Abstract
Social anxiety typically emerges by adolescence and is one of the most common anxiety disorders. Many clinicians and researchers utilize the Screen for Child Anxiety Related Disorders (SCARED) to quantify anxiety symptoms, including social anxiety, throughout childhood and adolescence. The SCARED can be administered to both children and their parents, though reports from each informant tend to only moderately correlate. Here, we investigated parent–child concordance on the SCARED in a sample of adolescents (N = 360, Mage = 13.2) using a multi-trait multi-method (MTMM) model. Next, in a selected sample of the adolescents, we explored relations among child report, parent report, and latent social anxiety scores with two laboratory tasks known to elicit signs of social anxiety in the presence of unfamiliar peers: a speech task and a “Get to Know You” task. Findings reveal differences in variance of the SCARED accounted for by parent and child report. Parent report of social anxiety is a better predictor of anxiety signs elicited by a structured speech task, whereas child report of social anxiety is a better predictor of anxiety signs during the naturalistic conversation with unfamiliar peers. Moreover, while latent social anxiety scores predict both observed anxiety measures, parent report more closely resembles latent scores in relation to the speech task, whereas child report functions more similarly to latent scores in relation to the peer conversation. Thus, while latent scores relate to either observed anxiety measure, parent and child report on the SCARED each provide valuable information that differentially relate to naturalistic social anxiety-related behaviors.
Keywords: Anxiety, SCARED, Child report, Parent report, Social anxiety
Social anxiety (SA), which affects about 12% of the population (Kessler et al. 2005), involves excessive fear of negative judgment (Erath et al. 2007; Mancini et al. 2005). Social anxiety symptoms typically first manifest in early adolescence, when social interactions and peer scrutiny become prominent (Kessler et al. 2005). These symptoms are typically assessed using self- and parent-report measures.
One of the most frequently used screening measures in children and adolescents is the Screen for Child Anxiety-Related Emotional Disorders (SCARED; Birmaher et al. 1997, 1999). The SCARED consists of 41items presented on a 3-point likert scale, which is designed to assess SA, as well as four other subtypes of anxiety: panic disorder, general anxiety, separation anxiety, and school avoidance (along with a “total anxiety” score). The SA subscale is frequently used to measure SA symptoms in adolescent populations (Bailey et al. 2006; Chronis-Tuscano et al. 2009; Lahat et al. 2014; Muris 2002; blinded for review) and is the focus of the current report. Previous work has established the factor structure of the subscales of anxiety measured by the SCARED (Birmaher et al. 1997, 1999) and validated the questionnaire’s ability to quantify anxiety symptoms in adolescent populations based on either child (self) or parent report (Birmaher et al. 1997, 1999; Dirks et al. 2014). The SCARED shows good internal consistency for both the parent and child versions (α = 0.90; Birmaher et al. 1999), and both versions differentiate anxious from healthy children (Rappaport et al. 2017), and children with anxiety diagnoses from children with depression diagnoses or disruptive disorders (Birmaher et al. 1999). Moreover, the instrument demonstrates good convergent validity with other self-report measures of anxiety (e.g. CBCL and STAIC; Monga et al. 2000), as well as clinician ratings (Behrens et al. 2018; Cosi et al. 2010).
The SCARED generally shows only moderate correlations between child and parent report scores, especially for the SA subscale (Behrens et al. 2018; Birmaher et al. 1997, 1999; Cosi et al. 2010; Dirks et al. 2014; Rappaport et al. 2017), and partial measurement invariance between reporters (Olino et al. 2018). These findings align with data demonstrating weak to moderate correlations between child and parent report of internalizing problems like anxiety (Langer et al. 2010) and depression (Kazdin et al. 1983; Moretti et al. 1985). Sophisticated statistical techniques provide relatively unexplored avenues for extending traditional correlational examinations of informant discrepancy by allowing for the parsing of unique and shared variance in parent-child informant pairs.
Multi-trait multimethod (MTMM) confirmatory factor analysis (CFA) (Maas et al. 2009; Marsh and Bailey 1991) provides a novel means for examining differences in child and parent report of anxiety symptoms from the SCARED. The MTMM approach simultaneously models latent trait (e.g., symptoms) and method (e.g., reporter) factors to partition trait (shared), method (unique), and error (unique) variance. MTMM tests for a reporter effect by determining whether the correlation between child report and parent report differs from 1.0, after accounting for trait and error variance, and evaluates measurement bias by comparing estimates of method and trait variance (Maas et al. 2009). Additionally, MTMM analyses provide factor scores for each individual and for each latent trait. These “pure” scores index a latent construct comprised of shared trait variance from each reporter. Importantly, these scores are free of measurement error or informant-related differences, which are included in more common correlational analyses of informant agreement and could bias results when attempting to examine differences in reporting of trait levels. Therefore, the MTMM framework can both identify unique variance associated with informant discrepancies (i.e., child vs parent) and shared variance by estimating latent traits of interest (i.e., for the social anxiety subscale) based on multiple reporters.
Informant discrepancies especially challenge researchers and clinicians seeking to understand how psychopathology manifests in different situations (De Los Reyes 2011; De Los Reyes et al. 2013), but also provide an important avenue to explore how we can utilize information from various informants to understand context-dependent expressions of psychopathology. Specifically for social anxiety, previous work has explored how different informant’s ratings of social anxiety relate to one rating of observed anxiety behavior. Child ratings of social phobia (SASC-R; Social Anxiety Scale for Children-Revised) relate to coded observed anxiety during a read aloud task in third to fifth graders, while parent and teacher ratings did not (Beidel et al. 2000). Informant discrepancies may be due to a lack of knowledge of the symptomology, as adolescents have explicitly attributed their parents’ lack of endorsement of social anxiety symptoms to the fact that they do not always share their inner feelings with their parents (Bidaut-Russell et al. 1995). When considering how child self-report only relates to real-world behaviors in different contexts, child report on the SPAI (Social Phobia and Anxiety Inventory) correlated with observed anxiety in a social interaction with peers during a role play task, but not during a structured read aloud task (DiBartolo and Grills 2006). Thus, report of SA symptoms may vary by both the informant and the context (naturalistic vs structured) in which social anxiety manifests; however, there is a lack of information exploring how both parent and child informants relate to social anxiety in different social contexts. The current study contributes an important consideration for clinicians by being the first to explore unique and shared variance of parent and child report of social anxiety, using an MTMM model of the commonly-used SCARED questionnaire, and to examine how both of these informant reports relate to real-world behaviors in two different contexts: a speech task with a controlled prompt and a realistic conversation with unfamiliar peers. The latter analyses specifically evaluate the presence of context-dependent relations between informant reports of SA on the SCARED and observable signs of SA.
