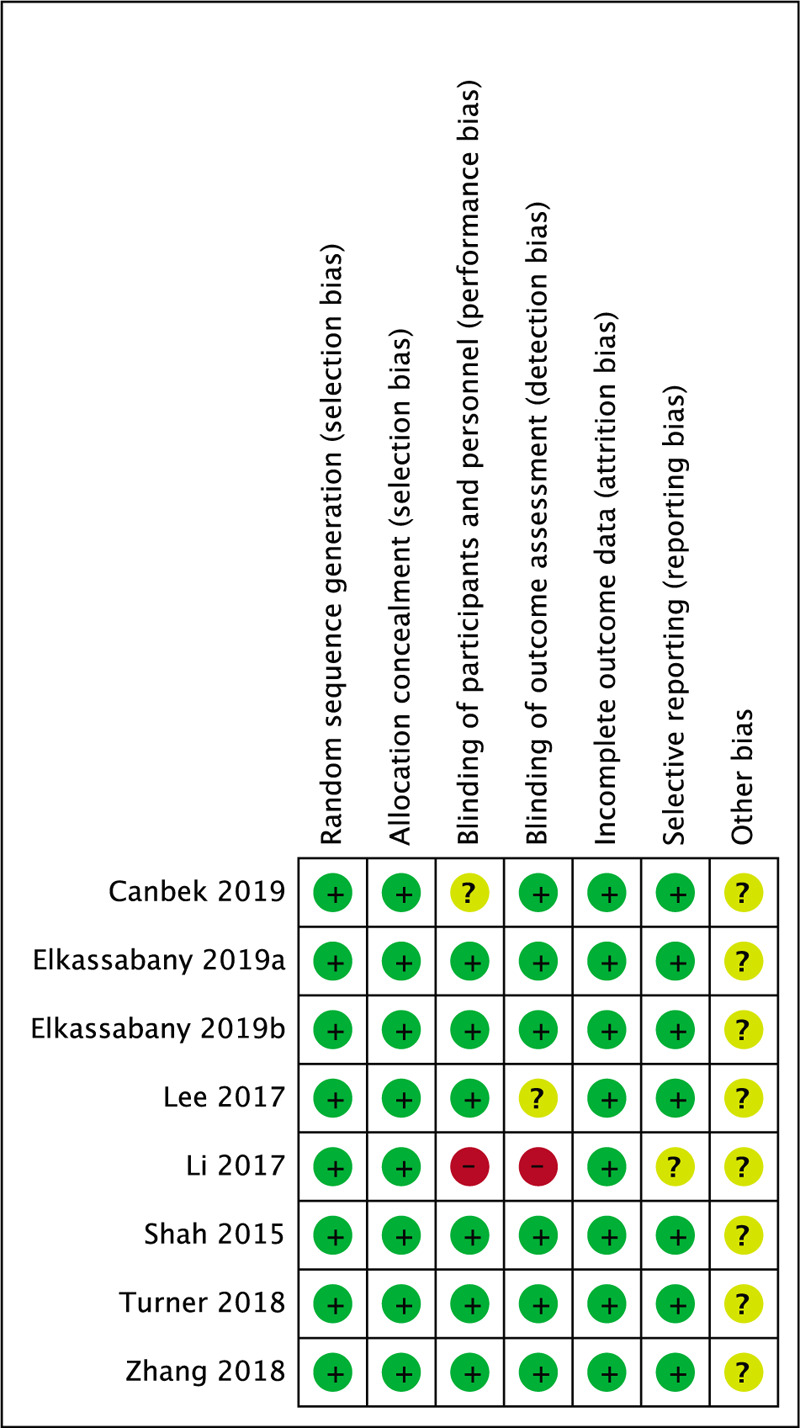
The risk of bias graph of the included studies.
Figure 3.
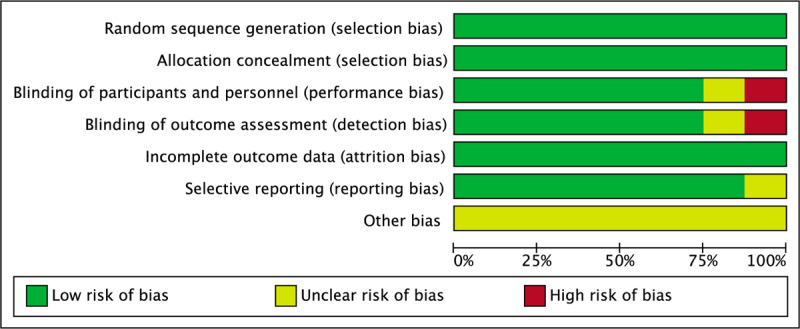
The risk of bias summary: review authors’ judgment of each risk of bias items for each included studies.
