Abstract
Purpose
To assess perceptions of occupational risk and changes to clinical practice of ophthalmology trainees in the United States during the coronavirus disease 2019 (COVID-19) pandemic.
Design
An anonymous, nonvalidated, cross-sectional survey was conducted online. Data were collected from April 7 through 16, 2020.
Participants
Second-year U.S. vitreoretinal surgery fellows in two-year training programs were invited to participate.
Methods
Online survey.
Main Outcome Measures
Survey questions assessed policies guiding COVID-19 response, exposure to severe acute respiratory syndrome coronavirus 2, changes in clinical duties, and methods to reduce occupational risk, including availability of personal protective equipment (PPE).
Results
Completed responses were obtained from 62 of 87 eligible recipients (71.2% response rate). Training settings included academic (58.1%), hybrid academic/private practice (35.5%), and private practice only settings (6.5%). Overall, 19.4% of respondents reported an exposure to a COVID-19–positive patient, 14.5% reported self-quarantining due to possible exposure, and 11.3% reported being tested for COVID-19. In regards to PPE, N95 masks were available in the emergency room (n = 40 [64.5%]), office (n = 35 [56.5%]), and operating room (n = 35 [56.5%]) settings. Perceived comfort level with PPE recommendations was significantly associated with availability of an N95 respirator mask in the clinic (P < 0.001), emergency room (P < 0.001), or operating room (P = 0.002) settings. Additional risk mitigation methods outside of PPE were: reduction in patient volume (n = 62 [100%]), limiting patient companions (n = 59 [95.2%]), use of a screening process (n = 59 [95.2%]), use of a slit-lamp face shield (n = 57 [91.9%]), temperature screening of all persons entering clinical space (n = 34 [54.84%]), and placement of face mask on patients (n = 33 [53.2%]). Overall, 16.1% reported additional clinical duties within the scope of ophthalmology, and 3.2% reported being re-deployed to nonophthalmology services. 98.4% of respondents, 98.4% expected a reduction in surgical case volume. No respondents reported loss of employment or reduction in pay or benefits due to COVID-19.
Conclusions
Suspected or confirmed clinical exposure to COVID-19–positive patients occurred in approximately one fifth of trainee respondents. Perceived comfort level with PPE standards was significantly associated with N95 respirator mask availability. As surgical training programs grapple with the COVID-19 pandemic, analysis of trainees’ concerns may inform development of mitigation strategies.
Abbreviations and Acronyms: ACGME, Accreditation Council for Graduate Medical Education; AUPO, Association of University Professors of Ophthalmology; COVID-19, coronavirus disease 2019; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
The coronavirus disease 2019 (COVID-19) was declared a global pandemic by the World Health Organization on March 11, 2020.1 Caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), this viral illness may cause severe dysfunction of the respiratory, immune, and other organ systems, resulting in significant morbidity and mortality.2, 3, 4, 5, 6, 7, 8, 9 As of June 24, 2020, 2 295 272 confirmed cases of COVID-19, resulting in 120 171 deaths, have been recorded in the United States.1
The ophthalmology community has been particularly interested in COVID-19 because early reports described ophthalmic involvement and potential transmission via tears and because of the role of the late Dr. Li Wenliang, an ophthalmologist at Wuhan Central Hospital, who initially raised concern of the growing pandemic and was one of its early casualties.5 , 10 , 11 As the disease has spread, reducing occupational risk in the face of an evolving understanding of the disease and its transmission, as well as nationwide shortages of personal protective equipment (PPE), have challenged all medical specialties, including ophthalmology. Meanwhile, the profession’s training programs have been stressed by the reduction in clinical volumes12 because prioritizing only emergent or urgent care has emerged as a key necessary strategy to slow the spread of infection.13
As a result of these changes, COVID-19 has changed the practice of ophthalmology abruptly, including that of its trainees. To the authors’ knowledge, no reports in the medical literature have assessed perception of occupational and educational risks to trainees because of the COVID-19 pandemic. One subpopulation that is of particular interest is vitreoretinal surgery fellows, as retina-related diseases comprise a significant portion of emergent and urgent ophthalmic conditions.13 , 14 This study was performed to assess the experience and concerns of United States retina fellows during the pandemic in terms of risk perception, changes in clinical practice, variations in risk mitigation strategies, and training and career impact.