The goals of this investigation were threefold. First, we sought to empirically determine if child and parent report on the SCARED differ using a MTMM framework. Second, we used observed signs of SA in two distinct contexts to test convergent validity of parent and child social anxiety SCARED scores. Third, we examined whether a latent SA factor derived from both reporters in the MTMM model and “free” from measurement- and informant-related error would also predict context-dependent observed SA signs, as compared to child or parent report alone. Within the MTMM, we hypothesized that child and parent report would be quantitatively distinct, even after accounting for error variance. Second, we predicted that parent and child scores of SA on the SCARED would map onto SA in different contexts. We also anticipated that factor scores of SA derived from the MTMM, reflective of shared variance, would correlate with both observed measures of SA, removing the nuance of the unique variance that each reporter can contribute.
Method
Participants
Participants from the greater Washington, D.C. metropolitan area were recruited as part of a longitudinal study examining socioemotional functioning across child development (Hane et al. 2008). At four months of age, 779 infants completed an in-lab temperament screening, during which emotional and motor reactivity to novel stimuli were observed (Fox et al. 2001). Subsequently, 291 infants (134 male) were selected to continue in the study based on in-lab temperament observations. Children were selected based on their affect (positive and negative) and motor responses to novel stimuli in order to identify children with distinct temperamental reactivity patterns (Fox et al. 2001). This selected, longitudinal sample continued to participate in assessments of socio-emotional development at 9 months, 2, 3, 4, 5, 7, 10, and 12 years.
For this study, data from the 12-year visit was used, for which 192 adolescents from our selected, longitudinal sample of 291 infants provided SCARED data on either the self-report, parent-report, or both. In addition to our selected sample, 168 adolescents from a community sample of 436 children, who served as “unfamiliar peers” in a number of observed social situations in the laboratory, provided self-report and/or parent-report data rating their own anxiety symptoms on the SCARED. In total, an intersection of 360 participants provided some data (either some child-report, some parent-report, or some data for both) with 353 children and 328 parents providing SCARED data. There were no differences in gender, mother’s race, or maternal education, all ps > 0.4, for participants who provided SCARED data compared to participants who did not have SCARED data. The University of Maryland Institutional Review Board approved all recruitment and study procedures; parents provided informed consent and all adolescents provided assent.
Screen for Child Anxiety Related Emotional Disorders (SCARED)
Participants and their parent completed the SCARED questionnaire (Birmaher et al. 1997, 1999) at the 12-year assessment. The SCARED is a 41-item parent and child questionnaire assessed using a 3-point Likert scale (0 = almost never, 1 = sometimes, 2 = often). Although a 3-point response scale provides challenges for statistical modelling, such as non-continuous data requiring specialized estimators (Finney & DiStefano, 2013), a Likert scale with only 3 responses is beneficial for younger participants as more limited response options make it easier for them to choose a response without affecting reliability or validity (Matell and Jacoby 1971). Parent and child responses on the SCARED are separately summed to create composites reflecting: total anxiety and five subscale scores (panic disorder, separation anxiety, school avoidance, general anxiety, and social anxiety). The total anxiety composite reflects a sum of all response items, whereas each subscale reflects a sum of particular items addressing relevant symptoms within each subscale. Total and subscale scores were calculated by summing scores and prorating based on how many questions were complete (separately for total and for each subscale). Scores for participants with less than 80% of the questions complete for that score were considered missing. Our sample was not a clinical sample, but, for total child SCARED scores (Meanchild = 18.56, SDchild = 11.76), 92 out of 342 (26.9%) participants reached clinical cutoffs (≥25) and, for total parent SCARED scores (MeanParent = 9.30, SDParent = 8.45), 17 out of 319 (5.3%) reached clinical cutoffs (≥25).
Get to Know you (GTKY) Task
At the 12-year assessment, participants were seated with the unfamiliar peer and that peer’s friend and introduced to one another by a researcher. The participants were left alone in the room and given the opportunity to speak with one another for two minutes. Because this task served as the introduction of the target adolescent to the novel peers participating in the visit, it was always performed first. The participants’ behaviors were video recorded and coded by trained coders. Using a coding system developed by Henderson and colleagues (see Usher et al., 2015 for more information), two behaviors were rated globally on a scale of 1 “completely inappropriate” to 5 “totally appropriate”: openness to interaction (e.g., eye contact in relation to peer, physical orientation in relation to peer) and appropriateness of conversation (e.g., flow of conversation, information seeking from peer). One behavior, social ease during interaction, was rated globally on a scale of 1 “uncomfortable” to 5 “totally comfortable” based on affect and behavior. The amount of time until the participant made their first spontaneous utterance and the percentage of time they spoke were recorded. The number of times that the participant shared information about themselves and the number of times they sought information from others through questions were also recorded. A graduate student served as the primary coder, who trained a team of two undergraduates to achieve reliability. Reliability estimates were excellent and ICCs ranged from 0.89–0.98 for the GTKY measures (see Supplementary Table 3 for descriptive statistics). The graduate student primary coder and two undergraduates then overlapped on approximately 20% of the sample. Where appropriate, coded variables were reverse-coded, such that a higher number would relate to greater anxiety. Exploratory factor analysis suggested a single-factor solution, supporting construction of a single composite measure. All measures were Z-scored and averaged into a composite reflecting anxiety during GTKY (α = 0.90).
