Short abstract
Osteoid osteoma is a small benign bone tumor that is primarily localized in long bone; lumbar osteoid osteoma combined with scoliosis has rarely been reported. Here, we describe a 9-year-old boy who complained of back pain and scoliosis. He underwent nidus resection and did not experience complications or osteoid osteoma recurrence. His pain and scoliosis were relieved after the operation. The findings in this case indicate that resection of osteoid osteoma is an effective and safe method of treatment. The lumbar spine is the most common location of osteoid osteoma, which causes painful scoliosis. Nidus resection can provide relief of back pain and scoliosis.
Keywords: Osteoid osteoma, back pain, scoliosis, resection, lumbar vertebrae, lumbosacral region, bone neoplasms
Introduction
Osteoid osteoma is a small benign bone tumor that arises from osteoblasts, which was first described by Jaffe in 19351 as a smaller version of an osteoblastoma. A tumor size of <1.5 cm was regarded as an osteoid osteoma, while a tumor of >1.5 cm was regarded as an osteoblastoma. Approximately 10% of osteoid osteomas occur in the spine; the majority of spinal osteoid osteomas occur in lumbar vertebrae, commonly in the posterior elements. Osteoid osteoma commonly occurs in the second decade of life, and is more common in boys than in girls (approximate ratio of 3:1).2,3 The typical chief complaints are pain that worsens at night and is relieved by administration of aspirin. The pain is caused by vascular pressure and the production of prostaglandins in the nidus of the osteoid osteoma.4 These aspects underlie the responses of osteoid osteomas to treatment with non-steroid anti-inflammatory drugs. Scoliosis resulting from spinal osteoid osteoma has been reported to cause painful scoliosis in 70% of adolescent patients; this painful scoliosis may be caused by paravertebral muscle spasm.5
Computed tomography (CT) is regarded as the best diagnostic tool for nidus identification and localization; magnetic resonance imaging (MRI) is less accurate than CT.6 Recently, interstitial laser photocoagulation and percutaneous radiofrequency coagulation have become increasingly popular for the treatment of non-spinal osteoid osteoma.7 Wang et al. showed that CT-guided percutaneous radiofrequency ablation was safe and effective for the treatment of spinal osteoid osteoma; however, this method is not indicated for lesions that are in close proximity to neurological structures.8 Surgery is the most common method for treatment of spinal osteoid osteoma; the prognosis for pain relief is good when en bloc resection of the tumor is performed. Here, we describe a patient who had an L5 osteoid osteoma, which was successfully treated by surgical resection.
Case report
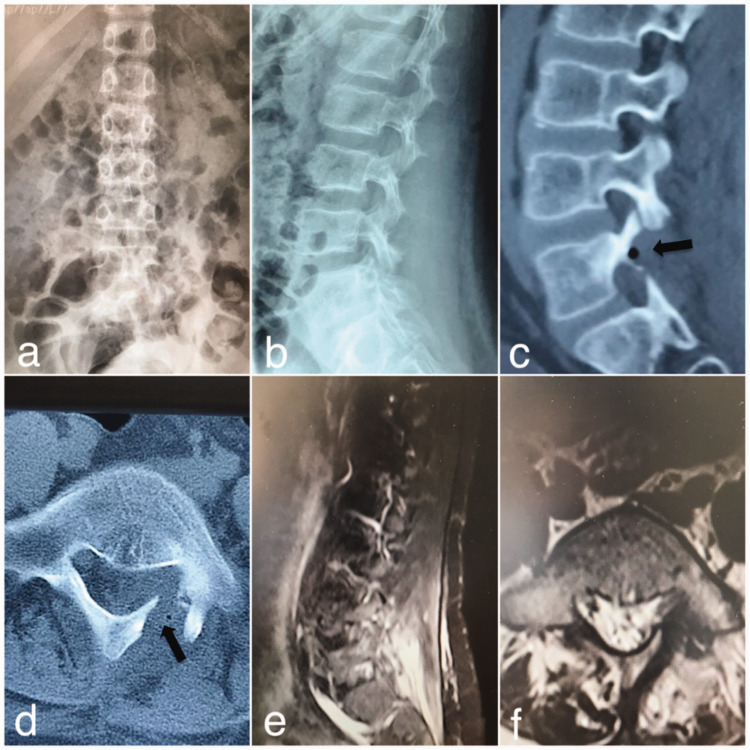
A 9-year-old boy presented with the complaint of lower back pain that had been present for 3 months and became aggravated at night. Physical examination revealed lumbar percussion pain and tenderness, combined with lumbar scoliosis. Neurologic examinations and laboratory analysis revealed no abnormalities. CT findings revealed a nidus in the left lamina of the L5 vertebrae. The nidus size was 4 mm. MRI showed inflammatory changes in the entire left pedicle, as well as the left lamina and vertebral body (Figure 1). However, the tumor did not compress the nerve root. Therefore, the patient was diagnosed with osteoid osteoma.