Methods
An anonymous, nonvalidated, cross-sectional online survey containing 32 questions was created for current 2019 through 2020 senior United States vitreoretinal surgery fellows in 2-year vitreoretinal surgery training programs (Supplemental Appendix, available at www.ophthalmologyretina.org). The survey was developed and administered using SurveyMonkey (SVMK, Inc, San Mateo, CA). This study received an exemption from the Wills Eye Hospital institutional review board because this survey did not collect personally identifiable demographic information and conferred minimal risk. This survey was conducted in accordance with the code of ethics established by the American Association of Public Opinion Research. Survey participants were aware that their responses may be used for research and that completion of the survey was indication of their consent to participate. All research adhered to the tenets of the Declaration of Helsinki.
Eligible fellows were identified from submitted San Francisco Residency and Fellowship Match Services fellowship application files to the Wills Eye Hospital Retina Service fellowship program in the 2017 application year and cross-referenced with a roster of fellow attendees to the 2020 Annual Fellows Forum meeting. Fellows training at institutions outside the United States, fellows designated as international fellows who may not have full clinical privileges, medical retina fellows, and fellows in the first year of vitreoretinal surgery training were excluded.
In all, 87 eligible fellows from 62 training programs were identified and received the survey via e-mail. Survey questions assessed training program environment, policies guiding COVID-19 response, changes in fellow duties and clinical volume, and methods to reduce occupational risk, including availability of PPE. The survey was open from April 7 through 16, 2020. Eligible recipients received an invitation e-mail followed by 2 reminder emails. Participation was voluntary and no compensation was offered.
Data were exported to Microsoft Excel (Microsoft, Redmond, WA), and descriptive characteristics were obtained. With a population size of 87, a sample size of 61 would be required to achieve a 95% confidence interval at a 7% margin of error. A Fisher exact test was used to determine, when applicable, associations between 2 categorical variables, with a P value of less than 0.05 deemed statistically significant.
Results
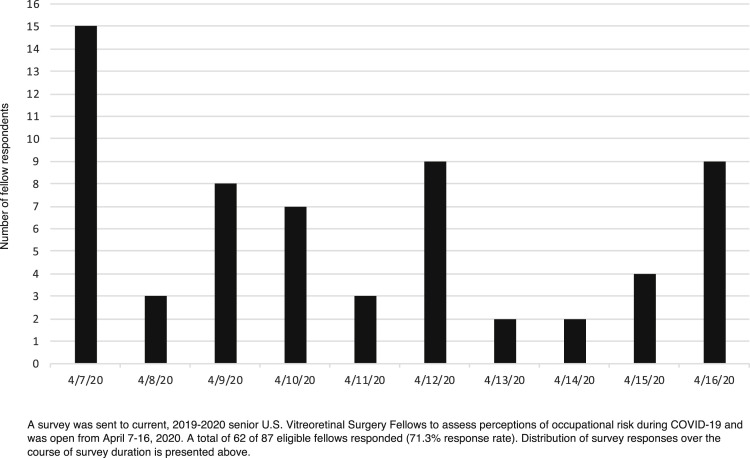
Completed responses were obtained from 62 of 87 eligible recipients (71.2% response rate) from April 7 through 16, 2020 (Fig 1 ). Two fellows chose to opt out of the survey, and the remaining 23 eligible fellows were nonresponders. Of the 62 complete responders, 58.1% (n = 36) reported training at an academic center, 35.5% (n = 22) reported training in a hybrid academic and private practice setting, and 6.5% (n = 4) reported training in a private practice setting. Overall, 50% of respondents (n = 31) trained in metropolitan areas deemed high risk for COVID-19 (Seattle, WA; San Francisco/Bay Area, CA; Los Angeles, CA; Boston, MA; Detroit, MI; Chicago, IL; New Orleans, LA; Miami, FL; Philadelphia, PA; New Haven, CT; and New York City, NY/Northern NJ). These metropolitan areas were chosen by the authors because they include the top 30 United States counties in overall confirmed case total as sourced by the Johns Hopkins University Coronavirus Resource Center as of April 20, 2020.15
Figure 1.