Speech Task
Participants then completed a modified version of the Trier Social Stress Test at the 12-year visit (Kirschbaum et al. 1993). Participants were told they have two minutes to prepare a five-minute speech on the topic of “What makes you a good leader?” They were told that they would present their speech to the unfamiliar peers and two research assistants while being video recorded. The participants were allowed to seek and/or receive help from the unfamiliar peer(s) when preparing. Although the participants were told that the speech needed to be five minutes long, the researcher ended the task after two minutes. If the participant stopped speaking before two minutes, they were prompted to “please continue” by the researcher. The following behaviors were rated globally (throughout the speech) on a scale from 1 “Not at all” to 5 “Very”: verbal anxiety/nervousness (e.g., nervous laughter, mumbling, stopping talking), physical anxiety/nervousness (e.g., scowling, fidgeting), and effectiveness of speech content (e.g., if transcribed, would it be a good speech). Additionally, the total length of the speech and the percentage of time that the participant spoke during the task were recorded. A graduate student served as the primary coder, who trained a team of two undergraduates to achieve reliability. Reliability estimates were excellent and ICCs ranged from 0.89–0.99 for the speech measures (see Supplementary Table 3 for descriptive statistics). The graduate student primary coder and two undergraduates then overlapped on approximately 20% of the sample. Exploratory factor analysis suggested a single-factor solution for all five measures. Each measure was z-scored and averaged into a composite reflecting anxiety during the speech task (α = 0.80).
Statistical Approach
Multitrait-Multimethod Model to Assess Meaningful Differences in Child and Parent Report
A multi-trait multimethod (MTMM) confirmatory factor analysis (CFA) model was conducted to test informant disagreement between parent and child report on the SCARED. Participants from both the selected sample and the community sample were included in the model if they had completed some data on child or parent SCARED, or both, during the 12-year assessment. Table 1 describes the demographic information for the participants included in the MTMM model.
Table 1.
Sample Demographics for Participants Included in the MTMM
| Selected Sample N = 192 |
Community Sample N = 168 |
|
|---|---|---|
| Age (Years) | 13.2 (0.65) | 13.1 (0.57) |
| Sex (Female) | 101 (52.6%) | 89 (52.9%) |
| Mother’s Education Level | ||
| High School Graduate | 26 (13.5%) | 15 (8.9%) |
| College Graduate | 76 (41.1%) | 71 (40.0%) |
| Graduate Degree | 74 (38.5%) | 74 (44.0%) |
| Other | 15 (7.8%) | 7 (4.2%) |
| Unknown | 1 (0.5%) | 1 (0.6%) |
| Race/Ethnicity | ||
| African American | 28 (14.5%) | 42 (25.0%) |
| Asian | 5 (2.6%) | 9 (5.4%) |
| Caucasian | 135 (70.3%) | 99 (5.9%) |
| Hispanic | 10 (5.2%) | 11 (6.5%) |
| Other | 4 (2.1%) | 5 (3.0%) |
| Unknown | 10 (5.2%) | 2 (1.2%) |
| Child SCARED Social Anxiety | 4.94 (3.58) | 4.73 (3.43) |
| Parent SCARED Social Anxiety | 3.82 (3.45) | 2.93 (2.86) |
| “Get to Know You” Task (N = 153) | 0.05 (0.78) | – |
| Speech Task (N = 145) | 0.11 (0.81) | – |
Data presented as Frequency (%) or Mean (SD)
SCARED SA subscale scores reported above only include children who had 80% of the data available (see missing data handling for more info; Selected sample: Child SCARED SA, N = 176, Parent SCARED SA, N = 169; Community Sample: Child SCARED SA, N = 162, Parent SCARED SA, N = 150)
We conducted the MTMM model using MPlus Version 8 (Muthén & Muthén, 2010). Five trait (the five anxiety subscales) and two method (parent- and child-report) latent variables were specified (Fig. 1). The single items from both the parent and child SCARED that are summed to create the subscale scores served as the indicator variables for the latent traits. Method factors were modeled as latent variables with parent items as the indicator variables for the parent factor and child items as the indicator variables for the child factor. The model allows trait factors to correlate and allows method factors to correlate. However, correlations between trait factors and method factors were constrained to zero (Marsh and Bailey 1991). Variances of the latent variables were constrained to be one in order to assign units to the factor by standardizing it.
Fig. 1.
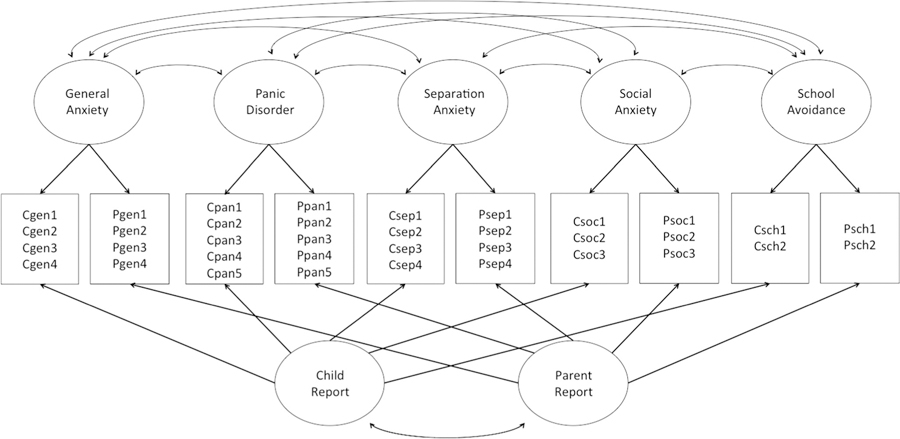
Path Diagram for MTMM model. Variances of the latent factors were set to one. Traits were allowed to covary and method factors were allowed to covary; however, covariance between trait factors and method factors were set to zero. Parceled items were used as manifest variables
However, using the single items of the SCARED as indicator variables proved to be a problem. SCARED items are ordinal with only 0, 1, or 2 as acceptable responses. Such a limited response range creates a lack of variance in responses and results in empty cells when examining covariance between two single items. Therefore, we collapsed, or “parceled” the single items to create composites in order to increase response variance. Detailed in Supplementary Table 1, we parceled single items that fall under the same subscale based on item content and item variance (e.g. items with low variance were grouped with related items with higher variance). Parceling is an acceptable solution for preventing empty cells between categorical responses (Little et al. 2002). These parceled items served as the final indicator variables for the latent factors as described above.
The robust weighted least squares estimator (WLSMV) for categorical data was used. The WLSMV estimator does not assume normally distributed variables (Brown 2006). The data are considered missing at random (MAR) because we do not believe that the missingness of the data is related to anxiety levels. Therefore, full information maximum likelihood (FIML) estimation was used to estimate missing data.
Model fit was determined using the Comparative Fit Index (CFI) and the Root-Mean-Square Error of Approximation (RMSEA). CFI values greater than 0.95 and RMSEA values below 0.06 suggest a good fit of the model with the data (Cheung and Rensvold 2002). In order to accomplish our first goal of determining if child and parent report differ, we tested whether 1 – (the correlation between the two latent trait factors) is statistically different from zero.