2.5. Dealing with missing data
For reports with incomplete and missing data, we attempted to contact the author of the original reports to obtain additional details and any missing data. All the data are presented as the mean ± standard deviation (SD) in our meta-analysis. If the data were reported as the median and interquartile range, we assumed that the median was equivalent to the mean and that the width of the interquartile range was equivalent to 1.35 times the SD. In the study of Hozo et al,[19] the median can be used to estimate the mean when the sample size is larger than 25. When the sample sizes were moderate (15 < n ≤ 70), the formula range/4 was the best estimator for the standard deviation. When the sample sizes were large (n > 70), the formula range/6 was the best estimator for the standard deviation. When the data were reported in a graph, means ± SDs were estimated by Get Data software (version 2.22, GetData Graph Digitizer, 2013). All the methods above were used to calculate the means ± SDs based on the Cochrane Handbook for Systematic Reviews.
2.6. Statistical analysis and data synthesis
Meta-analyses were performed with Review Manager Software for MAC. The mean difference (MD) or standard MD was used to assess the continuous outcomes, such as the VAS score, amount of opioid consumption, quadriceps muscle strength, TUG test results, LOH and degrees of maximum flexion, with a 95% confidence interval (CI). Relative risks with a 95% CI were used to assess the dichotomous outcomes, such as the incidence of complications, including PONV, DVT, catheter-related infections, catheter dislodgement, and neurologic deficits. We used the I2 statistic to estimate the heterogeneity among the studies, and substantial heterogeneity was represented by an I2 value >50%. A fixed effects model was used if the heterogeneity test did not reveal statistical significance (I2 < 50%, P > .1). Otherwise, we adopted a random effects model. The inverse variance and Mantel–Haenszel methods were used to combine separate statistics. P < .05 was considered to be statistically significant.
3. Results
3.1. Excluded studies and search results
Initially, we identified a total of 98 citations from electronic journal databases, 88 of which were removed by duplicate and primary screening according to the titles and abstracts. After reading the full texts of the 10 remaining studies in detail, we excluded three studies that did not meet the inclusion criteria. Seven articles were assessed for eligibility. In one article, Elkassabany et al[20] reported outcomes such as pain scores, opioid requirements, and LOH. In their study, there were two subgroups comparing single-injection ACB with CACB. In group B, the continuous catheter group corresponded to the 24-h infusion group. In group C, the continuous catheter group corresponded to the 48-h infusion group, so we divided the study into two groups, Elkassabany (2019a) and Elkassabany (2019b). Finally, we included 8 RCTs[20,21,22,23,24,25,26] with 702 knees that compared SACB with CACB in our meta-analysis. The detailed baseline characteristics and general intervention information of the 8RCTs are presented in Tables 1 and 2. All articles were published in English and Chinese between 2015 and December 2019.
Table 1.
The detailed baseline characteristics of included studies.

Table 2.
The general intervention information of included studies.

3.2. Results of the meta-analysis
3.2.1. Primary outcomes
3.2.1.1. VAS/NRS score at rest
Since the VAS and the NRS are two similar pain scoring systems, we combined the scores of these systems into one outcome for analysis. Five studies assessing 444 knees reported VAS scores within 12 h postoperatively. The data showed that there was no significant difference between the two groups (MD = 0.62; 95% CI, −0.19 to 1.43; P = .13; Fig. 4). Six studies assessing 493 knees reported VAS scores within 24 h postoperatively. The pooled data showed that compared with the SACB, the CACB had a better pain control effect at rest, with significant differences at 24 h (MD = 0.52; 95% CI, 0.07–0.96; P = .02; Fig. 4). Eight studies involving 702 knees reported the VAS score at 48 h. The meta-analysis showed that the CACB group had a better pain control effect at rest within 48 h, with significant differences between the CACB and SACB groups (MD = 0.62; 95% CI, 0.18–1.05; P = .006; Fig. 4).
Figure 4.
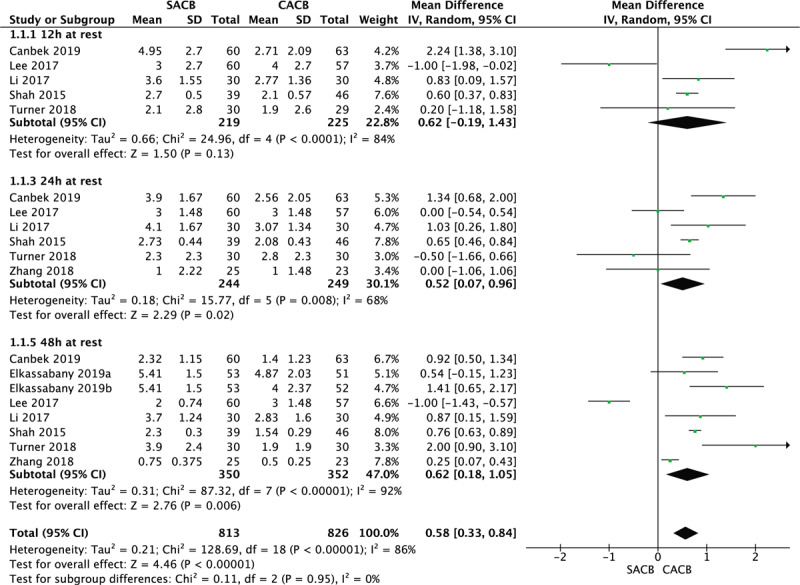
A funnel plot of VAS/NRS score within 48 h at rest. CACB = continuous catheter adductor canal block, CI = confidence interval, NRS = numerical rating scale, SACB = single-shot adductor canal block, VAS = visual analog scale.