Figure 1.
(a, b) Anteroposterior and lateral views of the lumbar spine revealed scoliosis, with absence of thoracic vertebrae rotation and minimal lumbar vertebrae rotation to the concave side. (c, d) Computed tomography scans revealed the nidus of the osteoid osteoma (black arrows). (e, f) Magnetic resonance imaging showed edema and inflammatory changes of the lamina and paravertebral soft tissue (red arrows).
We performed surgery using a traditional posterior approach, with the patient under general anesthesia. When the L5 level was identified under fluoroscopic control, partial laminectomy was performed as necessary. Total nidus resection was completed by using an osteotome. Histology and pathology findings confirmed the diagnosis of osteoid osteoma. The patient reported absence of pain and scoliosis after surgery. Postoperative anteroposterior imaging revealed that the scoliosis had disappeared. Postoperative CT revealed that the nidus had been completely resected, while postoperative MRI demonstrated resolution of edema in the lamina and paravertebral soft tissue (Figure 2). Routine follow-up was performed at 1 week, 6 weeks, and 6 months postoperatively. During 18 months of follow-up, the patient remained asymptomatic without recurrence of osteoid osteoma. The patient and his family consented to the publication of this case report.
Figure 2.
(a, b) Anteroposterior and lateral views of the lumbar spine showed disappearance of lumbar scoliosis. (c, d) Computed tomography scan showed en bloc resection of the nidus (black arrows). (e, f) Magnetic resonance imaging showed relief of edema and inflammatory changes in the lamina and paravertebral soft tissue.
Discussion
Patients with osteoid osteomas generally complain of pain that increases in severity during the night. This pain can be relieved by administration of non-steroid anti-inflammatory drugs. Some affected patients may present with painful scoliosis. Uehara et al. described a patient with osteoid osteoma who had presented with thoracic scoliosis; the patient complained of scoliosis without back pain or other problems.9 In the patient described by Uehara et al., the pain-related scoliosis resolved upon relief of the pain, similar to our patient; however, true scoliosis does not resolve. Moreover, patients with true scoliosis may exhibit deformities of the vertebral body, such as hemivertebrae or butterfly vertebrae, which are visible in X-ray images or CT scans.10 In patients with osteoid osteoma, pain generally arises from spasms of the paravertebral muscle, which cause pain-related scoliosis. Consistent with the findings in prior case reports, our patient complained of night pain and scoliosis.
Osteoid osteoma tumors can be detected by CT scans and bone scans; CT is more commonly used. Classically, CT scans of patients with osteoid osteoma have revealed a nidus with central mineralization and varying degrees of perennial sclerosis.11 However, CT findings in the spine depend on the position of the nidus; if its location is subchondral, sclerosis may be absent. In addition, if incisions are made at an inappropriate level or are excessively wide, the nidus of the tumor may be missed. Bone scanning represents a more sensitive method for localization of the tumor. In particular, the technetium bone scan method provides accurate localization of the lesion.12 For detection of changes in soft tissue and bone marrow around the nidus, MRI is a more sensitive modality than CT. However, MRI findings can be misleading in patients with osteoid osteoma.13 Therefore, it is necessary to rule out low-grade infection, as well as tuberculosis and Brodie abscesses, when using MRI findings for diagnosis of patients with osteoid osteoma. CT should be used when evaluating benign tumors with known inflammatory responses on MRI. The majority of spinal osteoid osteomas are located in lumbar vertebrae and the posterior elements; indeed, in our patient, the nidus was found in the left lamina of the L5 vertebrae. Osteoblastoma histology resembles that of osteoid osteoma; these tumors can be differentiated by size. The differential diagnosis should also include osteochondroma, aneurysmal bone cyst, and giant cell tumor. Furthermore, pain-related scoliosis can be caused by conditions such as lumbar disc herniation, muscular spasm, and discogenic pain; these should also be ruled out.14