Convergent Validity of Parent and Child SCARED Social Anxiety with Observed Anxiety
Next, we examined the convergent validity of child and parent reported SA on the SCARED with two observed SA composites during the speech and the GTKY. To do this, we employed hierarchical multiple regression. The regression analyses included only selected participants with SCARED data and speech (N = 130) and with SCARED data and GTKY (N = 138). Only the selected participants from the longitudinal study were included in the following speech and GTKY regression analyses in order to eliminate triad-level dependencies (e.g. GTKY and speech performance of the community participants would not be independent from the selected participants because they participated in these tasks together) and to mitigate order effects of speech presentation (e.g. selected participants always presented their speech first). There were no differences in gender, Χ2(1,N = 291) = 0.22, p = 0.64, mother’s race, Χ2(4,N = 290) = 3.18, p = 0.53, maternal education, Χ2(3,N = 289) = 1.59, p = 0.66, between the longitudinal participants who had GTKY data (N = 153) and the longitudinal participants who did not have GTKY data (N = 138). Similarly, there were no differences in gender, Χ2(1,N = 291) = 0.59, p = .44, mother’s race, Χ2(4,N = 290)= 1.86, p = 0.76, or maternal education, Χ2(3,N = 289) = 4.14, p = 0.25, between the longitudinal participants who had Speech data (N = 145) and the longitudinal participants who did not have Speech data (N = 146). There were also no differences in child or parent SA scores for those who completed the GTKY compared to those who did not, p’s > .4, or for those who completed the speech compared to those who did not, p’s > 0.4.
While age was unrelated to either child or parent report on the SCARED (ps > 0.10), females had higher parent report (t = −2.36, p = 0.02), and child report (t = −4.04, p < 0.001) of SA. Thus, our first block of the regression included gender alone. In the second block, child report SCARED was added and R2 change was assessed. In the final block, parent report SCARED was added and R2 change was evaluated. Then, we reversed the order so that parent report was added in the second block and child report was added in the third block.
Relations between Latent Scores and Observed Anxiety Variables Compared to Traditional Child and Parent Measures
To address our third aim, we examined convergent validity between the latent factor of SA (with the reporter and error variance removed) and observed measures of SA. Factor scores for the SA subscale for each participant were extracted from MPlus. This approach compared the correlation between observed anxiety and the latent factor scores, which should reflect only shared social anxiety variance as compared to using parent or child report alone. To assess convergent validity of these factor scores, we correlated the SA factors scores with both the speech and GTKY.
Females had higher factor scores of SA (t = −2.14, p = 0.034), while age was unrelated to factor scores of social anxiety for those included in the MTMM, r(332) = −0.012, p = 0.82). Therefore, we controlled for gender when calculating partial correlations between: SA factor scores-observed SA, child report SCARED SA-observed SA, and parent report SCARED SA-observed SA. Listwise deletion was used for these partial correlations to include only those who completed, first, both child and parent report SCARED and the speech task (N = 127), and second, both child and parent report SCARED and the GTKY task (N = 135). Next, we used an r-to-z test to formally test differences in the partial correlations between these factor scores and observed SA, as well as child or parent report and observed SA. Because the correlations compared in our r-to-z test share one variable in common, we used the r-to-z test of the difference between two dependent correlations (Lee & Preacher, 2013). Supplementary analyses (see the online supplementary material) also explored if relations between latent scores and observed anxiety differed from relations between averaging child and parent scores and observed anxiety because some researchers use this average approach in an attempt to reflect shared variance (Bourdon et al. 2019; Buzzell et al. 2017; Lahat et al. 2014; Lau et al. 2008; Roy et al. 2013; Shechner et al. 2014).
Results
MTMM Model: Child Vs Parent Report
The MTMM model showed good fit, CFI = 0.968, RMSEA = 0.032, 90% CI [0.026 0.038]. Table 2 shows the correlations between the latent trait variables. The mean and range of the factor loadings for each latent factor are as follows: panic disorder M = 0.33 (−0.05 to 0.67), general anxiety M = 0.19 (−0.20 to 0.61), social anxiety M = 0.61 (0.56 to 0.67), separation anxiety M = 0.43 (0.04 to 0.66), school avoidance M = 0.43 (0.35 to 0.52), child report M = 0.59 (0.34 to 0.83), and parent report M = 0.64 (0.47 to 0.94). Table 3 partitions variance in each indicator variable attributable to trait, method, and unique factors. Notably, each indicator variable displayed evidence of measurement bias, expressed as moderate variance attributable to method.
Table 2.
Correlations between Latent Trait Factors
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. General Anxiety | ||||
| 2. Panic Disorder | −0.09 | |||
| 3. Separation Anxiety | −0.05 | 0.37** | ||
| 4. Social Anxiety | 0.17 | 0.05 | 0.22** | |
| 5. School Avoidance | −0.01 | 0.43** | 0.24* | −0.05 |
p < .05
p < .01
Table 3.