Bar graph showing the distribution of fellow responses during survey availability, April 7 through 16, 2020.
Guidance Regarding Coronavirus Disease 2019 Policies
Sixty respondents (96.8%) reported that the policies developed regarding patient care during the COVID-19 pandemic were influenced by multiple sources. Of these, the most influential sources were the institution in which the fellowship training program held its academic affiliation (n = 52 [83.9%]), the American Academy of Ophthalmology (n = 40 [64.5%]), the United States Centers for Disease Control and Prevention (n = 33 [53.2%]), and the American Society of Retinal Specialists (n = 31 [50.0%]).
Changes to Clinical Duties
Two respondents (3.2%) reported being redeployed to nonophthalmology services (emergency medicine, internal medicine, or intensive care unit), and an additional 19 (30.6%) reported that redeployment is possible in coming weeks. Ten respondents (16.1%) reported reassignment to duties within the scope of ophthalmology, including staffing of a non–retina-related urgent care clinic, staffing of general ophthalmology clinics, participation in telemedicine visits, and being granted full attending privileges in the field of retina.
Respondents who trained in a metropolitan area considered high risk for COVID-19 were not more likely to be redeployed (P = 0.23) than those who did not. Respondents who trained in a metropolitan area considered high risk for COVID-19 were more likely to be assigned additional duties within the scope of ophthalmology compared with those who did not, but this difference was not statistically significant (P = 0.08).
Availability and Use of Personal Protective Equipment
Fifty-eight respondents (95.1%) reported that they are required to wear, at minimum, a surgical mask for all patient contact. Regarding N95 respirator masks, 35 respondents (56.5%) reported their availability in the office setting, 40 respondents (64.5%) reported their availability in the emergency room setting, and 35 respondents (56.5%) reported their availability in the operating room setting. Forty-seven respondents (75.8%) reported that their institution has a policy of sterilizing N95 respirator masks for reuse. Of surveyed PPE items—including N95 respirator masks, surgical masks, eye protection, gloves, and gowns—the least available PPE item in the emergency room or operating room setting was an N95 respirator mask (n = 35 [56.5%] available). In the clinic setting, the least available PPE item was a gown (n = 15 [24.2%] available).
Fifty-seven respondents (91.9%) stated that they believed current PPE recommendations at their training institution were influenced by current or anticipated PPE shortages. Among respondents, 56.5% (n = 35) expressed being comfortable with the PPE recommendations at their institution (n = 28 [45.2%] somewhat comfortable and n = 7 [11.3%] extremely comfortable). Sixteen respondents (26.2%) reported being uncomfortable with PPE recommendations at their training institution (n = 11 [17.7%] somewhat uncomfortable and n = 5 [8.1%] extremely uncomfortable). Comfort level (all comfortable vs. all uncomfortable) with PPE recommendations was associated significantly with availability of N95 masks in the clinic (P < 0.001), emergency room (P < 0.001), and operating room (P = 0.002).
A total of 7 respondents (11.3%) reported that they had no access to an N95 respirator mask. Of these 7, 2 trained at an academic institution, 2 trained in a private practice setting, and 3 trained at a hybrid academic and private practice program.