Treatment varies based on the condition of the affected patient. Some patients can be treated successfully by a conservative approach. However, most patients cannot tolerate long-term conservative treatment. If medication therapy fails or if the lesion increases in size, patients are selected for surgery with the aim of en bloc resection of the tumor. After resection of an osteoid osteoma, pain and scoliosis are relieved. Radiofrequency ablation is an attractive method because it involves minimal bone destruction and is minimally invasive, with adequate safety and efficacy.15,16 Radiofrequency ablation can be combined with guided bone biopsy. However, radiofrequency ablation is more widely used for non-spinal osteoid osteomas3 owing to the risk of damage to neural structures. We considered radiofrequency ablation to be inappropriate for our patient because his osteoid osteoma was adjacent (1.45 mm) to the dura. Moreover, minimally invasive surgeries, such as those involving video endoscopy, microscopy, and imaging-guided or navigation-guided techniques also achieve satisfactory outcomes.17 However, these methods have steep learning curves, as well as requirements for additional education and equipment.18,19
In this report, we have described a patient with a rare L5 osteoid osteoma, who complained of lumbar pain and scoliosis. The patient underwent nidus resection without any complications; his pain and scoliosis were relieved after the surgery. Our findings demonstrate that, if the osteoid osteoma nidus exhibits close proximity to the neural canal, resection of the osteoid osteoma is an effective and safe treatment method. The lumbar spine is the most common location of osteoid osteoma, which causes painful scoliosis. Nidus resection can provide relief of back pain and scoliosis in affected patients.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Wei-hu Ma https://orcid.org/0000-0001-5489-0203
References
- 1.Jaffe HL. “Osteoid-osteoma”: a benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg 1935; 31: 709–728. [Google Scholar]
- 2.Nemoto O, Moser RP, Jr, Van Dam BEet al. Osteoblastoma of the spine. A review of 75 cases. Spine 1990, 15: 1271–1280. [DOI] [PubMed] [Google Scholar]
- 3.Gasbarrini A, Cappuccio M, Bandiera Set al. Osteoid osteoma of the mobile spine: surgical outcomes in 81 patients. Spine (Phila Pa 1976) 2011; 36: 2089–2093. [DOI] [PubMed] [Google Scholar]
- 4.Sherman MS, McFarland G., Jr. Mechanism of pain in osteoid osteomas. South Med J 1965; 58: 163–166. [DOI] [PubMed] [Google Scholar]
- 5.Pourfeizi HH, Tabrizi A, Bazavar MRet al. Clinical findings and results of surgical resection of thoracolumbar osteoid osteoma. Asian Spine J 2014; 8: 150–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qiao J, Zhu F, Zhu Zet al. Conservative treatment for osteoid osteoma of the odontoid process of the axis: a case report. World J Surg Oncol 2014; 12: 305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barei DP, Moreau G, Scarborough MTet al. Percutaneous radiofrequency ablation of osteoid osteoma. Clin Orthop Relat Res 2000; 373: 115–124. [DOI] [PubMed] [Google Scholar]
- 8.Wang B, Song BH, Liang Jet al. Percutaneous radiofrequency ablation for spinal osteoid osteoma and osteoblastoma. Eur Spine J 2017; 26: 1–9. [DOI] [PubMed] [Google Scholar]
- 9.Uehara M, Takahashi J, Kuraishi Set al. Osteoid osteoma presenting as thoracic scoliosis. Spine J 2015; 15: e77. [DOI] [PubMed] [Google Scholar]
- 10.Hedequist D, Emans J. Congenital scoliosis. J Am Acad Orthop Surg 2004; 12: 61–66. [DOI] [PubMed] [Google Scholar]
- 11.Harish S, Saifuddin A. Imaging features of spinal osteoid osteoma with emphasis on MRI findings. Eur Radiol 2005; 15: 2396–2403. [DOI] [PubMed] [Google Scholar]
- 12.Nebreda CL, Vallejo R, Mayoral-Rojals Vet al. Osteoid osteoma: benign osteoblastic tumor of the lumbar L4 transverse process associated with radicular pain: a case report. Pain Pract 2018; 18: 118–122. [DOI] [PubMed] [Google Scholar]
- 13.Chakrapani SD, Grim K, Kaimaktchiev Vet al. Osteo-blastoma of the spine with discordant magnetic resonance imaging and computed tomography imaging in a child. Spine 2008; 33: E968–E970. [DOI] [PubMed] [Google Scholar]
- 14.Ravindra VM, Eli IM, Schmidt MHet al. Primary osseous tumors of the pediatric spinal column: review of pathology and surgical decision making. Neurosurg Focus 2016; 41: E3. [DOI] [PubMed] [Google Scholar]
- 15.Weber MA, Sprengel SD, Omlor GWet al. Clinical long-term outcome, technical success, and cost analysis of radiofrequency ablation for the treatment of osteoblastomas and spinal osteoid osteomas in comparison to open surgical resection. Skeletal Radiol 2015; 44: 981–993. [DOI] [PubMed] [Google Scholar]
- 16.Morassi LG, Kokkinis K, Evangelopoulos DSet al. Percutaneous radiofrequency ablation of spinal osteoid osteoma under CT guidance. Br J Radiol 2014; 87: 20140003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoshioka K, Matsuda E, Murakami Het al. Microendoscopic excision of osteoid osteoma in the pedicle of the third lumbar vertebra. Asian Spine J 2015; 9: 958–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moore T, McLain RF. Image-guided surgery in resection of benign cervicothoracic spinal tumors: a report of two cases. Spine J 2005; 5: 109–114. [DOI] [PubMed] [Google Scholar]
- 19.Nagashima H, Nishi T, Yamane Ket al. Case report: osteoid osteoma of the C2 pedicle: surgical technique using a navigation system. Clin Orthop Relat Res 2010; 468: 283–288. [DOI] [PMC free article] [PubMed] [Google Scholar]