Information about Indicator Variables Used in 12-Year MTMM Model
| Variable | N (included in Mean and SD) | Mean | SD | Total Variance Explained | Variance Explained from Trait | Variance Explained from Method | Unique Variance |
|---|---|---|---|---|---|---|---|
| CPan1 | 353 | 1.32 | 1.04 | 0.75 | 37.43% | 31.35% | 31.22% |
| CPan2 | 353 | 0.77 | 0.99 | 0.75 | 29.76% | 41.72% | 28.52% |
| CPan3 | 353 | 0.55 | 1.02 | 0.78 | 57.75% | 27.82% | 14.44% |
| CPan4 | 353 | 0.71 | 0.88 | 0.76 | 13.95% | 40.69% | 45.36% |
| CPan5 | 351 | 0.39 | 0.79 | 0.78 | 18.31% | 66.97% | 14.72% |
| CGen1 | 353 | 1.11 | 1.12 | 0.79 | 1.25% | 86.70% | 12.05% |
| CGen2 | 350 | 1.48 | 1.16 | 0.77 | 4.41% | 78.24% | 17.35% |
| CGen3 | 352 | 1.51 | 1.24 | 0.75 | 5.12% | 63.65% | 31.23% |
| CGen4 | 353 | 1.61 | 1.52 | 0.76 | 0.32% | 77.40% | 22.28% |
| CSoc1 | 353 | 1.42 | 1.15 | 0.76 | 40.78% | 38.61% | 20.61% |
| CSoc2 | 353 | 2.05 | 1.63 | 0.83 | 40.61% | 53.55% | 5.84% |
| CSoc3 | 348 | 1.37 | 1.21 | 0.78 | 41.40% | 44.07% | 14.54% |
| CSep1 | 352 | 0.80 | 0.99 | 0.75 | 17.17% | 40.38% | 42.45% |
| CSep2 | 353 | 0.29 | 0.64 | 0.76 | 56.16% | 24.54% | 19.30% |
| CSep3 | 353 | 0.93 | 0.96 | 0.76 | 35.13% | 14.69% | 50.17% |
| CSep4 | 351 | 0.78 | 0.88 | 0.75 | 27.81% | 46.30% | 25.90% |
| CSch1 | 353 | 0.35 | 0.79 | 0.76 | 35.04% | 43.37% | 21.59% |
| CSch2 | 353 | 1.10 | 1.01 | 0.75 | 30.52% | 30.26% | 39.22% |
| PPan1 | 328 | 0.40 | 0.62 | 0.77 | 2.05% | 42.08% | 55.87% |
| PPan2 | 328 | 0.21 | 0.56 | 0.75 | 8.33% | 57.69% | 33.98% |
| PPan3 | 328 | 0.11 | 0.42 | 0.80 | 17.32% | 73.07% | 9.61% |
| PPan4 | 328 | 0.10 | 0.34 | 0.90 | 0.28% | 98.38% | 1.34% |
| PPan5 | 327 | 0.12 | 0.45 | 0.83 | 8.40% | 85.87% | 5.73% |
| PGen1 | 328 | 0.73 | 1.01 | 0.52 | 17.15% | 82.85% | 0.00% |
| PGen2 | 327 | 0.70 | 0.82 | 0.82 | 45.32% | 47.58% | 7.10% |
| PGen3 | 327 | 0.85 | 0.91 | 0.78 | 26.52% | 59.94% | 13.53% |
| PGen4 | 328 | 1.05 | 1.20 | 0.78 | 21.50% | 64.42% | 14.08% |
| PSoc1 | 328 | 0.97 | 1.05 | 0.78 | 58.08% | 28.21% | 13.71% |
| PSoc2 | 328 | 1.45 | 1.36 | 0.86 | 52.75% | 44.48% | 2.76% |
| PSoc3 | 327 | 0.95 | 1.02 | 0.77 | 53.18% | 28.74% | 18.08% |
| PSep1 | 327 | 0.20 | 0.51 | 0.76 | 0.22% | 56.05% | 43.73% |
| PSep2 | 328 | 0.25 | 0.64 | 0.80 | 54.85% | 36.14% | 9.00% |
| PSep3 | 328 | 0.33 | 0.70 | 0.76 | 26.65% | 50.15% | 23.20% |
| PSep4 | 327 | 0.30 | 0.57 | 0.77 | 11.88% | 33.12% | 55.00% |
| PSch1 | 328 | 0.14 | 0.44 | 0.80 | 15.09% | 75.62% | 9.29% |
| PSch2 | 328 | 0.40 | 0.66 | 0.76 | 20.58% | 33.36% | 46.06% |
To determine if child and parent report empirically differ on the SCARED, we examined the correlation between child and parent report method factors. The child report method factor and parent report method factor were again moderately, positively correlated, r = 0.45, p < 0.001. However, we then tested whether the correlation between the child report method factor and parent report method factor differed from a perfect correlation value of one by subtracting this correlation coefficient from one (1–.45 = 0.55) and testing if the difference was significantly different from zero. We found evidence of discriminant validity between child and parent report, as their correlation was different from a correlation of one, z = 10.92, p < 0.001.
Convergent Validity of Social Anxiety SCARED Scores with Observed Anxiety
Given that child and parent report differed, we compared the ability of child- and parent-report of SA to predict observed SA. As shown in Table 4, the results from the regression model revealed that parent-report but not child-report significantly predicted child’s observed anxiety in the speech task. On the other hand, as shown in Table 5, when evaluating how child compared to parent report explains variance in SA during the GTKY task, child-report but not parent-report significantly predicted child’s observed anxiety in the GTKY task.
Table 4.
Hierarchical Multiple Regression Analysis Predicting Speech Task
| Variable | β | ΔF | dfs | ΔR2 |
|---|---|---|---|---|
| Block 1 | 0.36 | 1, 128 | 0.003 | |
| Gender | 0.05 | |||
| Block 2 | 1.10 | 1, 127 | 0.009 | |
| Gender | 0.02 | |||
| Child Report | 0.10 | |||
| Block 3 | 8.28** | 1, 126 | 0.061** | |
| Gender | −0.01 | |||
| Child Report | 0.00 | |||
| Parent Report | 0.07** | |||
| Block 1 | 0.36 | 1, 128 | 0.003 | |
| Gender | 0.05 | |||
| Block 2 | 9.52** | 1, 127 | 0.07** | |
| Gender | −0.01 | |||
| Parent Report | 0.27** | |||
| Block 3 | 0.00 | 1, 126 | 0.00 | |
| Gender | −0.01 | |||
| Parent Report | 0.27** | |||
| Child Report | 0.00 |
p < 0.05
p < 0.01
Table 5.
Hierarchical Multiple Regressions Predicting GTKY Task
| Variable | β | ΔF | dfs | ΔR2 |
|---|---|---|---|---|
| Block 1 | 1.66 | 1, 136 | 0.012 | |
| Gender | −0.11 | |||
| Block 2 | 9.69** | 1, 135 | 0.066** | |
| Gender | −0.21* | |||
| Child Report | 0.28* | |||
| Block 3 | 2.15 | 1, 134 | 0.015 | |
| Gender | −0.22* | |||
| Child Report | 0.22* | |||
| Parent Report | 0.14 | |||
| Block 1 | 1.66 | 1, 136 | 0.012 | |
| Gender | −0.11 | |||
| Block 2 | 6.44* | 1, 135 | 0.045* | |
| Gender | −0.16 | |||
| Parent Report | 0.22* | |||
| Block 3 | 5.28* | 1, 134 | 0.036* | |
| Gender | −0.34* | |||
| Parent Report | 0.03 | |||
| Child Report | 0.05* |
p < 0.05
p < 0.01
Convergent Validity of Child and Parent SCARED Scores as Compared to Latent Social Anxiety with Observed Anxiety
Next, we investigated how correlations between the factor scores from the latent SA factor and observed measures of SA (i.e., speech and GTKY) compared to correlations between either child report or parent report on the SCARED and the observed measures of SA. Table 6 details the correlation coefficients for these relations. The correlation coefficient for the factor scores and the speech task and the coefficient for parent report and the speech task did not differ, Z = −0.047, p = 0.96. However, the coefficient for child report and the speech task did differ significantly from the coefficient for factor scores and the speech task, Z = 2.41, p = 0.015.
