Abstract
IgE antibodies (Ab) specific to galactose-α−1,3-galactose (alpha-gal) are responsible for a delayed form of anaphylaxis that occurs 3–6 hours after red meat ingestion. In a unique prospective study of seventy participants referred with a diagnosis of idiopathic anaphylaxis (IA), six (9%) were found to have IgE to alpha-gal. Upon institution of a diet free of red meat, all patients had no further episodes of anaphylaxis. Two of these individuals had indolent systemic mastocytosis (ISM). Those with ISM had more severe clinical reactions but lower specific IgE to alpha-gal and higher serum tryptase levels, reflective of the mast cell burden. The identification of alpha-gal syndrome in patients with IA supports the need for routine screening for this sensitivity as a cause of anaphylaxis, where reactions to alpha-gal are delayed and thus may be overlooked.
Keywords: alpha-galactose, anaphylaxis, clonal, mastocytosis
1 |. INTRODUCTION
Idiopathic anaphylaxis (IA) is a diagnosis of exclusion based on the inability to identify a cause and effect relationship for a given anaphylactic event. Classically, IgE-mediated anaphylaxis to foods occurs within 5–30 minutes after ingestion and is typically protein-based. Nevertheless, recent studies support that IgE-specific antibodies (Ab) to the carbohydrate galactose-α−1,3-galactose (alpha-gal), similar in structure to the B blood group antigen1 and found in multiple tissues of nonprimate mammals,1,2 can induce serious clinical reactions hours after red meat ingestion.3–5 The development of this IgE-specific Ab to alpha-gal is linked to bites from ectoparasitic ticks worldwide and specifically to the Amblyomma americanum in the southeast region of the USA.6 However, due to the delayed nature of the reaction, alpha-gal sensitization may be overlooked in the differential diagnosis of recurrent unexplained anaphylaxis.
Systemic mastocytosis is a clonal mast cell disorder characterized by increased mast cell proliferation and often associated with activating mutations in KIT.7,8 The increased mast cell burden in these patients, clinically followed with serum tryptase levels (sTryp), is thought to result in more severe clinical symptoms in allergic reactions.9 A higher prevalence of venom sensitivity is reported in patients with mastocytosis and,10 although not as common, severe reactions to foods are also reported in this population including reports of alpha-gal sensitivity.11–13
Alpha-gal sensitivity has been reported mainly in adults over 50 years of age with non-B blood types.5,14 In this study, we report the clinical and laboratory characteristics of six patients with alphagal sensitization identified among 70 patients referred with a diagnosis of IA, two of which were found to have a clonal mast cell disorder. In addition, these patients experienced remission of anaphylactic events when red meat ingestion was discontinued.
2 |. MATERIALS AND METHODS
2.1 |. Subjects
Seventy participants (46 females and 24 males; age range 1570 years; median age 48 ± 14.1) with a referral diagnosis of IA were enrolled in the IRB-approved NIH protocol (NCT00719719). Screening this population for IgE to alpha-gal identified six individuals sensitive to the carbohydrate and who thus no longer met the diagnosis of IA. These participants also underwent a bone marrow biopsy and aspirate to determine the presence or absence of a clonal mast cell disorder following accepted consensus criteria.15 All subjects provided informed consent prior to enrollment.
2.2 |. Laboratory studies
2.2.1 |. Serum IgE and tryptase analysis
Total serum IgE level was determined using the Immulite XPI, solidphase chemiluminescence assay (Siemens Medical Solutions, Malvern, PA, USA). IgE levels to pork and beef were measured using a fluoroenzyme immunoassay (Phadia Immuno CAP; courtesy of Platts-Mills laboratory Charlottesville, VA, USA).3 To measure specific IgE, for galactose alpha-1,3-galactose (alpha-gal) we used an assay which employs a monoclonal antibody to cetuximab with a correlation of 0.95 to the commercially available assay in Europe which uses an antibody to beef thyroglobulin.16 Values greater than 0.35 IU/mL were considered positive in both assays. sTryp levels were determined using a commercial fluoro-enzyme immunoassay (Phadia Immuno CAP, Uppsala, Sweden) at CLIA-approved laboratories, and levels above 11.4 ng/mL were considered elevated.
2.3 |. Statistical analysis
Statistical analysis to elucidate correlations between alpha-gal specific IgE and sTryp as well as differences in alpha-gal levels between patients with IA and those with indolent systemic mastocytosis (ISM) was performed using GraphPad PRISM 6.0 software (La Jolla, CA, USA). Given the small sample size and non-Gaussian distribution, data are presented as medians with quartile ranges. Correlations are presented as Spearman r coefficient. Two-tailed P values <.05 are considered statistically significant. Ratios for alpha-gal specific IgE and total serum IgE were calculated to avoid the total IgE concentrations from influencing alpha-gal comparisons.