Assessment of Occupational Risk
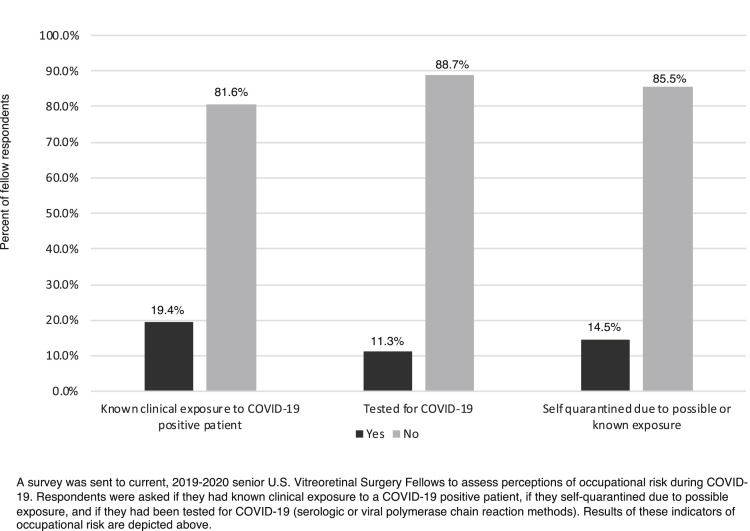
Reported occupational risk is depicted in Figure 2 . Among respondents, 19.4% (n = 12) reported a clinical exposure to a COVID-19–positive patient, 14.5% (n = 9) reported self-quarantining because of possible exposure, and 11.3% (n = 7) reported being tested for COVID-19. Fellows who train in metropolitan areas considered high risk for COVID-19 were not more likely to be exposed to (P = 0.11), undergo testing for (P > 0.99), or self-quarantine because of (P > 0.99) COVID-19. Fellows who train in academic institutions were not more likely to be exposed to (P = 0.11), be tested for (P = 0.39), or self-quarantine (P = 0.46) because of COVID-19 than those who did not.
Figure 2.
Bar graph showing the reported occupational risk of United States vitreoretinal surgery fellows during the coronavirus disease 2019 (COVID-19) pandemic, as of April 16, 2020.
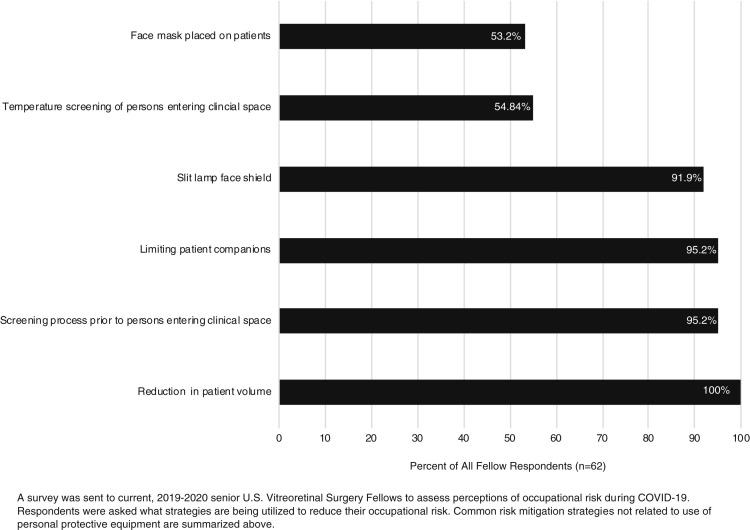
Risk mitigation strategies used at fellow respondent work places are depicted in Figure 3 . Risk mitigation strategies included reduction in patient volume and scheduling (n = 62 [100%]), limiting companions of patients (n = 59 [95.2%]), use of a screening process before patients entering clinical space (n = 59 [95.2%]), use of a slit-lamp face shield (n = 57 [91.9%]), temperature screening of all persons entering the clinical space (n = 34 [54.84%]), and placement of face mask on patients (n = 33 [53.2%]).
Figure 3.