Table 6.
Convergent Validity of Observed Anxiety with Reported Anxiety
| Reported Anxiety | Speech Task (N = 127) |
|---|---|
| Latent Scores | 0.261** |
| Child SCARED SA | 0.093 |
| Parent SCARED SA | 0.264** |
| Average SCARED SA | 0.216* |
| Reported Anxiety | GTKY Task (N = 135) |
| Latent Scores | 0.321** |
| Child SCARED SA | 0.259** |
| Parent SCARED SA | 0.213* |
| Average SCARED SA | 0.283* |
p < 0.05
p < 0.01
For the GTKY task, the correlation coefficient for the factor scores and GTKY and the coefficient for parent report and GTKY did marginally differ, Z = 1.723, p = 0.08. In contrast, the coefficient for child report and GTKY did not significantly differ from the coefficient for factor scores and GTKY, Z = 0.958, p = 0.33. These results provide further evidence that parent and child reports contribute unique information as they map onto different social contexts, as compared to the shared trait variance of the latent factors, which does not differentiate between contexts.
Discussion
Researchers and clinicians frequently measure adolescent social anxiety (SA) symptoms using the SCARED SA subscale from both parent and child reporters. Previous work has shown that parent and child report on questionnaires frequently differ (De Los Reyes et al. 2015; De Los Reyes and Kazdin 2005), and here, we demonstrate that these differences in parent and child report are also present in the SCARED. Specifically for the SA subscale measured by the SCARED, child and parent report differentially related to observed SA in different contexts. Using a latent trait approach or a simple average, with information from both reporters, correlated with both observed measures of SA in different social contexts. While these methods seem to quantify symptoms utilizing information from different reporters, those reporters also provide unique perspectives about the manifestation of SA symptoms in a context-dependent manner and should be examined carefully.
Here, we have shown that variance in anxiety symptoms on the SCARED due to child report and variance in anxiety symptoms on the SCARED due to parent report do quantitatively differ after accounting for shared trait variance and error variance, supporting informant disagreement on the SCARED during early adolescence. Previous work has underscored the importance of informant disagreement (De Los Reyes 2011), especially when considering diagnostic utility for clinicians. In terms of anxiety, work has shown that separate informants can report symptoms of anxiety differently on questionnaires (Erath et al. 2007; Langer et al. 2010). Moreover, previous work has found only moderate correlations between child and parent report on the SCARED (Birmaher et al. 1997, 1999; Rappaport et al. 2017) and partial measurement invariance for some subscales (though SA achieved full measurement invariance; Olino et al. 2018). Here, we have replicated the general trend of child-parent report disagreement and extended prior work by leveraging a MTMM confirmatory factor analysis model, rather than traditional correlational analyses, which allows for the parsing of shared (trait) variance vs unique (method and error) variance. Thus, the MTMM model shows that reporter discrepancies are not reflective of simply error, but that there is variance that is unique to child vs parent informants. Indeed, our follow-up analyses of SA, specifically, shed light on the important perspectives of informants in relation to symptomology in different contexts.
Because adolescence is a time when social interaction and peer judgment become increasingly important, we explored differences in child and parent report of social anxiety (SA) on the SCARED. We tested how child and parent report on the SA subscale of the SCARED related to observed SA in front of unfamiliar peers. We utilized direct observations of adolescents interacting with unfamiliar peers, a speech task and a Get to Know You (GTKY) task, as “objective” measures of SA. Parent report explained variance, beyond variance explained by child report, in a controlled speech task. On the other hand, child report explained more variance in a freeform conversation task as compared to parent report. Critically, the model only explained about 10% of the variance in the observed measures, so there is unexplained variance left in observed SA in these contexts that must be explained by other factors.
Moreover, when relating to the speech task, parent report, as compared to child report, more closely resembled latent scores of SA, derived from the MTMM, which remove variance due to reporter method. When relating to the GTKY task, child report, not parent report, was more similar to latent scores of SA. This dissociation again suggests that child and parent report may capture different aspects of SA. There are several explanations for these discrepancies. First, it is possible that parents are able to more accurately report on symptoms that their children present in a structured presentation like the speech task because that is a context within which they may more frequently observe their children (e.g., watching a child perform in a school play). Alternatively, parents may be less able to assess their child’s inner feelings during social interactions with peers, such as what is captured in the GTKY task, as parents are not typically included in these situations. Or finally, parents may be more focused on anxiety symptoms during a child’s performance or presentation, but less attentive to social anxiety symptoms in more routine peer interactions. Adolescents may be more able to introspect on their SA symptoms in these naturalistic, freeform interactions with peers.
Because parents are not deeply involved in peer interactions, recent work has emphasized the advantage of using informants other than the parent when assessing SA in adolescence, namely peer confederate report (Deros et al. 2018; Glenn et al. 2018). Because parent and child reports capture diverse aspects of SA, we also explored how latent factor scores, which reflect the shared trait variance derived from the MTMM model, relate to observed anxiety. Indeed, latent scores related to both the speech task and the GTKY task. Therefore, removing the reporter-specific information can eliminate valuable context-specific social anxiety symptomology that could be useful for both clinicians and researchers.
This study is not without its limitations. First, this sample is not a clinical population and is primarily Caucasian with well-educated mothers. Care should be taken when interpreting the generalizability of these findings and future work should explore how these relations may differ in clinical samples and/or more racially and socioeconomically diverse samples. In addition to demographic factors, it also is possible that parents’ own levels of anxiety influence their perceptions of their children’s anxiety (Briggs-Gowan et al. 1996). Future research that incorporates measures of parents’ anxiety would be helpful in aiding interpretation of parent vs. child report of anxiety. Another limitation is that the order of the GTKY task and the speech task were not randomized. The GTKY was always administered first because it served as the introduction of the unfamiliar peers. Given this ordering, it is possible that some of the anxiety observed during the GTKY task was due to anticipatory anxiety rather than social anxiety per se. However, mean levels of social anxiety did not differ between the speech and GTKY task suggesting that these tasks captured similar levels of anxiety. Future work should also examine other measures of SA, specifically those that primarily focus on SA and how discrepancies between parent and child reports of social anxiety change throughout adolescence.