2.4 |. Results
2.4.1 |. Clinical history
Six male participants (41–70 years) with a non-B blood type had alpha-gal specific IgE Ab above the positive cutoff of 0.35 IU/mL (Table 1). All individuals had histories of tick bites and were residents of five states within the area of the A. americanum or Lone Star tick normal distribution (NJ, MO, VA, TN, and AL, Figure S1). Clinical history revealed that these individuals ingested red meat within 3–6 hours prior to the onset of anaphylaxis. These symptoms included tachycardia, gastrointestinal distress, hives, angioedema, and/or generalized swelling and respiratory compromise. There were no reported reactions to milk or gelatin.
TABLE 1.
Characteristics of patients with antibodies to alpha-gal presented
| IgE IU/mL | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pt. | Diagnosis | Age | Sex | Race | State | Tick bites | Blood type | sTryp ng/mL | Frequency events/year | Total | Alpha-gal | Alpha-gal / IgE ratio | Pork | Beef |
| 1 | IA/ISM | 61 | M | W | VA | Y | O− | 16.3 | 4 | 28.8 | 2.7 | 0.093 | 0.51 | 0.46 |
| 2 | IA/ISM | 70 | M | W | AL | Y | O− | 15.6 | 6 | 28.0 | 1.1 | 0.039 | 0.26 | 0.28 |
| 3 | IA | 55 | M | W | MO | Y | O+ | 3.3 | 6 | 82.6 | 18.8 | 0.227 | 3.0 | 4.5 |
| 4 | IA | 37 | M | W | TN | Y | O+ | 6.4 | 4 | 96.9 | 14.8 | 0.152 | 4.5 | 6.2 |
| 5 | IA | 50 | M | W | NJ | Y | O+ | 4.0 | 5 | 1284 | 218 | 0.169 | 22.3 | 37.5 |
| 6 | IA | 41 | M | W | VA | Y | A− | 4.1 | 12 | 71.2 | 0.36 | 0.005 | 0.10 | 0.10 |
sTryp, serum tryptase.
All patients with delayed anaphylaxis had IgE Ab specific to alpha-gal above 0.35 kUA/L and considered positive (lower limit of detection 0.1 IU/mL).
Two of six patients were found to have ISM (33%). The individuals with ISM experienced symptoms that appeared more severe when compared to patients without a clonal mast cell disorder, including episodes of hypotension and syncope that resulted in visits to an emergency room and hospitalizations. Four patients (1, 3, 4, and 5) had IgE Ab to pork and/or beef above the positive cutoff (>0.35 IU/mL, Table 1) although only symptoms consistent with the delayed anaphylaxis were reported. There was no significant association between the diagnosis of ISM and alpha-gal syndrome.
These patients were subsequently followed for 18 months to 3 years after avoidance of beef, pork, lamb, and venison ingestion. Whereas episodes of anaphylaxis among these patients had ranged from 4 to 12 per year (median 5.5), following institution of the alpha-gal free diet, these individuals experienced no additional episodes of anaphylaxis.
2.4.2 |. Serum IgE and tryptase levels in IA and ISM
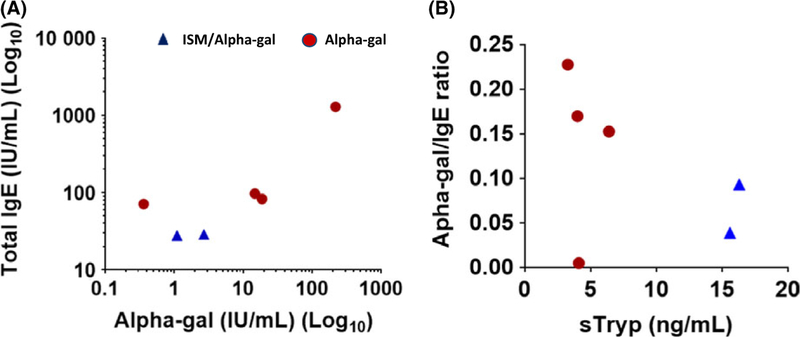
The four individuals with alpha-gal syndrome but no evidence of ISM had total serum IgE (sIgE) levels 2.2-fold higher than those found to have a clonal mast cell disorder (medians of 89.8 and 28.4 IU/mL, respectively; Table S1). Similarly, alpha-gal specific IgE in patients with IA were 7.8-fold higher than those with ISM (medians of 16.8 and 1.9 IU/mL, respectively; Table S1, Figure 1A). The ratio between total sIgE and alpha-gal specific IgE Ab confirmed that correlations were consistent. Excluding patient 6, sTryp negatively correlated with the anti-alpha-gal/IgE ratio (Figure 1B) and reflected the trend of lower IgE levels reported in clonal disease.17
FIGURE 1.