Bar graph showing the risk mitigation strategies used by United States vitreoretinal surgery fellows during coronavirus disease 2019 (COVID-19), as of April 16, 2020.
Access to Operating Room
Forty-five respondents (72.6%) reported that their institution is able to complete any emergent or urgent vitreoretinal surgery in a desired timeframe, whereas an additional 10 (16.1%) reported that their institution is able to complete surgery but in a delayed timeframe. Five respondents (8.1%) reported that surgical patients are being referred to other retinal specialists for surgical care.
Forty-seven respondents (75.8%) reported that their institution’s operating room required additional clearance (preoperative screening or testing) or administrative permission to complete vitreoretinal surgery during the COVID-19 pandemic. Fellows who trained at academic institutions were significantly more likely to report a need for additional clearance to complete operating room procedures (P = 0.03). Forty-nine respondents (81.7%) reported that their operating room facility has specific airborne isolation features available for confirmed COVID-19–positive patients. Regarding office-based procedures, 19 respondents (30.7%) reported availability of a procedure room with specific airborne isolation features when treating COVID-19–positive patients.
Use of Telemedicine
Nineteen respondents (30.1%) stated that fellows at their institution are completing telemedicine visits. Of these, 15 (78.9%) reported use of video-based telemedicine visits, and most reported that the average number of visits was 1 to 3 per week (n = 10/19 [53.6%]). Four respondents (21.1%) reported that fellows are completing more than 10 telemedicine visits per week. No significant association was noted between fellowship setting (academic vs. hybrid academic and private; P = 0.77) and training in an area at high risk for COVID-19 (P = 0.58) with the use of telemedicine by fellows.
Educational Considerations
Among respondents, 98.4% (n = 61) expected a reduction in surgical case volume. Twenty-eight respondents (45.2%) expected a surgical case volume reduction by 50% or more, 8 (12.9%) expected volume reduction by 30%, 18 (29.0%) expected volume reduction by 20%, and 7 (11.3%) expected a volume reduction by 10% or less. One respondent (1.6%) expected an increase in total surgical case volume.
Most respondents (n = 35 [56.5%]) reported concern about the effect of COVID-19 on their surgical training; 14.5% of respondents (n = 9) were extremely concerned and 41.9% (n = 26) were somewhat concerned, whereas 24.2% (n = 15) reported having no concerns regarding the effect of COVID-19.
No respondents reported reduction in pay or benefits or being unemployed or furloughed because of the COVID-19 pandemic. A total of 59 respondents (95.2%) stated that they had accepted a position of employment to start after completion of fellowship training. Of these, 3.4% (n = 2) reported that their employment contract was revoked (n = 1) or that the start date had been delayed (n = 1) because of the COVID-19 pandemic.
Discussion
Health care professionals are at increased risk during the COVID-19 pandemic.16 , 17 Recent data revealed that more than 9282 health care professionals in the United States have tested positive for COVID-19 from February 12 through April 9, 2020, a number considered to be an underestimate of likely health care professional-related cases.18 At the time of this study (April 7–16, 2020), approximately one fifth of responding United States vitreoretinal surgery fellows reported suspected or confirmed clinical exposure to COVID-19–positive patients. Testing rates for SARS-CoV-2 by serologic or polymerase chain reaction methods were lower than these exposure rates (11.3% of respondents reporting testing), possibly because of careful adherence to protective safety measures, the overall shortage of testing capacity in the United States at the time of the exposure, or both. To respect confidentiality, no survey question directly asked if a respondent had physical symptoms or had personally tested positive for SARS-CoV-2. Notably, fellowship program type (academic vs. private practice vs. hybrid) and location in a metropolitan area known to be at high risk for COVID-19 did not have a significant impact on reporting exposure to SARS-CoV-2.
