Short abstract
Objective
To evaluate two osteoporosis screening tools, the osteoporosis self-assessment tool for Asians (OSTA) and the osteoporosis screening tool for Chinese (OSTC), in postmenopausal Chinese women with type 2 diabetes mellitus (T2DM).
Methods
This retrospective study enrolled postmenopausal female patients with T2DM. Bone mineral density at the lumbar spine (L1–4) and left femoral neck was measured using dual-energy X-ray absorptiometry (DXA). The OSTA and OSTC scores were calculated and compared with bone mineral density at the two anatomical sites.
Results
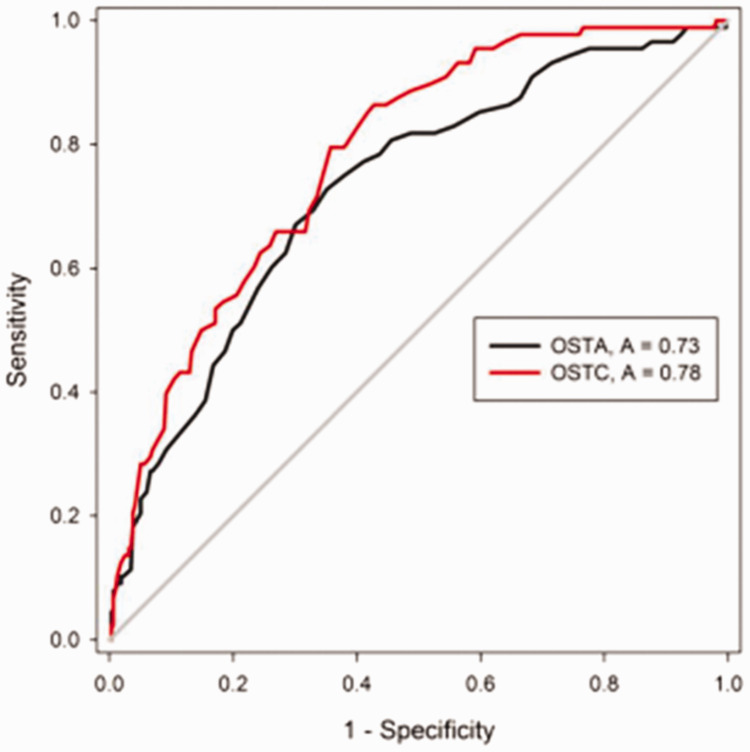
A total of 404 patients with T2DM were enrolled in this study. The detection rates for osteoporosis in the lumbar spine (L1–L4) and left femoral neck by DXA were 22.5% (91 of 404 patients) and 21.8% (88 of 404 patients), respectively; 14.4% (58 of 404 patients) and 18.1% (73 of 404 patients) by OSTA, respectively; and 21.5% (87 of 404 patients) at both sites by OSTC. At the femoral neck, the areas under the curve (AUC) of OSTA and OSTC for predicting osteoporosis were 0.73 and 0.78, respectively. The sensitivity and specificity for OSTA were 64.9% and 72.7%, respectively; and for OSTC, they were 64.2% and 79.5%, respectively.
Conclusions
The OSTC assessment tool was superior to OSTA for osteoporosis screening in postmenopausal Chinese women with T2DM.
Keywords: Osteoporosis self-assessment tool for Asians, osteoporosis screening tool for Chinese, osteoporosis, type 2 diabetes mellitus, dual-energy X-ray absorptiometry
Introduction
Epidemiological research has demonstrated a growing number of people with type 2 diabetes mellitus (T2DM) around world.1,2 T2DM was recently demonstrated to be an important risk factor for osteoporosis-associated fracture, depending on the skeletal site and disease severity, which is one of the main causes of disability and death in elderly patients.3 Bone mineral density (BMD) as measured by dual-energy X-ray absorptiometry (DXA) is recognized as a standard method for identifying and confirming the presence of osteoporosis and predicting future fracture risk.4,5 However, the use of DXA machines is limited in primary hospitals in rural China. Therefore, an effective and simple screening method would enable patients at risk for osteoporosis to receive early diagnosis and treatment.