3.2.1.2. VAS/NRS score at mobilization
Two studies assessing 119 knees reported VAS scores within 12 h with mobilization postoperatively. The results revealed a better pain control effect with mobilization in the CACB group than in the SACB group at 12 h (MD = 1.10; 95% CI, 0.45–1.75; P = .0009; Fig. 5). There were five studies involving a total of 376 knees that evaluated the VAS score with mobilization at 24 and 48 h postoperatively. The results of the meta-analysis revealed a better pain control effect with mobilization in the CACB group than in the SACB group at 24 h (MD = 1.01; 95% CI, 0.84–1.18; P < .00001; Fig. 5) and 48 h (MD = 0.87; 95% CI, 0.72–1.01; P < .00001; Fig. 5) postoperatively.
Figure 5.
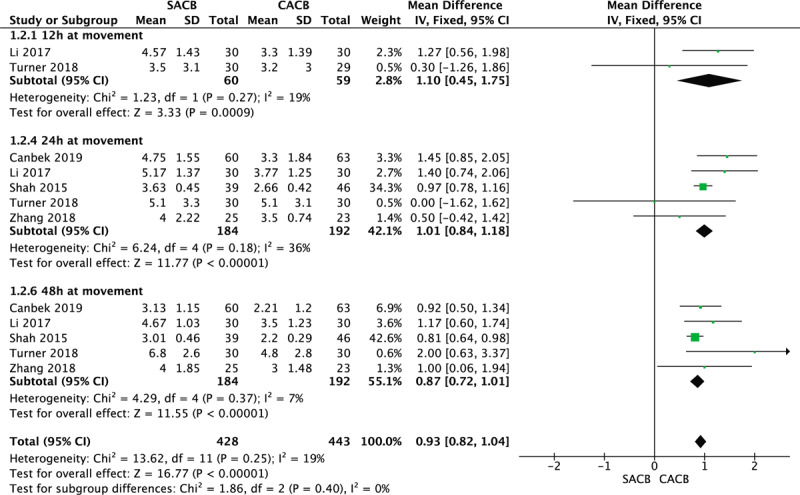
A funnel plot of VAS/NRS score within 48 h at mobilization. CACB = continuous catheter adductor canal block, CI = confidence interval, NRS = numerical rating scale, SACB = single-shot adductor canal block,VAS = visual analog scale.
3.2.1.3. Morphine consumption
Conversions of amounts of different opioids used were performed using a web-based opioid conversion calculator (http://www.globalrph.com/narcoticonv.htm). Morphine consumption at 24 h was reported in 6 RCTs involving a total of 557 knees in 3 of the included studies. The pooled data showed no significant difference between the two groups (MD = 17.35; 95% CI, −12.52 to 47.22; P = .25; Fig. 6). Morphine consumption at 48 h was conducted in 6 studies involving a total of 494 knees. The pooled data showed no significant difference between the two groups (MD = 31.81; 95% CI, −8.80 to 72.42; P = .12; Fig. 6). Morphine consumption at 72 h was conducted in 2 studies involving a total of 108 knees. The pooled data showed more morphine consumption in the SACB group than in the CACB group, with a significant difference between the two groups (MD = 109.34; 95% CI, 26.70–191.99; P = .01; Fig. 6).
Figure 6.
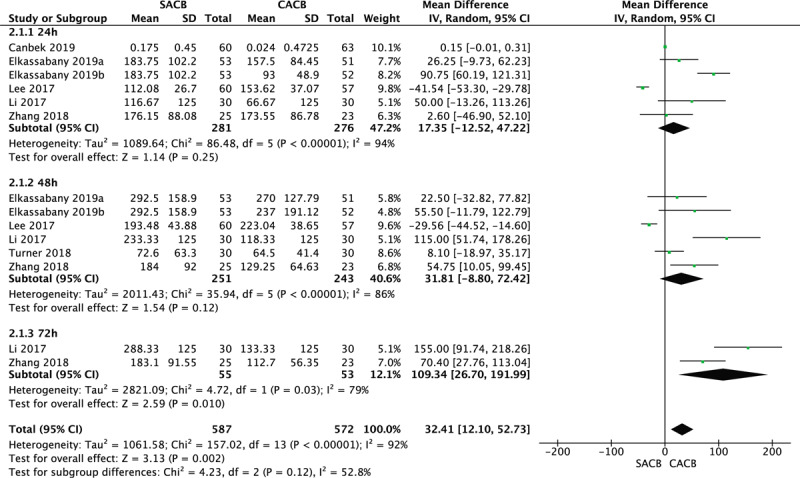
A funnel plot of Morphine consumption within 72 h at mobilization. CACB = continuous catheter adductor canal block, CI = confidence interval, SACB = single-shot adductor canal block.
