Sir,
In the celebration of the 200th anniversary of Florence Nightingale's birth, we are facing a pandemic of coronavirus disease (COVID-19) due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has infected more than four million persons with 265,862 deaths [1]. Although ‘Nurses and Midwives: CLEAN CARE is in YOUR HANDS’ is the focus of the World Health Organization (WHO) campaign in 2020, promotion of hand hygiene among all ranks of healthcare workers (HCWs) is very important in the fight against COVID-19. Our institution was a pilot centre in adopting the WHO multi-modal hand hygiene improvement strategy in 2007. Over years of promotion, hand hygiene compliance gradually increased from <25% at baseline (2006) to consistently >70% (from 2011 to 2019) in the hospital. During the COVID-19 pandemic, numerous sessions of sharing forums and departmental visits were arranged to enhance infection control awareness of our HCWs. In addition to the face-to-face training on donning and doffing personal protective equipment (PPE) by infection control nurses (ICNs), we enforced the practice of the WHO ‘my five moments for hand hygiene’, together with our institutionally promoted sixth moment: ‘hand hygiene before touching your mucous membrane’. We continued performing hand hygiene audits according to the WHO protocol. Since the SARS-CoV-2 is predominantly transmitted via droplet and contact routes, hand hygiene with appropriate PPE are key infection control measures to protect HCWs [2]. We therefore expected hand hygiene compliance among our HCWs to increase further during the COVID-19 pandemic.
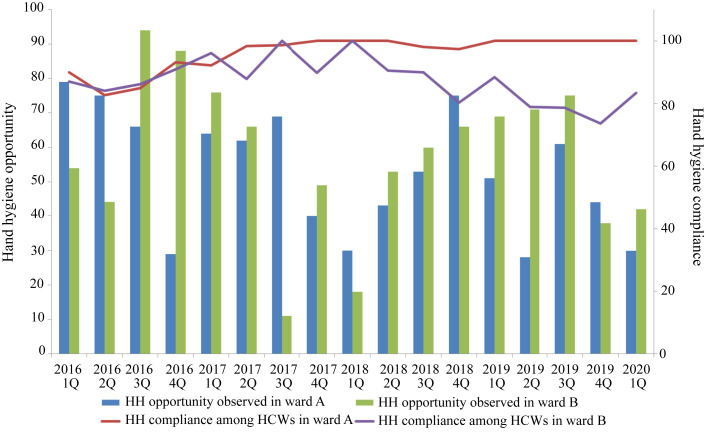
Hand hygiene compliance among HCWs in the paediatric units has been consistently >75% in our institution. Under the leadership of two different unit heads, our two paediatric units (A and B) are located in two different wards (A and B) with comparable numbers of beds and staff; the units are responsible for caring for patients with cardiac diseases and infectious diseases, respectively. In addition to 22 beds for general infectious diseases, there are seven airborne infection isolation rooms (AIIRs) in ward B, which were designated for caring for suspected or confirmed COVID-19 patients. During the COVID-19 pandemic, hand hygiene compliance among HCWs in ward A was 100% (30/30), which was significantly higher than the hand hygiene compliance among HCWs in ward B (83.3%, 35/42; P = 0.037) in the first quarter of 2020. We further analysed the yearly hand hygiene compliance among HCWs in ward A and ward B from 2016 to 2019, and found that the compliance in the two wards had differed since 2017. Indeed, hand hygiene compliance among HCWs in ward A had already achieved 100% in 2019 (Figure 1 , Table I ).
Figure 1.
Hand hygiene compliance among healthcare workers in two paediatric units before and during the COVID-19 pandemic. Paediatric unit A is located in ward A, caring for patients with cardiac diseases. Paediatric unit B is located in ward B, caring for patients with infectious diseases. Airborne infection isolation rooms are only available in ward B, which is designated for the management of suspected or confirmed COVID-19 patients. HCWs, healthcare workers; HH, hand hygiene.
Table I.