Over the past decade, researchers have attempted to develop easy and efficient assessment tools for the early screening of osteoporosis, but these have not been validated for the use in Asian populations.6,7 The osteoporosis self-assessment tool for Asians (OSTA), established using a multinational Asian cohort, was developed to identify patients with a high osteoporosis risk by considering body weight and age only.8,9 Studies demonstrated that OSTA could help to predict fracture risk among postmenopausal women.10–12 The osteoporosis screening tool for Chinese (OSTC) women, developed by Chinese researchers using body weight and age, was shown to effectively predict osteoporosis risk and to determine the appropriate use of BMD testing in community hospitals without sufficient DXA equipment.13 Considering that T2DM is associated with increased body weight,14 the OSTA and OSTC might estimate the fracture risk in patients with T2DM.
With the ever-increasing elderly population in China, physicians will need to treat a growing population of patients with T2DM at a higher risk of osteoporosis.15 However, DXA scans are not available to evaluate bone health at all healthcare centres in China because of the high cost and complicated methodology. Therefore, there is an urgent need to develop novel clinical strategies for discriminating those patients at high risk of fracture from the large number of patients with T2DM. This present analysis retrospectively investigated the BMD of postmenopausal women over 50 years old with T2DM in southern China and evaluated the use of the OSTA and OSTC scores compared with the DXA BMD findings in the diagnosis of osteoporosis.
Patients and methods
Patient population
This retrospective study enrolled consecutive postmenopausal female patients from the Department of Endocrinology and the Department of Orthopaedics, Affiliated Nanhai Hospital of Southern Medical University, Foshan, Guangdong Province, China between January 2015 and December 2017. The patients were diagnosed as having T2DM and had experienced a lumbar spine or intertrochanteric fracture caused by low-energy trauma. The menopause had lasted for at least 6 months. The clinicopathological parameters of all of the study participants were obtained from medical records and pathology reports. The diagnosis of T2DM was based on World Health Organization guidelines (1999).16,17 The diagnostic criteria for osteoporosis using BMD measurements were based on the Guidelines for Diagnosis and Treatment of Primary Osteoporosis of China.17 Patients with any illness that could affect bone metabolism, such as endocrine disorders, scoliosis, serious liver or kidney disease and others were excluded from the study. Patients were also excluded if they had a history of any spinal surgery or concomitant use of hormone drugs that could affect BMD measurement.
The Institutional Review Board of the Affiliated Nanhai Hospital approved the study (no. KY2018-129) and it was implemented in strict accordance with the ethical guidelines of the Declaration of Helsinki. All patients enrolled in this study provided written informed consent to the use of their clinical data for non-commercial scientific research.
Study methods
The BMD of the lumbar spine (L1–L4) and the left femoral neck were measured using DXA (Lunar Prodigy Advance; GE Medical Systems, Waukesha, WI, USA). The T-score value was used to express BMD as follows: T-score value ≤–2.5 indicated osteoporosis; –2.5 < T-score value <–1.0 indicated osteopenia; T-score value ≥ –1.0 indicated a normal bone mass.
The OSTA calculation formula was as follows: OSTA score = (weight [kg] – age [years]) × 0.2. Values were classified as follows: OSTA score < –4 indicated that the patient was at high risk of fracture; –4 ≤ OSTA score ≤–1 indicated a medium risk of fracture; and OSTA score > –1 indicated a low risk of fracture. The OSTC calculation formula was as follows: OSTC score = weight (kg) –2 × age (years) + 50. Values were classified as follows: OSTC score ≤0 indicated that the patient was at risk for osteoporosis; and an OSTC score > 0 indicated that the patient was at no risk for osteoporosis.
Statistical analyses
All statistical analyses were performed using PASW Statistics for Windows, Version 18.0 (SPSS Inc., Chicago, IL, USA). All data are presented as mean ± SD. Based on the BMD T-score value of the patients that reached the diagnostic criteria for osteoporosis, receiver operating characteristic (ROC) curve analyses of OSTA, OSTC and osteoporosis were undertaken. The area under curve (AUC) was analysed to obtain the best diagnostic cut-off points and 95% confidence intervals of the AUC were calculated. A P-value < 0.05 was considered statistically significant.