3.2.1.4. Complications
The incidence of nausea and vomiting was reported in 4 studies involving a total of 253 knees. The pooled data showed no significant differences between the two groups (MD = −0.04; 95% CI, −0.12 to 0.04; P = 0.30; Fig. 7). Three studies assessing 262 knees reported catheter site infections, neurologic deficits, and DVT. The results showed no significant differences between the two groups in terms of catheter site infections (MD = 0.00; 95% CI, −0.03 to 0.03; P = 1.00; Fig. 7), neurologic deficits (MD = 0.00; 95% CI, −0.03 to 0.03; P = 1.00; Fig. 7) and DVT (MD = 0.00; 95% CI, −0.03 to 0.03; P = 1.00; Fig. 7). Two studies assessing 145 knees reported catheter dislodgement. The pooled data showed no significant differences between the two groups (MD = 0; 95% CI, −0.04 to 0.04; P = 1.00; Fig. 7).
Figure 7.
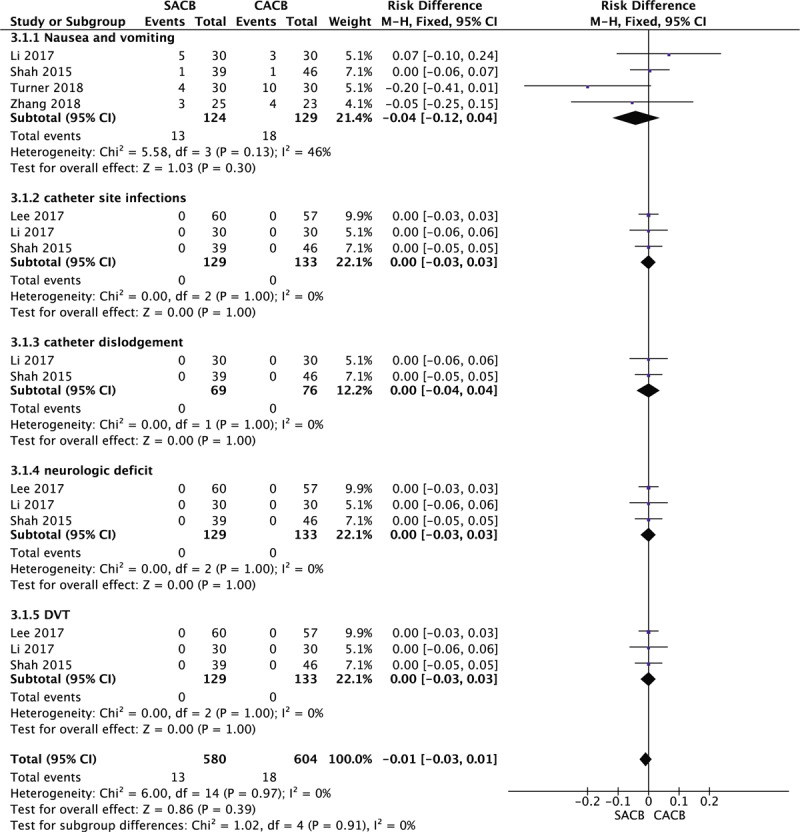
A funnel plot of complications. CACB = continuous catheter adductor canal block, CI = confidence interval, DVT = deep venous thrombosis, SACB = single-shot adductor canal block.
3.2.2. Secondary outcomes
3.2.2.1. Quadriceps muscle strength (manual muscle test)
Two studies involving 108 knees reported quadriceps muscle strength as measured by the manual muscle test at 24, 48, and 72 h. The pooled data showed no significant differences at 24 h (MD = 0.32; 95% CI, −0.99 to 1.63; P = .63; Fig. 8), at 48 h (MD = −0.03; 95% CI, −0.78 to 0.83; P = .94; Fig. 8) and 72 h (MD = −0.20; 95% CI, −0.48 to 0.09; P = .17; Fig. 8).
Figure 8.
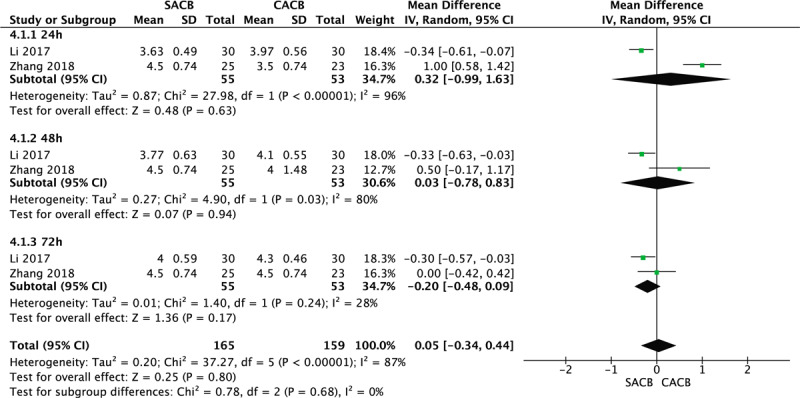
A funnel plot of Quadriceps Muscle Strength. CACB = continuous catheter adductor canal block, CI = confidence interval, MMT = manual muscle test, SACB = single-shot adductor canal block.