Specific anti-alpha-gal IgE correlation with total IgE and serum tryptase. A, Total IgE vs alpha-gal levels. Patients with co-occurring clonal disease (triangles) tend to have lower levels of both IgE and alpha-gal titers, rs = .77 (B). Alpha-gal/IgE ratios vs serum tryptase (sTryp) levels. There is a trend for positive and negative correlations for figures (A) and (B), respectively. Patients with clonal disease (triangles) had lower alpha-gal/IgE ratios but higher tryptase levels, rs = −.60
3 |. DISCUSSION
This study highlights alpha-gal sensitization as a trigger of unexplained anaphylaxis in patients with or without clonal mast cell disease. This diagnosis was apparently not considered in initial evaluations prior to referral to us because alpha-gal-induced systemic reactions occurred remotely in time relative to ingestion of the provoking food. We suspected the diagnosis-based history, which we confirmed by the presence of alpha-gal specific IgE and resolution of symptoms with an avoidance diet. The resulting message is that IgE to alpha-gal should be determined in patients where the etiology of anaphylaxis remains obscure.
These six individuals presented symptoms between 6:30 PM and 2 AM, usually starting after midnight, which is consistent with alpha-gal syndrome. Patients with mastocytosis had lower levels of both total serum IgE and alpha-gal specific IgE although they experienced more severe clinical symptoms, including hypotension and syncope, not typically reported by patients without clonal disease.3,13 Furthermore, a negative correlation between sTryp, representative of mast cell burden, and anti-alpha-gal IgE/ total IgE ratio was also observed. As reported, these lower IgE levels in patients with mastocytosis appear related to their higher mast cell burden, theoretically resulting in fewer IgE molecules bound per individual mast cell and/or adsorption of most of the circulating IgE.17
All patients with alpha-gal syndrome were male. This observation correlates with previous reports in which men have been shown to be more prone to venom allergies and sensitivities, suggesting that although ingestion of the allergen is necessary, exposure may be more influential in insect-mediated sensitizations.18 This trend can also be seen in other alpha-gal published reports,4,19 but no formal correlation between gender and alpha-gal sensitization has been established.
Four of these six patients were sensitized to beef and pork (IgE levels above 0.35 IU/mL), but showed no symptoms of allergy occurring within 2 hours of eating red meat. A strong correlation between results for alpha-gal, beef, and pork specific IgE antibodies has been reported, suggesting that assays measuring these IgE levels may only be quantifying the alpha-gal component.4 These findings, together with the fact that avoidance of red meat consumption prevented further episodes consistent with alpha-gal syndrome in our patients, demonstrate the need for more specific assays for precise alpha-gal quantification and the need for similar prospective studies involving more patients. We are aware of the occasional discrepancies between the beef thyroglobulin assay used in Europe and the cetuximab-based assay used in this study; however, both assays are reliable and sensitive and results are essentially equivalent.
Due to the structural similarity between alpha-gal and the B blood group, most patients with alpha-gal syndrome have non-B blood types,14 although blood type is not predictive of sensitization. All patients in this study followed this trend, providing further evidence that similarity between these carbohydrates could influence the sensitivity to the alpha-gal epitope.14 Furthermore, it suggests that the development of IgE Ab against the alpha-gal carbohydrate was consistent with current literature highlighting a tick bite history and specific geographic distribution (Figure S1).6 Approximately 1% of all circulating IgGs are directed toward alpha-gal regardless of ABO blood type, but reactions are less common in subjects with B blood type.20
In conclusion, this study shows the importance of including alpha-gal syndrome in the differential diagnosis of anaphylaxis in patients with and without clonal mast cell disease. This identification of alpha-gal syndrome in patients with idiopathic anaphylaxis supports the need for routine screening for this sensitivity as a cause of anaphylaxis, especially when patients live in tick-targeted geographic areas and reactions are delayed and thus not associated with food ingestion shortly before the anaphylaxis event.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the Division of Intramural Research of NIAID. The authors also thank Erica Brittain, PhD, Mathematical Statistician at the NIH Division of Clinical Research and David Liewehr Statistician of the Center for Cancer Research Biostatistics and Data Management Section for their insight in statistical analysis.
Funding information
Supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health
Footnotes
CONFLICTS OF INTEREST
Dr. Lieberman reports personal fees from kaleo, personal fees from mylan, outside the submitted work; Dr. Platts-Mills reports grants from Thermo Fisher Scientific/Phadia, outside the submitted work; The other authors declare no conflict of interest.
SUPPORTING INFORMATION
Additional Supporting Information may be found online in the supporting information tab for this article.