Results
This retrospective study enrolled 404 postmenopausal women with T2DM and their clinicopathological features are summarized in Table 1. The mean ± SD age of the study cohort was 69.0 ± 12.2 years (range, 50–93 years). The mean ± SD body weight was 59.2 ± 10.1 kg. Before the patients were recruited, based on the diagnosis of T2DM according to World Health Organization guidelines (1999), 237 of 404 patients (58.7%) had T2DM for > 3 years. Of these patients, 155 patients (65.4%) were being treated with insulin and its analogues. A total of 287 of 404 patients (71.0%) had complications associated with T2DM such as diabetic foot ulcers, diabetic nephropathy and diabetic peripheral neuropathy. The OSTA and OSTC scores decreased with increasing age, which was consistent with the left femoral neck BMD and T-scores (Table 2). The lumbar spine (L1–L4) BMD showed a similar change with increasing age although it was not as marked. These data indicated that the OSTA and OSTC scores might be able to identify osteoporosis.
Table 1.
Baseline demographic and clinical characteristics of the postmenopausal female patients with type 2 diabetes (n = 404) who participated in this study to measure the use of two screening tools, the osteoporosis self-assessment tool for Asians and the osteoporosis screening tool for Chinese women, compared with dual-energy X-ray absorptiometry in the diagnosis of osteoporosis.
| Characteristic | Mean ± SD |
|---|---|
| Age, years | 69.0 ± 12.2 |
| Body weight, kg | 59.2 ± 10.1 |
| Height, cm | 157.6 ± 9.1 |
| Fasting blood glucose, mmol/l | 10.5 ± 3.3 |
| Plasma glucose at 2 h after meal, mmol/l | 19.3 ± 5.7 |
| Glycosylated haemoglobin, % | 8.6 ± 1.9 |
Table 2.
Comparison of the scores for the two screening tools used to predict osteoporosis, the osteoporosis self-assessment tool for Asians (OSTA) and the osteoporosis screening tool for Chinese women (OSTC), compared with bone mineral density (BMD) measurements from dual-energy X-ray absorptiometry in the diagnosis of osteoporosis in postmenopausal female patients with type 2 diabetes (n = 404) stratified according to age.
| Age, years | Weight, kg | n | OSTA | OSTC |
Lumbar spine (L1–L4) |
Left femoral neck |
||
|---|---|---|---|---|---|---|---|---|
| BMD | T-score | BMD | T-score | |||||
| 50–59 | 60.0 ± 9.1 | 67 | 1.03 ± 1.92 | 0.36 ± 10.71 | 1.06 ± 0.19 | –0.46 ± 1.55 | 0.89 ± 0.11 | –0.31 ± 0.93 |
| 60–69 | 59.8 ± 10.0 | 156 | –1.02 ± 2.09 | –20.01 ± 11.54 | 0.96 ± 0.19 | –1.28 ± 1.54 | 0.78 ± 0.12 | –1.28 ± 1.01 |
| 70–79 | 58.8 ± 10.1 | 131 | –3.10 ± 2.12 | –39.73 ± 11.68 | 0.91 ± 0.17 | –1.69 ± 1.44 | 0.70 ± 0.13 | –1.94 ± 1.09 |
| ≥80 | 57.4 ± 9.1 | 50 | –5.47 ± 2.00 | –62.14 ± 11.98 | 0.91 ± 0.19 | –1.66 ± 1.56 | 0.65 ± 0.14 | –2.37 ± 1.16 |
| All | 59.2 ± 10.1 | 404 | –1.90 ± 2.83 | –28.24 ± 21.89 | 0.96 ± 0.19 | –1.32 ± 1.57 | 0.75 ± 0.15 | –1.47 ± 1.22 |
Data presented as mean ± SD.