3.2.2.2. TUG test
The TUG test at 24 h was conducted in 4 RCTs involving a total of 417 knees to evaluate mobility. There were no significant differences between the single-injection ACB and CACB groups (MD = 0.41; 95% CI, −1.54 to 2.36; P = .68; Fig. 9).
Figure 9.
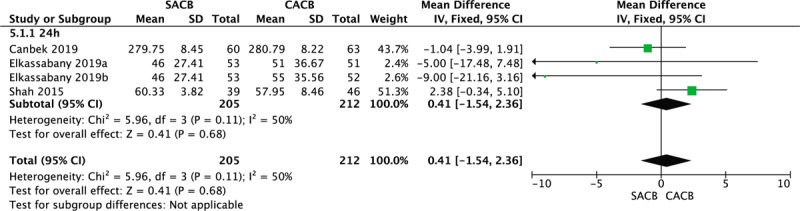
A funnel plot of TUG test. CACB = continuous catheter adductor canal block, CI = confidence interval, SACB = single-shot adductor canal block, TUG = test, timed up and go test.
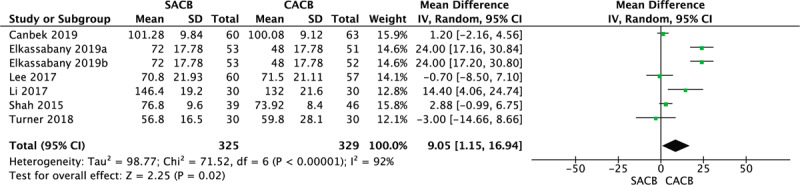
3.2.2.3. LOH
Seven RCTs with 654 patients reported the LOH. Compared with the SACB group, a shorter LOH was found in the CACB group, with significant differences in our meta-analysis (MD = 9.05; 95% CI, −1.15 to 16.94; P = .02; Fig. 10).
Figure 10.
A funnel plot of length of hospital stay. CACB = continuous catheter adductor canal block, CI = confidence interval, SACB = single-shot adductor canal block.
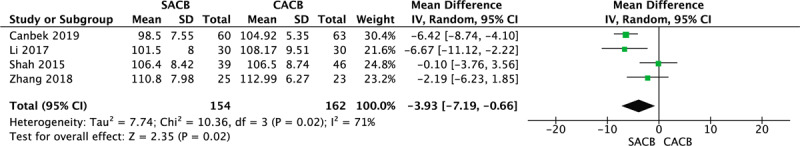
3.2.2.4. Degrees of maximum flexion
Degrees of maximum flexion were reported in 4 of the included studies, and a total of 316 knees were involved in the meta-analysis. There were fewer degrees of maximum flexion in the SACB group than in the CACB group, with significant differences between the two groups (MD = −3.93; 95% CI, −7.19 to −0.66; P = .02; Fig. 11).
Figure 11.
A funnel plot of degrees of maximum flexion. CACB = continuous catheter adductor canal block, CI = confidence interval, SACB ‘= single-shot adductor canal block.
4. Discussion
The ACB is an optimal method for achieving analgesia after TKA with minimal quadriceps weakness.[1,2,3] However, the ideal local anesthetic regimen, either continuous or single shot ACB administration, has yet to be determined. To date, only two meta-analysis were recently published on this topic.[27,28] In Zhang's meta-analysis, only four RCTs were included in the meta-analysis, and there was considerable heterogeneity in some results between the two groups. Second, they only analyzed opioid consumption within 48 h after surgery. Data collected at 48 h only may not reflect the advantages of the CACB in efficient opioid use. In both Zhang and Wang's meta-analysis they do not analyze postoperative quadriceps muscle strength and walking ability which are critical for rapid recovery. Doctors’ concerns about the CACB included the risk of catheter-related infections, catheter dislodgement, and neurologic deficits. The previous two meta-analyses did not analyze these complications that doctors were concerned about. Therefore, we performed a meta-analysis to evaluate the evidence from all the available RCTs that compared the SACB with CACB for patients undergoing primary TKA. We believe that our meta-analysis will provide a more definite conclusion about which ACB method is better for TKA patients because we included the highest-level evidence-based (level I) studies. Moreover, our results included opioid consumption at 72 h; complications including catheter-related infections, catheter dislodgement and neurologic deficits; quadriceps strength; and ambulation ability, which may be essential supplements to the previous meta-analysis. Furthermore, we propose recommendations for clinicians using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system, which make our results more convincing.