Conclusion
The SCARED is a widely-used tool used to quantify anxiety symptoms in adolescents through self- and parent-report. However, researchers need to be cognizant and thoughtful about the differences between parent and child report on the SCARED, especially when comparing these values to other measures of anxiety. While shared trait variance from both reporters relate to observed anxiety, parent and child report differentially relate to specific outcomes being investigated, and both sources of information play a valuable role in assessing social anxiety in different contexts.
Supplementary Material
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10802-019-00609-3) contains supplementary material, which is available to authorized users.
Compliance with Ethical Standards
Conflict of Interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures were approved by the University of Maryland Institutional Review Board and in accordance with ethical standards of the 1964 Helsinki declaration and its later amendments.
Informed Consent Informed consent was obtained from all parents of participants and assent was obtained from adolescent participants included in the study.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bailey KA, Chavira DA, Stein MT, & Stein MB (2006). Brief measures to screen for social phobia in primary care pediatrics. Journal of Pediatric Psychology, 31(5), 512–521. 10.1093/jpepsy/jsj044. [DOI] [PubMed] [Google Scholar]
- Behrens B, Swetlitz C, Pine DS, & Pagliaccio D (2018). The screen for child anxiety related emotional disorders (SCARED): Informant discrepancy, measurement invariance, and test–retest reliability. Child Psychiatry & Human Development, 1–10. 10.1007/s10578-018-0854-0. [DOI] [PMC free article] [PubMed]
- Beidel DC, Turner SM, Hamlin K, & Morris TL (2000). The social phobia and anxiety inventory for children (SPAI-C): External and discriminative validity. Behavior Therapy, 31(1), 75–87. 10.1016/S0005-7894(00)80005-2. [DOI] [Google Scholar]
- Bidaut-Russell M, Reich W, Cottler LB, Robins LN, Compton WM, & Mattison RE (1995). The diagnostic interview schedule for children (PC-DISC v.3.0): Parents and adolescents suggest reasons for expecting discrepant answers. Journal of Abnormal Child Psychology, 23(5), 641–659. 10.1007/BF01447667. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SM (1997). The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 545–553. 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999). Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry, 38(10), 1230–1236. 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Bourdon JL, Savage JE, Verhulst B, Carney DM, Brotman MA, Pine DS, Leibenluft E, Roberson-Nay R, & Hettema JM (2019). The genetic and environmental relationship between childhood behavioral inhibition and preadolescent anxiety. Twin Research and Human Genetics, 22(1), 48–55. 10.1017/thg.2018.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, & Schwab-Stone M (1996). Discrepancies among mother, child, and teacher reports: Examining the contributions of maternal depression and anxiety. Journal of Abnormal Child Psychology, 24(6), 749–765. 10.1007/BF01664738. [DOI] [PubMed] [Google Scholar]
- Brown T (2006). Confirmatory factor analysis for applied research. New York, NY: Guildford. [Google Scholar]
- Buzzell GA, Troller-Renfree SV, Barker TV, Bowman LC, Chronis-Tuscano A, Henderson HA, Kagan J, Pine DS, & Fox NA (2017). A neurobehavioral mechanism linking behaviorally inhibited temperament and later adolescent social anxiety. Journal of the American Academy of Child & Adolescent Psychiatry, 56(12), 1097–1105. 10.1016/J.JAAC.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung GW, & Rensvold RB (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 9(2), 233–255. 10.1207/S15328007SEM0902_5. [DOI] [Google Scholar]
- Chronis-Tuscano A, Degnan KA, Pine DS, Perez-Edgar K, Henderson HA, Diaz Y, Raggi VL, & Fox NA (2009). Stable early maternal report of behavioral inhibition predicts lifetime social anxiety disorder in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 48(9), 928–935. 10.1097/CHI.0B013E3181AE09DF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosi S, Canals J, Hernández-Martinez C, & Vigil-Colet A (2010). Parent–child agreement in SCARED and its relationship to anxiety symptoms. Journal of Anxiety Disorders, 24(1), 129–133. 10.1016/j.janxdis.2009.09.008. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A (2011). Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child & Adolescent Psychology, 40(1), 1–9. 10.1080/15374416.2011.533405. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, & Kazdin AE (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509. 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Goodman KL, & Kundey SMA (2013). Principles underlying the use of multiple informants’ reports. 10.1146/annurev-clinpsy-050212-185617. [DOI] [PMC free article] [PubMed]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DAG, Burgers DE, & Rabinowitz J (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858–900. 10.1037/a0038498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deros DE, Racz SJ, Lipton MF, Augenstein TM, Karp JN, Keeley LM, et al. (2018). Multi-informant assessments of adolescent social anxiety: Adding clarity by leveraging reports from unfamiliar peer confederates. Behavior Therapy, 49(1), 84–98. 10.1016/J.BETH.2017.05.001. [DOI] [PubMed] [Google Scholar]
- DiBartolo PM, & Grills AE (2006). Who is best at predicting children’s anxiety in response to a social evaluative task?: A comparison of child, parent, and teacher reports. Journal of Anxiety Disorders, 20(5), 630–645. 10.1016/J.JANXDIS.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Dirks MA, Weersing VR, Warnick E, Gonzalez A, Alton M, Dauser C, Scahill L, & Woolston J (2014). Parent and youth report of youth anxiety: Evidence for measurement invariance. Journal of Child Psychology and Psychiatry, 55(3), 284–291. 10.1111/jcpp.12159. [DOI] [PubMed] [Google Scholar]
- Erath SA, Flanagan KS, & Bierman KL (2007). Social anxiety and peer relations in early adolescence: Behavioral and cognitive factors. Journal of Abnormal Child Psychology, 35(3), 405–416. 10.1007/s10802-007-9099-2. [DOI] [PubMed] [Google Scholar]