To determine if the OSTA and OSTC scores could efficiently identify osteoporosis, the detection rates of osteoporosis and low BMD measured using DXA, OSTA and OSTC were analysed (Tables 3 and 4). The detection rates for osteoporosis (T-score value ≤ –2.5) with DXA in the lumbar spine (L1–L4) and the left femoral neck were 22.5% (91 of 404 patients) and 21.8% (88 of 404 patients), respectively; while the detection rates of osteoporosis in the OSTA medium–high risk group were 14.4% (58 of 404 patients) and 18.1% respectively (73 of 404 patients); and in the OSTC at risk group it was 21.5% (87 of 404 patients) for both skeletal sites.
Table 3.
Comparison of the screening results for the two screening tools used to predict osteoporosis, the osteoporosis self-assessment tool for Asians (OSTA) and the osteoporosis screening tool for Chinese women (OSTC), compared with bone mineral density measurements of the lumbar spine from dual-energy X-ray absorptiometry (DXA) in postmenopausal female patients with type 2 diabetes (n = 404).
| Screening classification |
Lumbar spine (L1–L4) T-score |
All | ||
|---|---|---|---|---|
| ≤–2.5 | –2.5 < T-score < –1 | ≥–1 | ||
| OSTA | ||||
| Medium–high risk | 58 (14.4%) | 97 (24.0%) | 94 (23.3%) | 249 (61.6%) |
| Low risk | 33 (8.2%) | 54 (13.4%) | 68 (16.8%) | 155 (38.4%) |
| OSTC | ||||
| At risk | 87 (21.5%) | 138 (34.2%) | 139 (34.4%) | 364 (90.1%) |
| No risk | 4 (1.0%) | 13 (3.2%) | 23 (5.7%) | 40 (9.9%) |
| DXA | 91 (22.5%) | 151 (37.4%) | 162 (40.1%) | 404 (100.0%) |
Data presented as n of 404 patients (%).
Table 4.
Comparison of the screening results for the two screening tools used to predict osteoporosis, the osteoporosis self-assessment tool for Asians (OSTA) and the osteoporosis screening tool for Chinese women (OSTC), compared with bone mineral density measurements of the left femoral neck from dual-energy X-ray absorptiometry (DXA) in postmenopausal female patients with type 2 diabetes (n = 404).
| Screening classification |
Left femoral neck T-score |
All | ||
|---|---|---|---|---|
| ≤–2.5 | –2.5 < T-score < –1 | ≥–1 | ||
| OSTA | ||||
| Medium–high risk | 73 (18.1%) | 108 (26.7%) | 68 (16.8%) | 249 (61.6%) |
| Low risk | 15 (3.7%) | 63 (15.6%) | 77 (19.1%) | 155 (38.4%) |
| OSTC | ||||
| At risk | 87 (21.5%) | 164 (40.6%) | 113 (28.0%) | 364 (90.1%) |
| No risk | 1 (0.2%) | 7 (1.7%) | 32 (7.9%) | 40 (9.9%) |
| DXA | 88 (21.8%) | 171 (42.3%) | 145 (35.9%) | 404 (100.0%) |
Data presented as n of 404 patients (%).
For the osteopenia BMD results (2.5 < T-score value < –1.0), the detection rates with DXA in the lumbar spine (L1–L4) and the left femoral neck were 37.4% (151 of 404 patients) and 42.3% (171 of 404 patients) (Tables 3 and 4), respectively. At the left femoral neck, 26.7% (108 of 404 patients) were in the OSTA medium–high risk group and 40.6% (164 of 404 patients) were in the OSTC at risk group, but at the lumbar spine (L1–L4), the detection rates in the OSTA medium–high risk group and the OSTC at risk group were 24.0% (97 of 404 patients) and 34.2% (138 of 404 patients), respectively. These findings indicate that the detection rates for OSTC were higher than those for OSTA in terms of osteoporosis and osteopenia detection in both the lumbar spine (L1–L4) and the left femoral neck.
With regard to the lumbar spine (L1–L4), the AUCs from the ROC curve analysis are shown in Table 5. The AUCs of OSTA and OSTC screening for osteoporosis were 0.55 (95% confidence interval [CI] 0.4804, 0.6158) and 0.57 (95% CI 0.5070, 0.6376), respectively; and the diagnostic efficiency of both tools was low. For the left femoral neck, the AUCs of OSTA and OSTC screening for osteoporosis were 0.73 (95% CI 0.6681, 0.7872) and 0.78 (95% CI 0.7296, 0.8312), respectively (Figure 1 and Table 5). With regard to the left femoral neck as the detection site, the sensitivity and specificity of OSTA and OSTC screening for osteoporosis were 64.9%, 64.2% and 72.7%, 79.5%, respectively; and the best diagnostic cut-off points were –2.3 and –29.5, respectively (Table 5).
