Abstract
Introduction
We describe our initial experience with the React 68 catheter (Medtronic, Dublin, Ireland), an FDA-approved catheter designed for aspiration in cases of emergent large vessel occlusion, as compared with the ACE 68 catheter (Penumbra, Alameda, CA).
Methods
This observational study followed consecutive patients treated with the React catheter over a seven-month period at a comprehensive stroke center. Use of the device was per discretion of the operator. Patient demographics, thrombectomy technique, reperfusion scoring, and disposition were assessed. Performance was compared with patients treated with the ACE 68 catheter over a comparable period.
Results
We treated 47 patients using the React 68 catheter using either aspiration alone or a combination of aspiration and stent retriever technique. The catheter was used in a variety of circumstances including proximal and distal occlusions involving the anterior and posterior circulation. Modified TICI 2b-3 was achieved in 45 of the 47 patients. The React 68 was comparable to the ACE 68 by all performance measures.
Conclusion
The React 68 catheter is a large-bore reperfusion catheter with trackability suitable for use in direct aspiration for recanalization of emergent large vessel occlusion.
Keywords: Emergent large vessel occlusion, aspiration, thrombectomy
Introduction
Mechanical thrombectomy is the most effective treatment for emergent large vessel occlusion (ELVO) in qualifying patients.1–7 Current thrombectomy techniques include stent retrievers, direct aspiration through a large bore catheter,8 and combinations thereof. Although the initial positive clinical trials used stent retrievers, subsequent work has demonstrated non-inferiority of aspiration alone or in concert with stent retrievers.9–12 Because of the speed and technical simplicity, aspiration is frequently the initial technique of choice, with other methods such as stent retrieval used as adjunct or bail-out.
Aspiration catheters have two fundamental requirements: trackability to allow easy, atraumatic navigation through tortuous, distal vessels, and a large inner diameter to generate maximal aspiration force while resisting collapse. The first requirement has been achieved by building catheters with multiple segments of varying flexibility, starting from stiff proximally to more compliant distally.13–15 Advances in catheter technology have enabled increasingly larger inner diameter to improve engagement and subsequent aspiration of greater thrombus volume. There are currently a number of aspiration catheters available in the United States with ID equal or greater than 0.060″ (Table 1).
Table 1.
Large-bore aspiration catheters in the US market in 2018.
| Catheter | Company | ID | OD |
|---|---|---|---|
| Jet 7 | Penumbra | 0.072″ | 0.085″ |
| AXS Vecta | Stryker | 0.071″ | 0.085″ |
| React 71 | Medtronic | 0.071″ | 0.086″ |
| SOFIA PLUS | Microvention | 0.070″ | 0.082″ |
| React 68 | Medtronic | 0.068″ | 0.083″ |
| ACE 68 | Penumbra | 0.068″ | 0.080″ |
The React 68 catheter is a 0.068″ ID aspiration catheter from Medtronic (Dublin, Ireland) with end-to-end Nitinol construction in a coil and braid design. The distal tip is beveled to enable smooth tracking. In this paper, we describe our initial clinical experience using the catheter for direct aspiration and as a distal access catheter during stent retriever thrombectomy and compare the catheter performance with the ACE 68, a similar-sized aspiration catheter from Penumbra (Alameda, CA) that has been on the market longer in the United States.
Methods
We performed a retrospective observational study on consecutive patients treated for ELVO at our institution over a 17-month period from January 2018 to May 2019. Patients for the React cohort came from October 2018 (when the React 68 became available at our institution) up to May 2019. Use of the React catheter was at the discretion of the treating physician and was unavailable for a portion of the period because of high demand. Other aspiration catheters, including the ACE 68, Jet 7 and Sofia Plus, were used for treating ELVO patients during the same period. Patients from the ACE cohort came from January 2018 up to December 2018, which was chosen to provide a comparable sample size and limit overlap between the two periods, when operator discretion may have more of an effect. Only 3 of the ACE 68 patients were treated during concurrent availability of the React 68 catheter. The study was performed under the supervision and approval of our institutional review board (IRB). Consent was waived due to the observational nature of the study.