The VAS score, opioid consumption, and complications were the primary outcomes assessed in our meta-analysis. Previous studies have suggested that movement (dynamic) pain is more important to consider than pain at rest.[29] Therefore, we assessed not only the pain score at rest but also the dynamic VAS pain scores. A recently published meta-analysis demonstrated that SACB groups present VAS scores at 24 h at rest and during movement after TKA that are similar to those of CACB groups, but the CACB groups had lower VAS scores at 48 h at rest and during movement than did the corresponding SACB groups. However, according to our meta-analysis, the VAS score evaluating postoperative pain showed better results and statistically significant differences at 24 and 48 h at rest and mobilization in the CACB group than in the SACB group. Both meta-analyses showed better pain control effects at 48 h in the CACB group than in the SACB group. Our findings may be intuitively explained by the fact that continuous infusion catheter blocks permit adequate analgesia of the local anesthetic for a longer period of time than single-shot technique does. In our included studies, the heterogeneity test showed a statistically significance difference in the VAS score at rest. Thus, a random effects model was performed to evaluate the results. The heterogeneity may be caused by several reasons: first, the different races of the patients. One trial was conducted in Asia, and the other trials were conducted in Europe or America. Second, the mean age was different in the included articles. Third, for some of the studies, we needed to estimate the mean and variance from the median, range, and size of a sample (range = maximum–minimum). However, the evidence regarding the VAS score at rest and during movement was of moderate quality. Furthermore, all the included studies were RCTs of high quality. Therefore, the overall quality of evidence and effect estimate regarding the VAS score at rest and upon ambulation was reliable.
In our meta-analysis, we found no difference in the quantity of opioids used within the 24- and 48-h time periods between the two groups. This finding is comparable to the findings of a recent meta-analysis by Zhang. However, Zhang did not have any data on morphine consumption at 72 h postoperatively. Concerning the 72 h time period, our results showed significantly lower opioid consumption in the CACB group than in the SACB group. There was a high level of heterogeneity between the two groups. However, the quality of evidence was high according to the GRADE system, and we could confidently conclude this result. Our results indicate that over time, the analgesic effect experienced by the SACB group gradually decreased with the decrease in the local anesthetic drug concentration, while the CACB group continued to receive local anesthetic drugs after retaining the catheter. Therefore, the catheter group demonstrated an opioid-sparing effect as the initial bolus wore off.
Regarding the complications, an ideal method of achieving analgesia is to relieve pain without increasing the number of complications. PONV are common opioid consumption-associated side effects. Our meta-analysis shows that the incidence of PONV was low without a significant difference between SACB and CACB. Moreover, we found no significant difference in DVT between the two groups. These results were comparable to the findings of a recent meta-analysis by Zhang. However, Zhang's meta-analysis only evaluated PONV and DVT. Doctors’ concerns about CACB are related to the risk of catheter-related infections, catheter dislodgement and neurologic deficits. Therefore, we also evaluated these complications. Our results showed that no significant difference was found in terms of catheter-related infections, catheter dislodgement and neurologic deficits. The quality of evidence was high according to the GRADE system; therefore, the overall quality of evidence and effect estimate regarding complications was reliable.
Quadriceps strength, the TUG test results, ROM, and LOH were the secondary outcomes assessed in our meta-analysis, and they had a direct impact on the speed of postoperative recovery of the TKA patients. Quadriceps strength can improve physical therapy outcomes for TKA patients, which is vital to relieving pain in TKA patients. Muscle strength was measured using manual muscle testing, and our meta-analysis failed to find any significant difference between the SACB and CACB groups regarding quadriceps muscle strength at 24, 48, and 72 h. The quality of evidence was moderate at 24 h and high at 48 and 72 h according to the GRADE system, and we could confidently draw conclusions about this result.
Ambulation ability was assessed by the TUG test. The results of our meta-analysis showed similar results of the TUG tests at 24 h in both the SACB and CACB groups, with no statistical significance. The quality of evidence was high according to the GRADE system.
The LOH represented the economic expenditure of each patient. ROM was used to measure early mobilization, which can facilitate functional recovery and reduce postoperative complications and LOH. Our meta-analysis showed that compared with the SACB group, the CACB group had a shorter LOH and larger ROM, with a significant difference. LOH and ROM were affected by multiple factors, including age, body mass index, physiological status and American Society of Anesthesiologists status,[30] and there was large heterogeneity between the SACB and CACB groups. However, the quality of evidence was high according to the GRADE system, and the conclusion about this result was reliable. Our results are different from Zhang's result. In Zhang's meta-analysis, no significant differences were found between the two groups in terms of LOH and ROM. We think the reason for this discrepancy is that Zhang's meta-analysis included too few RCTs.
In clinical practice, the time for postoperative CACB placement did not significantly add to the total time of the primary surgical procedure.[26,30] Additionally, it is not necessary for surgeons to worry about the risk of dislodgement with vigorous movements of the leg during operation, catheter blockages in the surgical field, and tourniquet use over the block when performing CACB after the operation.[6,31,32] There are several reported side effects, especially when performing continuous nerve blocks, such as catheter site infections, prolonged nerve palsies, heel ulcers, and other catheter-related problems due to the sensory block.[11,33,34] However, in our meta-analysis, there were no side effects in either group. We believe with the development of ultrasonography, identification of the adductor canal is relatively easy, and we can achieve a high success rate when performing ultrasound-guided ACB.[6,7,26]
Our systematic review and meta-analysis have the following limitations.
-
1.
Only 8 RCTs and 702 knees were included in our meta-analysis; if more RCTs had been included, the statistical power of our analysis would have been higher.
-
2.
We evaluated only the immediate effects within 72 h after TKA; we do not know the duration of the effects or whether these effects lead to better long-term functional outcomes. Therefore, a long-term follow-up study is needed to investigate long-term functional outcomes.