Table 5.
Predictive value of the two screening tools, the osteoporosis self-assessment tool for Asians (OSTA) and the osteoporosis screening tool for Chinese women (OSTC), to predict osteoporosis at the lumbar spine (L1–L4) and the left femoral neck in postmenopausal female patients with type 2 diabetes (n = 404).
| Anatomical site | Screening tool | AUC | Cut-off point | Sensitivity, % | Specificity, % |
|---|---|---|---|---|---|
| Lumbar spine (L1–L4) | OSTA | 0.55 | –2.7 | 65.0% | 48.9% |
| OSTC | 0.57 | –25.5 | 51.0% | 63.3% | |
| Femoral neck | OSTA | 0.73 | –2.3 | 64.9% | 72.7% |
| OSTC | 0.78 | –29.5 | 64.2% | 79.5% |
AUC, area under the curve.
Figure 1.
Receiver operating characteristic curve for the two screening tools, the osteoporosis self-assessment tool for Asians (OSTA) and the osteoporosis screening tool for Chinese women (OSTC), to predict osteoporosis the left femoral neck in postmenopausal female patients with type 2 diabetes (n = 404).
Discussion
The present study evaluated the accuracy of the OSTA and OSTC tools for the screening of osteoporosis and osteopenia in postmenopausal Chinese women with T2DM. The detection rates of OSTC were higher than OSTA for both osteoporosis and osteopenia at both anatomical sites (i.e. lumbar spine L1–L4 and left femoral neck). Furthermore, this current study demonstrated that the sensitivity and specificity of OSTC were both greater than OSTA regardless of the anatomical site.
Type 2 diabetes mellitus is a risk factor for osteoporosis.18 DXA is the gold standard for the diagnosis of osteoporosis but a survey showed that only 14.4% of patients at a high risk of osteoporosis received DXA for BMD testing in China.19 To be widely used to screen a large population with T2DM, an assessment tool must be as simple as possible. The World Health Organization recommends the fracture risk assessment tool, known as FRAX, which combines at least 10 risk factors.20 At present, OSTA and OSTC are the main screening tools for osteoporosis in Asian countries. They are both simple, quick and inexpensive fracture risk assessment tools that only need the two variables of age and body weight.10,13 In this current study, DXA, OSTC and OSTA were used to measure lumbar spine (L1–L4) and left femoral neck BMD in menopausal women with T2DM and it found that the OSTA and OSTC scores decreased with age, which was consistent with the left femoral neck BMD and T-score values.
Dual-energy X-ray absorptiometry is not affordable at every healthcare centre in China because of the high cost and complicated methodology. Studies have reported conflicting data on BMD and the risk of osteoporosis in patients with T2DM.21–23 Some research has demonstrated that material changes and structural abnormalities led to increased bone fragility in patients with T2DM.24 The OSTA and OSTC tools are simple methods to assess bone strength that can be used to assess osteoporosis without the use of DXA. Previous studies have shown that OSTA and OSTC provided a reliable estimation of mechanical bone quality.13,25 The present study showed that the detection rates for osteoporosis at the lumbar spine (L1–L4) and left femoral neck in the OSTA medium–high risk group were 14.4% and 18.1%, respectively; and in OSTC at risk group it was 21.5% at both anatomical sites; all of which were a little lower than for the DXA measurements. The detection rates for osteopenia using the OSTC tool were similar to those of DXA at both anatomical sites. These findings suggest that these two screening tools could be used for screening for osteoporosis in Chinese patients with T2DM.