REFERENCES
- 1.Macher BA, Galili U. The Galalpha 1,3Galbeta1,4GlcNAc-R (alphaGal) epitope: a carbohydrate of unique evolution and clinical relevance. Biochim Biophys Acta. 2008;1780:75–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spiro RG, Bhoyroo VD. Occurrence of alpha-D-galactosyl residues in the thyroglobulins from several species. Localization in the saccharide chains of the complex carbohydrate units. J Biol Chem. 1984;259:9858–9866. [PubMed] [Google Scholar]
- 3.Commins SP, Satinover SM, Hosen J, et al. Delayed anaphylaxis, angiodema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-a-1,3-galactose. J Allergy Clin Immunol. 2009;123:426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kennedy JL, Stallings AP, Platts-Mills TA, et al. Galactose-alpha-1,3galactose and delayed anaphylaxis, angioedema, and urticaria in children. Pediatrics. 2013;131:e1545–e1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Platts-Mills TA, Schuyler AJ, Hoyt AE, Commins SP. Delayed anaphylaxis involving IgE to galactose-alpha-1,3-galactose. Curr Allergy Asthma Rep. 2015;15:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Commins SP, James HR, Kelly LA, et al. The relevance of tick bitesto the production of IgE antibodies to the mammalian oligosaccharide galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2011;127:1286–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valent P, Escribano L, Broesby-Olsen S, et al. Proposed diagnosticalgorithm for patients with suspected mastocytosis: a proposal of the European Competence Network on Mastocytosis. Allergy. 2014;69:1267–1274. [DOI] [PubMed] [Google Scholar]
- 8.Horny H, Atkin C, Metcalfe D, et al. Mastocytosis In: Swedlow S,Campo E, Harris N, Jaffe E, Pileri S, Stein H, Thiele J, Vardiman J, eds. World Health Organization (WHO) Classification of Tumours. Lyon, France: IARC Press; 2008: 54–63. [Google Scholar]
- 9.Brockow K, Jofer C, Behrendt H, Ring J. Anaphylaxis in patients withmastocytosis: a study on history, clinical features and risk factors in 120 patients. Allergy. 2008;63:226–232. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez de Olano D, de la Hoz Caballer B, Nunez Lopez R, et al. Prevalence of allergy and anaphylactic symptoms in 210 adult and pediatric patients with mastocytosis in Spain: a study of the Spanish network on mastocytosis (REMA). Clin Exp Allergy. 2007;37:1547–1555. [DOI] [PubMed] [Google Scholar]
- 11.Brady S, Novack D, Kulczyzki AJ. Recurrent anaphylaxis due todelayed allergy to mammalian meat in a patient with mastocytosis. J Allergy Clin Immunol. 2015;1:AB206. [Google Scholar]
- 12.Prieto-García A, Alvarez-Perea A, Matito A, et al. Systemic mastocytosis presenting as IgE-mediated food-induced anaphylaxis: a report of two cases. J Allergy Clin Immunol Pract. 2015;3:456–458. [DOI] [PubMed] [Google Scholar]
- 13.Roenneberg S, Bohner A, Brockow K, et al. Alpha-Gal-a new clue for anaphylaxis in mastocytosis. J Allergy Clin Immunol Pract. 2016;4:531–532. [DOI] [PubMed] [Google Scholar]
- 14.Platts-Mills TA, Schuyler AJ, Tripathi A, Commins SP. Anaphylaxis to the carbohydrate side chain alpha-gal. Immunol Allergy Clin North Am. 2015;35:247–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valent P, Akin C, Arock M, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157:215–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chung CH, Mirakhur B, Chan E, et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-a-1,3-galactose. N Engl J Med. 2008;358:1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Müller U, Helbling A, Hunziker T, et al. Mastocytosis and atopy: a€ study of 33 patients with urticaria pigmentosa. Allergy. 1990;45:597603. [DOI] [PubMed] [Google Scholar]
- 18.Perez Pimiento AJ, Prieto Lastra L, Rodriguez Cabreros MI, VasquezBautista AA, Garcia Cubero A, Calvo Manuel E. Systemic reactions to wasp sting: is the clinical pattern related to age, sex and atopy? Allergol Immunopathol (Madr). 2007;35:10–14. [DOI] [PubMed] [Google Scholar]
- 19.Hilger C, Fischer J, Swiontek K, et al. Two galactose-alpha-1,3-galactose carrying peptidases from pork kidney mediate anaphylactogenic responses in delayed meat allergy. Allergy. 2016;71:711–719. [DOI] [PubMed] [Google Scholar]
- 20.Rispens T, Derksen NI, Commins SP, Platts-Mills TA, Aalberse RC.IgE production to alpha-gal is accompanied by elevated levels of specific IgG1 antibodies and low amounts of IgE to blood group B. PLoS One. 2013;8:e55566. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.