Patient population
Patients were selected according to AHA 2018 guidelines for endovascular treatment of ELVO16 and had ELVO confirmed by CTA or MRA prior to intervention. A subset of patients had CTA at an outside hospital prior to transfer. Those presenting to our institution less than 6 h from ictus were taken immediately to the angiography suite, while those presenting greater than 6 h from ictus were taken to MRI for evaluation of infarct volume prior to endovascular therapy.
Technique
The aspiration catheter was advanced under flush through a sheath, typically a Neuron Max (Penumbra, Alameda, CA). When possible, we would advance the catheter to the clot without a guidewire or microcatheter (SNAKE technique),17 which were used only in tortuous cases with difficult navigation. After bringing the catheter to the occlusion, flush was discontinued, the catheter was attached to primed pump tubing, and the pump started. Manufacturer specific pumps were used with the respective catheters, i.e. the Medtronic pump was used with the React catheter and the Penumbra pump was used with the ACE catheter. When suction pressure was maximal, the catheter was advanced into the clot face and the aspiration tubing valve opened rapidly to allow an immediate aspiration effect. The catheter remained on direct aspiration for 2–3 min before being drawn gently from the intracranial circulation. Angiography was performed immediately after withdrawing the catheter to assess the thrombectomy effect. If aspiration alone was unsuccessful after two attempts, a stent retriever was used for additional thrombectomy passes. Solitaire Platinum (Medtronic, Dublin, Ireland) and Trevo (Stryker, Fremont, CA) were used in cases requiring a stent retriever. In cases with very tortuous anatomy that limited advancement of the aspiration catheter, a stent retriever was deployed across the occlusion and used as distal support to advance the aspiration catheter while on suction, the so-called grappling hook technique.18 Reperfusion was scored by an interventional neuroradiologist using the modified TICI scale.
Data
Demographic information including patient gender, age, time of last seen well, presenting NIHSS, time of groin puncture, first pass and modified TICI score were obtained from the medical and imaging records. Statistics were calculated using the R open source statistics platform.19 Demographics were compared using t-test for normally distributed data, Mann–Whitney for non-normal distributions, and Chi-square for binomial data. Non-inferiority was determined by comparing overlap of the 95% confidence interval, calculated with a bootstrap technique.
Results
We included a total of 92 patients, aged 29–98 years old, last seen well from 20 min to 20 h, and NIHSS ranging from 2 to 26. Demographics between the patients treated with the different catheters were similar (Table 2), with a trend toward slightly younger patients and more posterior circulation patients in the React group. Modified TICI 2b or better was achieved in 83 of 92 patients (90%). Median procedure length (time from groin puncture to reperfusion) was 28.5 min (IQR 18.0–52.3 min). Four complications occurred, two in each catheter group, none of which were related to the aspiration catheter, including subarachnoid hemorrhage (2), cervical ICA dissection (1), and subclavian occlusion (1).
Table 2.
Demographics.
| Total | ACE 68 | React 68 | p | |
|---|---|---|---|---|
| N | 92 | 45 | 47 | |
| Sex | ||||
| F | 40 (43.5%) | 24 (53.3%) | 16 (34.0%) | 0.10 |
| M | 52 (56.5%) | 21 (46.7%) | 31 (66.0%) | |
| Age | 69 (59–79) | 71 (62–79) | 67 (57–77.5) | 0.06 |
| NIHSS | 17 (12–20) | 16 (11–19) | 18 (14.5–20.5) | 0.16 |
| Location | ||||
| Tandem | 12 (13%) | 7 (16%) | 5 (11%) | 0.55 |
| Anterior | 86 (93%) | 44 (98%) | 42 (89%) | |
| Posterior | 6 (7%) | 1 (2%) | 5 (11%) | 0.20 |
| tPA | 35 (38.1%) | 19 (42.2%) | 16 (34.0%) | 0.55 |
| LSW to GP (h) | 4.6 (3.0–9.2) | 4.6 (3.0–9.1) | 4.5 (3.0–9.15) | 0.90 |
Note: p values were calculated using the Chi-squared test for binomial data and Mann–Whitney test for other data.