The sensitivity and specificity of OSTA in the diagnosis of osteoporosis in a Japanese population were 91% and 45%, respectively.26 However, research has shown that OSTA screening for osteoporosis in Chinese menopausal women was less sensitive than other Asian countries.27 This current study found that the OSTA and OSTC tools had poor consistency with the DXA measurements in postmenopausal women with T2DM when the lumbar spine was taken as the detection site, indicating that neither of the two screening tools was suitable for osteoporosis screening at the lumbar spine. With the left femoral neck as the detection site, the diagnostic consistency between OSTA, OSTC and DXA was acceptable. The AUC of the OSTC tool was greater than the OSTA tool, indicating that the OSTC might be the preferred assessment tool.
This current study had several limitations. First, it was a retrospective single-centre study, which may have resulted in selection bias. A prospective multi-centre study would be more appropriate for the prediction of incident fractures. Secondly, the sample size was relatively small and the study only enrolled Asian patients, so the findings should be further verified in other larger cohorts and different ethnic populations. Previous studies investigated the important role of depression or anxiety disorders in chronic diseases such as osteoporosis and T2DM, but these are not factored into the OSTA and OSTC tools.28,29 The mutual inter-relationships deserve further research.
In conclusion, the OSTA and OSTC osteoporosis assessment tools are suitable for the early screening of osteoporosis in the femoral neck in postmenopausal female patients with T2DM in China. The findings of this current study suggest that the OSTC tool would be the optimal choice and the best diagnostic cut-off point was –29.5. The OSTC calculation is simple and could be readily used for the early screening of osteoporosis at basic medical and health institutions in China.
Acknowledgements
We appreciate the participation of all the patients enrolled in this study. We also thank Editage for their support.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This work was supported by a grant from the Medical Research Project of Foshan Health and Family Planning Commission (no. 20160215).
ORCID iD
Shuai Liu https://orcid.org/0000-0002-8775-3245
References
- 1.Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014; 103: 137–149. [DOI] [PubMed] [Google Scholar]
- 2.Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med 2001; 345: 790–797. [DOI] [PubMed] [Google Scholar]
- 3.Greenhill C. Shared variants for osteoporosis and T2DM. Nat Rev Endocrinol 2018; 14: 627. [DOI] [PubMed] [Google Scholar]
- 4.Harris AM, Lee AR, Wong SC. Systematic review of the effects of bisphosphonates on bone density and fracture incidence in childhood acute lymphoblastic leukaemia. Osteoporos Int 2020; 31: 59–66. [DOI] [PubMed] [Google Scholar]
- 5.Kendler DL, Compston J, Carey JJ, et al. Repeating measurement of bone mineral density when monitoring with dual-energy X-ray absorptiometry: the 2019 ISCD official position. J Clin Densitom 2019; 22: 489–500. [DOI] [PubMed] [Google Scholar]
- 6.Crandall CJ. Risk assessment tools for osteoporosis screening in postmenopausal women: a systematic review. Curr Osteoporos Rep 2015; 13: 287–301. [DOI] [PubMed] [Google Scholar]
- 7.Aw D, Thain J, Ali A, et al. Predicting fracture risk in osteoporosis: the use of fracture prediction tools in an osteoporosis clinic population. Postgrad Med J 2016; 92: 267–270. [DOI] [PubMed] [Google Scholar]
- 8.Yang Y, Wang B, Fei Q, et al. Validation of an osteoporosis self-assessment tool to identify primary osteoporosis and new osteoporotic vertebral fractures in postmenopausal Chinese women in Beijing. BMC Musculoskelet Disord 2013; 14: 271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koh LK, Sedrine WB, Torralba TP, et al. A simple tool to identify Asian women at increased risk of osteoporosis. Osteoporos Int 2001; 12: 699–705. [DOI] [PubMed] [Google Scholar]