Availability of PPE has been an ongoing source of anxiety and controversy during the COVID-19 pandemic, because evolving guidelines on viral transmission reduction have impacted health care facility recommendations, whereas stresses resulting from PPE shortages have raised concern levels broadly across the ranks of frontline responders. Encouragingly, use of surgical masks among ophthalmology trainees in this study was high: 95.1% of respondents reported use of a surgical mask for all patient contact, and 53.2% reported placement of face masks on patients as a risk mitigation strategy used by their institution. In a recent report, Leung et al19 demonstrated that surgical masks are effective in reducing transmission of seasonal influenza and coronaviruses from symptomatic individuals, highlighting their important role in infection source control as well as PPE.
Access to N95 respirator masks, in particular, has been a flashpoint for risk perception. Many institutions are following current Centers for Disease Control and Prevention guidelines that do not call for routine use of N95 respirator masks for lower-risk interactions, instead reserving them to protect workers in higher-risk settings. In this study, the lone factor significantly associated with perceived comfort level with PPE recommendations during the study period was the availability of an N95 respirator mask, and we further found that 91.9% of respondents stated that they believe their institutional PPE recommendations were influenced by PPE shortages. Among respondents, 11.3% reported they had no access to an N95 respirator mask whatsoever, and approximately half (56.5%) reported availability of N95 respirator masks for use in the ophthalmic operating room or clinic setting. It should be emphasized here that this study assessed perceptions of risk and cannot comment on actuality of risk. Although perceptions reported herein indicate an association of N95 respirator availability with comfort levels regarding PPE, it should not be inferred as a determination of need in all care settings or at the expense of health care workers in high-risk care settings. Evidence-based efforts to determine necessity in the midst of an evolving pandemic, PPE shortages, and calls to consider universal precautions20 are complex and challenging, and perceptions of risk may evolve as wider goals for increased diagnostic testing and PPE supply are addressed and further data on the effectiveness of PPE against SARS-CoV-2 transmission become available.
Olivia Li et al11 recently discussed the importance of preparedness and adoption of risk mitigation strategies to allow necessary ophthalmic care to continue during the COVID-19 pandemic. Fellow clinical practice was in line with these recommendations. Outside of PPE use, the most common risk mitigation strategies in the clinical practice of United States vitreoretinal surgery fellows were reduction in patient volume (100%), limiting companions of patients (95.2%), use of a screening process before patients enter clinical space (95.2%), use of a slit-lamp face shield (91.9%), temperature screening of all persons entering clinical space (54.84%), and placement of a face mask on patients (53.2%). Moreover, 30.1% of respondents stated that fellows at their institution are taking part in telemedicine visits in an effort to reduce in-person interaction. It will be important, as Olivia Li et al noted, that evidence-based efforts be conducted to assess the relative effectiveness of these strategies moving forward.
Unlike ophthalmology residencies, ophthalmology fellowships are not under the purview of the Accreditation Council for Graduate Medical Education (ACGME). However, guidelines set forth by the ACGME regarding medical trainees are helpful in guiding expectations. The ACGME has affirmed 4 priorities regarding trainees during the COVID-19 pandemic, including: adherence to work hour requirements (80 hours/week averaged over 4 weeks), adequate resources and training with regard to PPE and occupational risk, adequate supervision of clinical work, and outlining circumstances in which fellows may function as attendings in their core specialty (the specialty in which they completed their residency training).21 These priorities should be considered by fellowship programs because relevant scenarios are currently affecting fellow clinical practice. Two respondents (3.2%) reported being redeployed to nonophthalmology services, with an additional 19 (30.6%) reporting that this may be possible imminently. Moreover, 16.1% of respondents reported that they have been tasked with additional duties within the scope of ophthalmology, including being granted higher-level clinical privileges. The ACGME, in addition, has conveyed that furloughs of trainees are “unacceptable.”22 No respondents reported reduction in pay or benefits or being unemployed or furloughed because of the COVID-19 pandemic.