NIHSS: National Institutes of Health Stroke Scale; tPA: tissue plasminogen activator; LSW to GP: last seen well to groin puncture.
The React 68 catheter performed similar to the ACE 68 catheter by all outcome measures (Table 3). TICI 2b-3 reperfusion rates (96 vs. 84%, p = 0.09) and time to reperfusion (22 vs. 36 min, p = 0.09) were comparable between the two catheters, with a slight trend in favor of the React catheter. Of note, we started using the SNAKE technique coincident with introduction of the React catheter, which could be a confounder on the time-to-reperfusion. Functional outcome (mRS 0–2) at discharge and 90 days was comparable between the two groups, with non-significant, slightly lower rate of favorable outcome in the React 68 group. Follow-up at 90 days was only available for 42 of 92 patients and recapitulated the findings at discharge.
Table 3.
Techniques and outcomes.
| ACE 68 (n = 45) | React 68 (n = 47) | p | Δ [CI] | |
|---|---|---|---|---|
| N passes | 1 (1–3) | 2 (1–3) | 0.40 | 0.13 [−0.49 0.71] |
| Grappling hook | 18 (40.0%) | 11 (23.4%) | 0.14 | −0.17 [−0.37 0.04] |
| First pass aspiration | 21 (46.7%) | 15 (31.9%) | 0.22 | −0.15 [−0.38 0.07] |
| Aspiration alone | 22 (48.9%) | 25 (53.2%) | 0.83 | 0.04 [−0.18 0.27] |
| Time to reperfusion (min) | 36 (22–53) | 22 (16.5–43) | 0.08 | −6.6 [−24.2 9.5] |
| mTICI 2b-3 | 38 (84.4%) | 45 (95.7%) | 0.09 | 0.11 [−0.03 0.25] |
| SICH | 2 (4.4%) | 2 (4.3%) | 0.99 | −0.002 [−0.09 0.08] |
| mRS 0–2 @ discharge | 15 (33.3%) | 9 (19.1%) | 0.19 | −.14 [−0.34 0.06] |
| mRS @ 90 days | 9 (45.0%) | 4 (23.5%) | 0.19 | −.22 [−.53 0.09] |
Note: p values were calculated using the Chi-squared test for binomial variables and Mann–Whitney test for other variables. Δ is the difference between the proportions (binomial variables) or median values (continuous variables) for the two catheters with the 95% confidence interval in brackets.
Trackability of the React 68 was assessed using a number of surrogate measures. The SNAKE technique, advancement of the aspiration catheter to the clot without requiring microcatheter or wire support, is a rough measure of trackability. SNAKE was attempted in all of the React group and successful at reaching clot face in 21%. SNAKE was only recently adopted at our institution and not routinely used during the ACE control group (only one patient). Grappling hook, or the use of distal stent retriever deployment to pull the aspiration catheter around sharp turns, was needed in 23% of patients in the React group compared with 40% in the ACE group (p = 0.14).
Aspiration efficacy was estimated using first pass aspiration and aspiration only success rates. Our practice utilizes aspiration on the first (ADAPT) and second passes, except in cases requiring the grappling hook technique to advance the aspiration catheter; therefore, in this series, aspiration success should not be confounded by operator preference or stentriever use. First pass aspiration TICI 2b-3 was achieved in 32% and aspiration alone recanalization was achieved in 53% of the React group, comparable to the ACE group (see Table 3).
Most of the occlusions involved the middle cerebral artery, M1 segment, although the React catheter was used for more distal (M2) and proximal (ICA terminus) occlusions. We used React for distal aspiration in five patients with tandem carotid occlusions to achieve reperfusion intracranially prior to angioplasty and/or stenting of the proximal lesion. In one case of basilar occlusion, the React catheter was advanced to the right V4 segment but could not be passed further because of small size of the hypoplastic segment distal to the PICA origin; thrombectomy was performed with a Trevo stent retriever using a combined stent retriever-aspiration technique.