Hand hygiene compliance among healthcare workers in two paediatric units before and during COVID-19 pandemic
| Year | Hand hygiene compliance |
P-value | |
|---|---|---|---|
| Ward A | Ward B | ||
| 2016 | 85.8% (182/212) | 87.6% (191/218) | 0.590 |
| 2017 | 96.6% (199/206) | 91.6% (152/166) | 0.036 |
| 2018 | 98.2% (166/169) | 87.3% (151/173) | <0.001 |
| 2019 | 100% (162/162) | 79.8% (174/218) | <0.001 |
It is encouraging to observe 100% hand hygiene compliance among HCWs in paediatric unit A (ward A), especially during the COVID-19 pandemic. Although hand hygiene compliance monitored by ICNs may be subjected to the Hawthorne effect, the same audit protocol was applied to ward B and other specialties [3]. In fact, the key success of hand hygiene compliance is mostly due to the leadership of the unit head of ward A. Instead of being the role model of hand hygiene in the ward, the unit head of ward A empowered ICNs to provide immediate concurrent feedback to the non-compliant HCWs at the bedside. ICNs were requested to send e-mails to the unit head of ward A for each episode of hand hygiene non-compliance for internal evaluation and following up.
It is unexpected to observe relatively lower hand hygiene compliance among HCWs working in ward B, of which some of the beds are used for caring for suspected or confirmed COVID-19 patients. We understand that it may not be realistic to achieve 100% hand hygiene compliance in all units, but lapses in hand hygiene may pose a risk to HCWs, especially during the COVID-19 pandemic. Therefore, we have introduced a buddy system to implement a model of directly observed doffing to minimize the risk of self-contamination [4]. The model of directly observed doffing has been taught to all HCWs who need to work in AIIRs during our face-to-face training sessions. In this model, the HCW is observed by other colleagues during the degowning procedure. Hand hygiene and appropriate degowning are ensured by real-time reminders. This intervention may be a reason why we have achieved zero nosocomial infection by SARS-CoV-2 among HCWs from the pre-pandemic phase of COVID-19, and until now [5].
Hand hygiene among HCWs has become even more important in the context of the COVID-19 pandemic, especially with evidence of SARS-CoV-2 transmission while presymptomatic or asymptomatic [6,7]. Although we have enforced directly observed doffing and directly observed hand hygiene during the critical moments in patient care practice, leaders' commitment to build up a good hand hygiene culture can protect our HCWs and patients in all circumstances including the COVID-19 pandemic [8].
Acknowledgement
We thank our healthcare workers in fighting against the COVID-19 pandemic.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.World Health Organization . 2020. Coronavirus disease 2019 (COVID-19)https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200509covid-19-sitrep-110.pdf?sfvrsn=3b92992c_4 Situation Report – 110. Available at: [last accessed May 2020] [Google Scholar]
- 2.Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gould D.J., Creedon S., Jeanes A., Drey N.S., Chudleigh J., Moralejo D. Impact of observing hand hygiene in practice and research: a methodological reconsideration. J Hosp Infect. 2017;95:169–174. doi: 10.1016/j.jhin.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Wong S.C., Leung M., Yip L.L.Y., Chung K.L., Cheng V.C. Infection control challenge in setting up a temporary test center at the international airport for rapid diagnosis of coronavirus disease 2019 (COVID-19) due to SARS-CoV-2. J Hosp Infect. 2020 doi: 10.1016/j.jhin.2020.05.006. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng V.C.C., Wong S.C., Chuang V.W.M., So S.Y.C., Chen J.H.K., Sridhar S. Absence of nosocomial transmission of coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in the pre-pandemic phase in Hong Kong. Am J Infect Control. 2020 doi: 10.1016/j.ajic.2020.05.018. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lotfinejad N., Peters A., Pittet D. Hand hygiene and the novel coronavirus pandemic: the role of healthcare workers. J Hosp Infect. 2020 Mar 19 doi: 10.1016/j.jhin.2020.03.017. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Furukawa N.W., Brooks J.T., Sobel J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg Infect Dis. 2020 May 4 doi: 10.3201/eid2607.201595. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng V.C.C., Wong S.C., Wong S.C.Y., Yuen K.Y. Directly observed hand hygiene – from healthcare workers to patients. J Hosp Infect. 2019;101:380–382. doi: 10.1016/j.jhin.2018.11.016. [DOI] [PubMed] [Google Scholar]