The clinical education of trainees in the face of reduced clinical care volume, particularly as the need to limit care to emergent or urgent indications continues, is deserving of special attention and effort. All but 1 respondent (n = 61 [98.4%]) in this study expected a reduction in surgical case volume because of the COVID-19 pandemic, with 45.2% (n = 28) expecting a reduction by 50% or more. Data from the Association of University Professors of Ophthalmology (AUPO) Fellowship Compliance Committee indicate that the average number of vitrectomies performed as primary surgeon by fellows graduating in years 2017, 2018, and 2019 in AUPO-accredited fellowships was 228.4.23 How significant a change in volume will occur, and how or whether this reduction will impact surgical competence, remains to be determined. Efforts to mitigate any negative effect on training, including use of virtual training methods or supplementation with remote surgical or clinical conferences, were not addressed in this survey but are worthy of evaluation.
This study has several limitations. Although the survey achieved a 71.2% response rate, nonresponse bias may be present. To limit this effect and improve response rates, we used e-mail addresses that were listed recently as the primary contact address on fellowship application files and no “bounce-back” e-mails were generated from the survey software. Grouping of question topics was used to avoid order bias. Allowing anonymity and avoiding organizational (e.g., American Society of Retinal Specialists, Association of University Professors of Ophthalmology) sponsorship were used to reduce any response bias. All results are self-reported, so validity of exposure perceptions, institutional policies, and other variables cannot be ascertained. This survey assessed perceptions of occupational risk, and true risk cannot be inferred by these responses. Risk tolerance and comfort levels regarding institutional policies may differ from physician to physician and thus may influence the perceptions described herein. Discussion of data regarding differential reduction of SARS-CoV-2 or other coronavirus transmission with surgical or N95 respirator masks is outside the scope of this study assessing ophthalmology trainee perceptions of occupational risk. Although PPE availability was assessed, more specific technical questions regarding precise PPE details (such as results of fit testing, size of eye protection, use of a surgical vs. standard N95 respirator masks, PPE manufacturer, etc.) were not asked. Vitreoretinal surgery fellows were selected for survey because their specialty often requires urgent and emergent care, and their experience, exposure rates, and perceptions may not be applicable to vitreoretinal surgery attendings or residents or to fellows of different subspecialties. Conversely, because vitreoretinal fellows may be more clinically active during the COVID-19 pandemic, they may be less likely to be redeployed to nonophthalmology settings that could influence their overall exposure risk. Finally, as the COVID-19 pandemic continues, respondent sentiments should be taken in context of the study period evaluated, because risk perceptions and national, local, and institutional policies will continue to evolve, particularly as guidance to reopen surgical facilities for elective and semielective surgery in May 2020 are planned.
In conclusion, the COVID-19 pandemic has, over a period of months, resulted in unprecedented stresses on the United States health care system and health care workers, including trainees. This study reports occupational risk perceptions, currently used risk-mitigation strategies, and surgical volume training concerns for second-year United States vitreoretinal surgery fellows amid pandemic escalation. Elucidating the concerns of ophthalmic surgical trainees, both physical and psychological, can guide mitigation strategies aimed not only to alleviate concerns and enhance workforce health but also to optimize this key period of training, despite its challenges.
Manuscript no. ORET-2020-344.
Footnotes
Supplemental material available at www.ophthalmologyretina.org.
Financial Disclosure(s): The author(s) have made the following disclosure(s): M.A.K.: Consultant - Allergan
J.A.H.: Consultant - Alcon, KalVIsta, Merck, Novartis, Spark Therapeutics; Board of Directors - Bristol-Myers Squibb, Celgene; Financial support - Aura Bioscience, Janssen, Lowy Medical Research Institute, Bionic Sight
Supported by the J. Arch McNamara Research Fund, Philadelphia, PA.
HUMAN SUBJECTS: Human subjects were included in this study. The human ethics committees at Wills Eye Hospital exempted this study because this survey did not collect personally identifiable demographic information and conferred minimal risk. All participants provided informed consent.