Case illustrations
Case 1
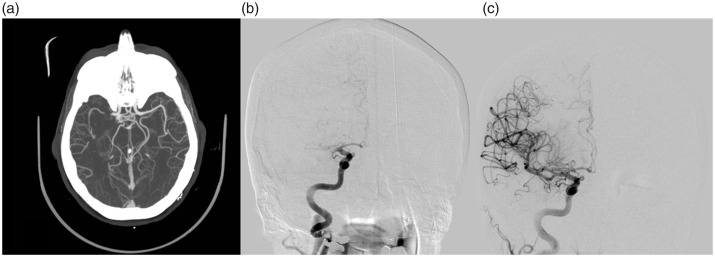
An elderly patient presented less than an hour after acute onset left hemiparesis and neglect. NIHSS was 10 for a right MCA syndrome and CTA demonstrated a right M1 occlusion (Figure 1). IV tPA was administered and the patient was brought directly to the angio suite from CT. After obtaining femoral access, a 6 Fr Neuron Max sheath was advanced over a Davis catheter (5 Fr Beacon tip Davis catheter, Cook, Bloomington IN) into the right internal carotid artery.
Figure 1.
Elderly patient presenting with acute left hemiparesis. (a) Axial MIPs from CTA demonstrate a right M1 occlusion with good collateral opacification. (b) Initial transfemoral catheter angiography confirms the right M1 occlusion. (c) Complete recanalization and reperfusion (mTICI 3) after two aspiration attempts.
The React aspiration catheter was introduced into the sheath, advanced directly to the ophthalmic ICA past multiple cervical ICA turns (Figure 1(b)), and then pushed over a Velocity microcatheter (Penumbra, Alameda, CA) and Synchro 2 microwire (Stryker, Fremont, CA) to the clot face. The microcatheter and microwire were removed and the aspiration system was activated. After 3 min of aspiration, the React catheter was withdrawn and angiography demonstrated only partial recanalization. Complete recanalization with distal reperfusion (mTICI 3) was achieved after a second aspiration (Figure 1(c)).
Case 2
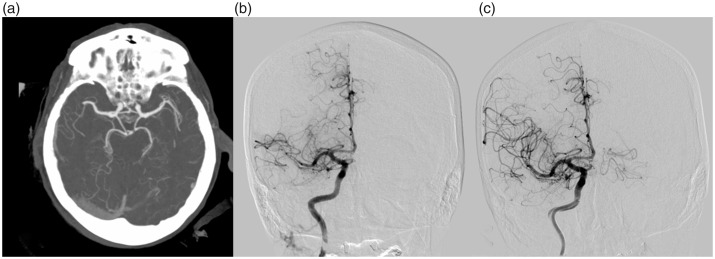
An elderly patient presented 30 min from last seen well with left hemiparesis. NIHSS was 20 for a right MCA syndrome. CTA demonstrated a right M2 occlusion (Figure 2). The Neuron Max sheath was placed in the right internal carotid artery via transfemoral access. The React aspiration catheter was connected to flush, introduced into the sheath and advanced to the ophthalmic segment. A Velocity microcatheter and Synchro 2 microwire were loaded into the catheter and then used to cross the thrombus in the superior division. The React aspiration catheter was not easily advanced beyond the ophthalmic segment despite having distal support. The microwire was removed and a 4 mm × 40 mm Solitaire Platinum stent retriever was deployed spanning the occlusion in the proximal M2 middle cerebral artery. Using the grappling hook technique, the React catheter was then advanced into the M1 segment and aspiration initiated. Combined stent retriever-aspiration was performed twice without success.
Figure 2.
Elderly patient presents with left hemiparesis. (a) Axial MIPs from CTA demonstrate a proximal right M2 occlusion. (b) Initial transfemoral catheter angiography confirms a proximal right M2 occlusion. (c) Complete recanalization of the proximal occlusion and good distal reperfusion (mTICI 2b) after three thrombectomy passes.