-
3.
Heterogeneity among the included studies was unavoidable due to a variety of factors, such as age, sex, racial differences, tourniquet use, type of catheter and analgesia methods.
-
4.
Some other minor factors, such as differences in the technique, time of the block, doses of the different drugs administered, amount and techniques of the assessments, may affect the quality of results and produce some bias.
Although this study has several limitations, it is the first meta-analysis to evaluate opioid consumption at 72 h, quadriceps strength, ambulation ability, and complications including catheter-related infections, catheter dislodgement and neurologic deficits related to SACB versus CACB in TKA patients. Furthermore, it is a comprehensive review of Level-I evidence on this topic with articles that were stringently screened before being included. Therefore, the review is of high quality (that is, the studies were all prospective randomized trials). Finally, the PRISMA guidelines and the Cochrane Handbook GRADE approach were applied to assess the quality of the results and evidence published in all included studies.
5. Conclusion
Based on this meta-analysis of all previously published RCTs, we found CACB can provide better pain relief, a shorter LOH, more degrees of maximum flexion and lower opioid consumption over time, furthermore, it provides a comparable level of recovery of quadriceps strength and mobility and a similar risk of catheter-related complications. Therefore, for a fast recovery after TKA, CACB is recommended as an alternative analgesic method after TKA at present. However, due to the variations among the included studies, more large-sample and high-quality RCTs are needed in the future to demonstrate the efficacy and safety of CACB compared with SACB after TKA.
Author contributions
Guarantor of integrity of entire study: Xu Cai.
Study concepts: Changjiao Sun.
Study design: Changjiao Sun.
Literature research: Changjiao Sun, Fei Song.
Data acquisition: Changjiao Sun, Zhe Zhao, Ruiyong Du, Sha Wu, Qi Ma.
Data analysis/interpretation: Changjiao Sun, Xiaofei Zhang.
Statistical analysis: Changjiao Sun, Xiaofei Zhang.
Manuscript preparation: Changjiao Sun.
Manuscript definition of intellectual content: Changjiao Sun.
Manuscript editing: Changjiao Sun.
Manuscript revision/review: Changjiao Sun, Xiaofei Zhang, Xu Cai.
Manuscript final version approval: Xu Cai.
Supplementary Material
Footnotes
Abbreviations: ACB = adductor canal block, CACB = continuous catheter adductor canal block, CIs = Confidence intervals, FNB = femoral nerve block, GRADE = Grading of Recommendations, Assessment, Development, and Evaluation, OR = odds ratio, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-analyses, RCTs = randomized controlled trials, RD = risk difference, RR = risk ratio, SACB = single-shot adductor canal block, THA = total hip arthroplasty, TJA = total joint arthroplasty, TKA = total knee arthroplasty, WMD = weighted mean difference.
How to cite this article: Sun C, Zhang X, Song F, Zhao Z, Du R, Wu S, Ma Q, Cai X. Is continuous catheter adductor canal block better than single-shot canal adductor canal block in primary total knee arthroplasty? A GRADE Analysis of the Evidence Through a Systematic Review and Meta-Analysis. Medicine. 2020;99:20(e20320).
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Availability of data and materials: The datasets generated and analyzed during the present study are available from the corresponding author on reasonable request.
The authors have no funding information to disclose.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
The datasets generated during and/or analyzed during the present study are publicly available.
References
- [1].Gao F, Ma J, Sun W, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a systematic review and meta-analysis. Clin J Pain 2017;33:356–68. [DOI] [PubMed] [Google Scholar]
- [2].Jæger P, Zaric D, Fomsgaard JS, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: a randomized, double-blind study. Reg Anesth Pain Med 2013;38:526–32. [DOI] [PubMed] [Google Scholar]
- [3].Hanson NA, Allen CJ, Hostetter LS, et al. Continuous ultrasound-guided adductor canal block for total knee arthroplasty: a randomized, double-blind trial. Anesth Analg 2014;118:1370–7. [DOI] [PubMed] [Google Scholar]
- [4].Li D, Yang Z, Xie X, et al. Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: a systematic review and meta-analysis. Int Orthop 2016;40:925–33. [DOI] [PubMed] [Google Scholar]
- [5].Zhao XQ, Jiang N, Yuan FF, et al. The comparison of adductor canal block with femoral nerve block following total knee arthroplasty: a systematic review with meta-analysis. J Anesth 2016;30:745–54. [DOI] [PubMed] [Google Scholar]
- [6].Jaeger P, Grevstad U, Henningsen MH, et al. Effect of adductor-canal-blockade on established, severe post-operative pain after total knee arthroplasty: a randomised study. Acta Anaesthesiol Scand 2012;56:1013–9. [DOI] [PubMed] [Google Scholar]
- [7].Manickam B, Perlas A, Duggan E, et al. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med 2009;34:578–80. [DOI] [PubMed] [Google Scholar]
- [8].Jenstrup MT, Jæger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand 2012;56:357–64. [DOI] [PubMed] [Google Scholar]