- Fox NA, Henderson HA, Rubin KH, Calkins SD, & Schmidt LA (2001). Continuity and Discontinuity of Behavioral Inhibition and Exuberance: Psychophysiological and Behavioral Influences across the First Four Years of Life. Child Development, 72(1), 1–21. 10.1111/1467-8624.00262 [DOI] [PubMed] [Google Scholar]
- Glenn LE, Keeley LM, Szollos S, Okuno H, Wang X, Rausch E, et al. (2018). Trained observers’ ratings of adolescents’ social anxiety and social skills within controlled, cross-contextual social interactions with unfamiliar peer confederates. Journal of Psychopathology and Behavioral Assessment, 1–15. 10.1007/s10862-018-9676-4. [DOI]
- Kazdin AE, French NH, Unis AS, & Esveldt-Dawson K (1983). Assessment of childhood depression: Correspondence of child and parent ratings. Journal of the American Academy of Child Psychiatry, 22(2), 157–164. 10.1016/S0002-7138(09)62329-3. [DOI] [PubMed] [Google Scholar]
- Hane AA, Fox NA, Henderson HA, & Marshall PJ (2008). Behavioral reactivity and approach-withdrawal bias in infancy. Developmental Psychology, 44(5), 1491 10.1037/a0012855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602 Retrieved from http://www.ph.ucla.edu/epi/faculty/detels/PH150/Kessler_DSMIV_AGP2009.pdf. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke K-M, & Hellhammer DH (1993). The ‘Trier social stress test’ – A tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology, 28(1–2), 76–81. 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Lahat A, Lamm C, Chronis-Tuscano A, Pine DS, Henderson HA, & Fox NA (2014). Early behavioral inhibition and increased error monitoring predict later social phobia symptoms in childhood. Journal of the American Academy of Child & Adolescent Psychiatry, 53(4), 447–455. 10.1016/J.JAAC.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer DA, Wood JJ, Bergman RL, & Piacentini JC (2010). A multitrait–multimethod analysis of the construct validity of child anxiety disorders in a clinical sample. Child Psychiatry & Human Development, 41(5), 549–561. 10.1007/s10578-010-0187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau JYF, Lissek S, Nelson EE, Lee Y, Roberson-Nay R, Poeth K, et al. (2008). Fear conditioning in adolescents with anxiety disorders: Results from a novel experimental paradigm. Journal of the American Academy of Child & Adolescent Psychiatry, 47(1), 94–102. 10.1097/CHI.0B01E31815A5F01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee IA, & Preacher KJ (2013). Calculation for the test of the difference between two dependent correlations with one variable in common [Computer software]. Available from http://quantpsy.org.
- Little TD, Cunningham WA, Shahar G, & Widaman KF (2002). To parcel or not to parcel: Exploring the question, Weighing the Merits. Structural Equation Modeling. Retrieved from http://faculty.psy.ohio-state.edu/cunningham/pdf/little.sem.2002.pdf
- Maas CJM, Lensvelt-Mulders GJLM, & Hox JJ (2009). A multilevel multitrait-multimethod analysis. Methodology, 5, 72–77. 10.1027/1614-2241.5.3.72. [DOI] [Google Scholar]
- Mancini C, Van Ameringen M, Bennett M, Patterson B, & Watson C (2005). Emerging treatments for child and adolescent social phobia: A review. Journal of Child a nd A dolescent Psychopharmacology, 15(4), 589–607. Retrieved from. 10.1089/cap.2005.15.589. [DOI] [PubMed] [Google Scholar]
- Marsh HW, & Bailey M (1991). Confirmatory factor analyses of multitrait-multimethod data: A comparison of alternative models. Applied Psychological Measurement, 15(1), 47–70. 10.1177/014662169101500106. [DOI] [Google Scholar]
- Matell MS, & Jacoby J (1971). Is there an optimal number of alternatives for Likert scale items? Study I: Reliability and validity. Educational and Psychological Measurement, 31(3), 657–674. 10.1177/001316447103100307. [DOI] [Google Scholar]
- Monga S, Birmaher B, Chiappetta L, Brent D, Kaufman J, Bridge J, & Cully M (2000). Screen for child anxiety-related emotional disorders (SCARED): Convergent and divergent validity. Depression and Anxiety, 12(2), 85–91. . [DOI] [PubMed] [Google Scholar]
- Moretti MM, Fine S, Haley G, & Marriage K (1985). Childhood and adolescent depression: Child-report versus parent-report information. Journal of the American Academy of Child Psychiatry, 24(3), 298–302. 10.1016/S0002-7138(09)61090-6. [DOI] [PubMed] [Google Scholar]
- Muris P (2002). Relationships between self-efficacy and symptoms of anxiety disorders and depression in a normal adolescent sample. Personality and Individual Differences, 32(2), 337–348. 10.1016/S0191-8869(01)00027-7. [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (2010). Mplus User’s Guide (Sixth). Los Angeles, USA: Muthén & Muthén. [Google Scholar]
- Olino TM, Finsaas M, Dougherty LR, & Klein DN (2018). Is parent–child disagreement on child anxiety explained by differences in measurement properties? An examination of measurement invariance across informants and time. Frontiers in Psychology, 9 10.3389/fpsyg.2018.01295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappaport BI, Pagliaccio D, Pine DS, Klein DN, & Jarcho JM (2017). Discriminant validity, diagnostic utility, and parent-child agreement on the screen for child anxiety related emotional disorders (SCARED) in treatment- and non-treatment-seeking youth. Journal of Anxiety Disorders, 51, 22–31. 10.1016/J.JANXDIS.2017.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy AK, Fudge JL, Kelly C, Perry JSA, Daniele T, Carlisi C, et al. (2013). Intrinsic functional connectivity of amygdala-based networks in adolescent generalized anxiety disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 52(3), 290–299.e2. 10.1016/J.JAAC.2012.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechner T, Rimon-Chakir A, Britton JC, Lotan D, Apter A, Bliese PD, Pine DS, & Bar-Haim Y (2014). Attention Bias modification treatment augmenting effects on cognitive behavioral therapy in children with anxiety: Randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 61–71. 10.1016/J.JAAC.2013.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher LV, Burrows CA, Schwartz CB, & Henderson HA (2015). Social competence with an unfamiliar peer in children and adolescents with high functioning autism: Measurement and individual differences. Research in Autism Spectrum Disorders, 17, 25–39. 10.1016/j.rasd.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