On the third pass, with the sheath high in the cervical ICA, we were able to advance the aspiration catheter over the microcatheter to the clot face without utilizing the stent retriever because of better proximal support. Recanalization of the proximal occlusion (mTICI 2b) was achieved after primary aspiration (Figure 2(c)).
Discussion
Direct aspiration as the first pass technique (also referred to as ADAPT, A Direct Aspiration, First Pass Technique) is a fast and simple method popular among interventionalists. Although direct aspiration was not included in the initial thrombectomy trials, multiple subsequent studies have demonstrated non-inferiority of aspiration to stent retrievers,9,20 including ASTER10 and COMPASS,12 trials randomizing to aspiration or stent retriever as first device, and Penumbra 3D separator,21 a trial randomizing to aspiration with or without a stent retriever. In some analyses, aspiration may be slightly faster than stent retrievers.22
The first large series describing aspiration utilized intermediate sized catheters with distal inner diameter of 0.054–0.057″.8,23 Subsequently, a number of companies have developed larger bore aspiration catheters with distal inner diameters from 0.068 to 0.072″ (Table 1). Bench studies suggest that larger bore catheters exert higher catheter tip force and aspiration flow rates.24 In clinical studies, a larger inner diameter increases recanalization rates and first-pass efficacy.11,25,26
In this series, we report on our initial experience with the React 68 catheter, which demonstrated excellent time to reperfusion and TICI 2b-3 reperfusion rates, comparable to an ACE 68 catheter control group treated at our institution in the immediate preceding time period. Although there were small differences in performance measures, none of these were statistically significant (Table 3). Subtle differences in catheter performance will require larger registry data to untangle.
The React catheter has excellent trackability for a large bore catheter. The catheter was advanced to the clot face on its own or over a microcatheter in 36 of 47 patients. In the other 11 patients, a grappling hook technique was required. Being able to advance the aspiration catheter without using the grappling hook technique can save precious minutes during prolonged thrombectomy and should cut down on time to reperfusion.
The large distal inner diameter of the React catheter (0.068″) is effective for direct aspiration. In our series, first pass mTICI 2b-3 was achieved by aspiration in 15 of 47 patients. Aspiration alone was successful in 25 of 47 patients and a combined aspiration-stent retriever technique was used in the remainder (mTICI 2b-3 in 96% total). Aspiration was performed in the proximal, large vessels, including the cervical ICA, and in distal vessels beyond the MCA bifurcation. We are unable to comment on performance in the presence of a proximal balloon guide catheter based on this series.
A larger version of the React catheter with an inner diameter of 0.071″ became available in the US market during data collection for this series. This may provide some advantage due to the expected larger aspiration force provided. However, further work will be needed to evaluate the trackability and durability of that product, and performance relative to other 0.071–072″ catheters.
Our study is subject to the typical limitations of a single center effort, with small patient numbers. However, we present a consistent treatment approach across multiple operators and demonstrate effective recanalization rates in a real-world population. Further, our angiographic outcomes are independently adjudicated by an interventional neuroradiologist and endovascular neurosurgeon.
Conclusion
We present the first systematic published data on the performance of the React 68, a large-bore reperfusion catheter with trackability suitable for thrombectomy in ELVO involving both proximal and distal occlusions in the anterior and posterior circulations.
Data sharing statement
The authors are willing to share the data on request.