- [9].Gwam CU, Mistry JB, Khlopas A, et al. Does addition of multimodal periarticular analgesia to adductor canal block improve lengths of stay, pain, discharge status, and opioid use after total knee arthroplasty? J Arthroplasty 2017;32:1470–3. [DOI] [PubMed] [Google Scholar]
- [10].Andersen LØ, Gaarn-Larsen L, Kristensen BB, et al. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia 2009;64:508–13. [DOI] [PubMed] [Google Scholar]
- [11].Cuvillon P, Ripart J, Lalourcey L, et al. The continuous femoral nerve block catheter for postoperative analgesia: bacterial colonization, infectious rate and adverse effects. Anesth Analg 2001;93:1045–9. [DOI] [PubMed] [Google Scholar]
- [12].Johnson RL, Kopp SL, Hebl JR, et al. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth 2013;110:518–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ilfeld BM, Duke KB, Donohue MC. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth Analg 2010;111:1552–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336e41. [DOI] [PubMed] [Google Scholar]
- [15].Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ (Clin Res Ed) 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Higgins J. Cochrane handbook for systematic reviews of interventions version 5.0.1. Cochrane Datab Syst Rev 2011;2011. [Google Scholar]
- [17].Chapman CR, Casey KL, Dubner R, et al. Pain measurement: an overview. Pain 1985;22:1e31. [DOI] [PubMed] [Google Scholar]
- [18].Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther 2000;80:896e903. [PubMed] [Google Scholar]
- [19].Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Elkassabany NM, Cai LF, Badiola I, et al. A prospective randomized open-label study of single injection versus continuous adductor canal block for postoperative analgesia after total knee arthroplasty. Bone Joint J 2019;101-B:340–7. [DOI] [PubMed] [Google Scholar]
- [21].Canbek U, Akgun U, Aydogan NH, et al. Continuous adductor canal block following total knee arthroplasty provides a better analgesia compared to single shot: a prospective randomized controlled trial. Acta Orthop Traumatol Turc 2019;53:334–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Turner JD, Dobson SW, Henshaw DS, et al. Single-injection adductor canal block with multiple adjuvants provides equivalent analgesia when compared with continuous adductor canal blockade for primary total knee arthroplasty: a double-blinded, randomized, controlled, equivalency trial. J Arthroplasty 2018;33:3160–6.e1. [DOI] [PubMed] [Google Scholar]
- [23].Zhang Y, Tan Z, Liao R, et al. The prolonged analgesic efficacy of an ultrasound-guided single-shot adductor canal block in patients undergoing total knee arthroplasty. Orthopedics 2018;41:e607–14. [DOI] [PubMed] [Google Scholar]
- [24].Lee S, Rooban N, Vaghadia H, et al. A randomized non-inferiority trial of adductor canal block for analgesia after total knee arthroplasty: single injection versus catheter technique. J Arthroplasty 2018;33:1045–51. [DOI] [PubMed] [Google Scholar]
- [25].Li C, Xu H, Shen B, et al. Effect of continuous and single shot adductor canal blocks for postoperative analgesia and early rehabilitation after total knee arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2017;31:1049–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shah NA, Jain NP, Panchal KA. Adductor canal blockade following total knee arthroplasty-continuous or single shot technique? Role in postoperative analgesia, ambulation ability and early functional recovery: a randomized controlled trial. J Arthroplasty 2015;30:1476–81. [DOI] [PubMed] [Google Scholar]
- [27].Zhang LK, Zhang BY, Quan RF, et al. Single shot versus continuous technique adductor canal block for analgesia following total knee arthroplasty: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 2019;98:e15539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Wang C, Chen Z, Ma X. Continuous adductor canal block is a better choice compared to single shot after primary total knee arthroplasty: a meta-analysis of randomized controlled trials. Int J Surg 2019;72:16–24. [DOI] [PubMed] [Google Scholar]
- [29].Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth 2008;101:17–24. [DOI] [PubMed] [Google Scholar]
- [30].Shah NA, Jain NP. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: a randomized controlled trial. J Arthroplasty 2014;29:2224–9. [DOI] [PubMed] [Google Scholar]
- [31].Lund J1, Jenstrup MT, Jaeger P, et al. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand 2011;55:14–9. [DOI] [PubMed] [Google Scholar]
- [32].Andersen HL, Gyrn J, Møller L, et al. Continuous saphenous nerve block as supplement to single-dose local infiltration analgesia for postoperative pain management after total knee arthroplasty. Reg Anesth Pain Med 2013;38:106–11. [DOI] [PubMed] [Google Scholar]
- [33].Salinas FV, Liu SS, Mulroy MF. The effect of single-injection femoral nerve block versus continuous femoral nerve block after total knee arthroplasty on hospital length of stay and long-term functional recovery within an established clinical pathway. Anesth Analg 2006;102:1234. [DOI] [PubMed] [Google Scholar]
- [34].Henningsen MH, Jaeger P, Hilsted KL, et al. Prevalence of saphenous nerve injury after adductor-canal-blockade in patients receiving total knee arthroplasty. Acta Anaesthesiol Scand 2013;57:1127. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