- 10.Su FM, Liu DH, Chen JF, et al. Development and validation of an Osteoporosis Self-Assessment Tool for Taiwan (OSTAi) postmenopausal women – a sub-study of the Taiwan OsteoPorosis Survey (TOPS). PLoS One 2015; 10: e0130716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Si L, Winzenberg TM, Chen M, et al. Screening for osteoporosis in Chinese post-menopausal women: a health economic modelling study. Osteoporos Int 2016; 27: 2259–2269. [DOI] [PubMed] [Google Scholar]
- 12.Meng J, Sun N, Chen Y, et al. Artificial neural network optimizes self-examination of osteoporosis risk in women. J Int Med Res 2019; 47: 3088–3098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang J, Wu T, Yang D. A study on osteoporosis screening tool for Chinese women. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2007; 21: 86–89 [Article in Chinese, English abstract]. [PubMed] [Google Scholar]
- 14.Wannamethee SG, Shaper AG. Weight change and duration of overweight and obesity in the incidence of type 2 diabetes. Diabetes Care 1999; 22: 1266–1672. [DOI] [PubMed] [Google Scholar]
- 15.Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013; 310: 948–959. [DOI] [PubMed] [Google Scholar]
- 16. IDF Clinical Guidelines Task Force. Global Guideline for Type 2 Diabetes: recommendations for standard, comprehensive, and minimal care. Diabet Med 2006; 23: 579–593. [DOI] [PubMed] [Google Scholar]
- 17.Wu XP, Liao EY, Zhang H, et al. Determination of age-specific bone mineral density and comparison of diagnosis and prevalence of primary osteoporosis in Chinese women based on both Chinese and World Health Organization criteria. J Bone Miner Metab 2004; 22: 382–391. [DOI] [PubMed] [Google Scholar]
- 18.Lipscombe LL, Jamal SA, Booth GL, et al. The risk of hip fractures in older individuals with diabetes: a population-based study. Diabetes Care 2007; 30: 835–841. [DOI] [PubMed] [Google Scholar]
- 19.Han W, Bai X, Wang N, et al. Association between lumbar bone mineral density and serum uric acid in postmenopausal women: a cross-sectional study of healthy Chinese population. Arch Osteoporos 2017; 12: 50. [DOI] [PubMed] [Google Scholar]
- 20.Kanis JA, McCloskey EV, Johansson H, et al. Development and use of FRAX in osteoporosis. Osteoporos Int 2010; 21(Suppl 2): S407–S413. [DOI] [PubMed] [Google Scholar]
- 21.Tomczak RL, VanCourt R. Metatarsal insufficiency fractures in previously undiagnosed osteoporosis patients. J Foot Ankle Surg 2000; 39: 174–183. [DOI] [PubMed] [Google Scholar]
- 22.Stavem K, Naumann MG, Sigurdsen U, et al. Association of body mass index with the pattern of surgically treated ankle fractures using two different classification systems. J Foot Ankle Surg 2017; 56: 314–318. [DOI] [PubMed] [Google Scholar]
- 23.Ma L, Oei L, Jiang L, et al. Association between bone mineral density and type 2 diabetes mellitus: a meta-analysis of observational studies. Eur J Epidemiol 2012; 27: 319–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leslie WD, Rubin MR, Schwartz AV, et al. Type 2 diabetes and bone. J Bone Miner Res 2012; 27: 2231–2237. [DOI] [PubMed] [Google Scholar]
- 25.Wang P, Abdin E, Shafie S, et al. Estimation of prevalence of osteoporosis using OSTA and its correlation with sociodemographic factors, disability and comorbidities. Int J Environ Res Public Health 2019; 16: pii: E2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chin KY. A review on the performance of osteoporosis self-assessment tool for Asians in determining osteoporosis and fracture risk. Postgrad Med 2017; 129: 734–746. [DOI] [PubMed] [Google Scholar]
- 27.Liu Z, Gao H, Bai X, et al. Evaluation of Singh Index and Osteoporosis Self-Assessment Tool for Asians as risk assessment tools of hip fracture in patients with type 2 diabetes mellitus. J Orthop Surg Res 2017; 12: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Catalano A, Martino G, Bellone F, et al. Anxiety levels predict fracture risk in postmenopausal women assessed for osteoporosis. Menopause 2018; 25: 1110–1115. [DOI] [PubMed] [Google Scholar]
- 29.Martino G, Catalano A, Bellone F, et al. As time goes by: anxiety negatively affects the perceived quality of life in patients with type 2 diabetes of long duration. Front Psychol 2019; 10: 1779. [DOI] [PMC free article] [PubMed] [Google Scholar]