Declaration of conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Patel is a consultant for Medtronic, Penumbra, and Microvention.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Scott B Raymond https://orcid.org/0000-0001-7008-8974
References
- 1.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 2.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 4.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 5.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 6.Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018; 378: 708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018; 378: 11–21. [DOI] [PubMed] [Google Scholar]
- 8.Jankowitz B, Aghaebrahim A, Zirra A, et al. Manual aspiration thrombectomy: adjunctive endovascular recanalization technique in acute stroke interventions. Stroke 2012; 43: 1408–1411. [DOI] [PubMed] [Google Scholar]
- 9.Stapleton CJ, Leslie-Mazwi TM, Torok CM, et al. A direct aspiration first-pass technique vs stentriever thrombectomy in emergent large vessel intracranial occlusions. J Neurosurg 2018; 128: 567–574. [DOI] [PubMed] [Google Scholar]
- 10.Lapergue B, Blanc R, Gory B, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER Randomized Clinical Trial. JAMA 2017; 318: 443–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alawieh A, Chatterjee AR, Vargas J, et al. Lessons learned over more than 500 stroke thrombectomies using ADAPT with increasing aspiration catheter size. Neurosurgery 2020; 86: 61–70. [DOI] [PubMed] [Google Scholar]
- 12.Turk AS, Siddiqui A, Fifi JT, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet 2019; 393: 998–1008. [DOI] [PubMed] [Google Scholar]
- 13.Simon SD, Ulm AJ, Russo A, et al. Distal intracranial catheterization of patients with tortuous vascular anatomy using a new hybrid guide catheter. Surg Neurol 2009; 72: 737–740. discussion 740. [DOI] [PubMed] [Google Scholar]
- 14.Spiotta AM, Hussain MS, Sivapatham T, et al. The versatile distal access catheter: the Cleveland Clinic experience. Neurosurgery 2011; 68: 1677–1686. discussion 1686. [DOI] [PubMed] [Google Scholar]
- 15.Park MS, Stiefel MF, Fiorella D, et al. Intracranial placement of a new, compliant guide catheter: technical note. Neurosurgery 2008; 63: E616–617. discussion E617. [DOI] [PubMed] [Google Scholar]
- 16.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018; 49: e46–e110. [DOI] [PubMed] [Google Scholar]
- 17.Heit JJ, Wong JH, Mofaff AM, et al. Sofia intermediate catheter and the SNAKE technique: safety and efficacy of the Sofia catheter without guidewire or microcatheter construct. J Neurointerv Surg 2018; 10: 401–406. [DOI] [PubMed] [Google Scholar]
- 18.Hui FK, Hussain MS, Spiotta A, et al. Merci retrievers as access adjuncts for reperfusion catheters: the grappling hook technique. Neurosurgery 2012; 70: 456–460; discussion 460. [DOI] [PubMed] [Google Scholar]
- 19.R_Core_Team. R: A language and environment for statistical computing, Vienna, Austria: R Foundation for Statistical Computing, 2013. [Google Scholar]
- 20.Phan K, Dmytriw AA, Teng I, et al. A direct aspiration first pass technique vs standard endovascular therapy for acute stroke: a systematic review and meta-analysis. Neurosurgery 2018; 83: 19–28. [DOI] [PubMed] [Google Scholar]
- 21.Nogueira RG, Frei D, Kirmani JF, et al. Safety and efficacy of a 3-dimensional stent retriever with aspiration-based thrombectomy vs aspiration-based thrombectomy alone in acute ischemic stroke intervention: a randomized clinical trial. JAMA Neurol 2018; 75: 304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsang COA, Cheung IHW, Lau KK, et al. Outcomes of stent retriever versus aspiration-first thrombectomy in ischemic stroke: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2018; 39: 2070–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turk AS, Frei D, Fiorella D, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg 2014; 6: 260–264. [DOI] [PubMed] [Google Scholar]
- 24.Hu YC, Stiefel MF. Force and aspiration analysis of the ADAPT technique in acute ischemic stroke treatment. J Neurointerv Surg 2016; 8: 244–246. [DOI] [PubMed] [Google Scholar]
- 25.Anadani M, Alawieh A, Vargas J, et al. First attempt recanalization with ADAPT: rate, predictors, and outcome. J Neurointerv Surg 2019; 11: 641–645. [DOI] [PubMed] [Google Scholar]
- 26.Delgado Almandoz JE, Kayan Y, Wallace AN, et al. Larger ACE 68 aspiration catheter increases first-pass efficacy of ADAPT technique. J Neurointerv Surg 2019; 11: 141–146. [DOI] [PubMed] [Google Scholar]