No animal subjects were included in this study.
Author Contributions:
Conception and design: Khan, Sivalingam, Haller
Analysis and interpretation: Khan, Sivalingam, Haller
Data collection: Khan, Sivalingam, Haller
Obtained funding: Khan
Overall responsibility: Khan, Sivalingam, Haller
Supplementary Data
References
- 1.World Health Organization WHO COVID-19 dashboard. https://covid19.who.int/ Accessed June 24, 2020.
- 2.Giamarellos-Bourboulis E.J., Netea M.G., Rovina N. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. 2020;April 17 doi: 10.1016/j.chom.2020.04.009. S1931–3128(20)30236–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toscano G., Palmerini F., Ravaglia S. Guillain–Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020 doi: 10.1056/NEJMc2009191. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bangalore S., Sharma A., Slotwiner A. ST-segment elevation in patients with Covid-19—a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu Jun I.S., Anderson D.E., Zheng Kang A.E. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. 2020;127:977–979. doi: 10.1016/j.ophtha.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arabi Y.M., Murthy S., Webb S. COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med. 2020;46:833–836. doi: 10.1007/s00134-020-05955-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helms J., Kremer S., Merdji H. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mao R., Qiu Y., He J.-S. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667–678. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Puelles V.G., Lütgehetmann M., Lindenmeyer M.T. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. 2020 doi: 10.1056/NEJMc2011400. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jun I.S.Y., Hui K.K.O., Songbo P.Z. Perspectives on coronavirus disease 2019 control measures for ophthalmology clinics based on a Singapore center experience. JAMA Ophthalmol. 2020 doi: 10.1001/jamaophthalmol.2020.1288. in press. [DOI] [PubMed] [Google Scholar]
- 11.Olivia Li J.-P., Shantha J., Wong T.Y. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology. 2020;127:569–572. doi: 10.1016/j.ophtha.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehrotra A., Chernew M., Linetsky D. What impact has COVID-19 had on outpatient visits? To the point (blog) Commonwealth Fund. 2020 [Google Scholar]
- 13.American Academy of Ophthalmology List of urgent and emergent ophthalmic procedures. March 27, 2020 https://www.aao.org/headline/list-of-urgent-emergent-ophthalmic-procedures [Google Scholar]
- 14.The American Society of Retina Specialists COVID-19 updates and resources: retina emergent/urgent procedures. https://www.asrs.org/practice/asrs-member-alert-regarding-covid-19-pandemic
- 15.Johns Hopkins Coronavirus Resource Center COVID-19 United States cases by county. https://coronavirus.jhu.edu/
- 16.Zhan M., Qin Y., Xue X., Zhu S. Death from Covid-19 of 23 health care workers in China. N Engl J Med. 2020;382:2267–2268. doi: 10.1056/NEJMc2005696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow E.J., Schwartz N.G., Tobolowsky F.A. Symptom screening at illness onset of health care personnel with SARS-CoV-2 infection in King County, Washington. JAMA. 2020;323:2087–2089. doi: 10.1001/jama.2020.6637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention COVID-19 Response Team Characteristics of health care personnel with COVID-19—United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leung N.H.L., Chu D.K.W., Shiu E.Y.C. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Livingston E.H. Surgery in a time of uncertainty: a need for universal respiratory precautions in the operating room. JAMA. 2020 doi: 10.1001/jama.2020.7903. in press. [DOI] [PubMed] [Google Scholar]
- 21.Accreditation Council for Graduate Medical Education ACGME reaffirms its four ongoing requirement priorities during COVID-19 pandemic. April 5, 2020. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10188/ACGME-Reaffirms-its-Four-Ongoing-Requirement-Priorities-during-COVID-19-Pandemic
- 22.Accreditation Council for Graduate Medical Education ACGME statement on furloughs resulting from the COVID-19 pandemic emergency. April 9, 2020. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10194/ACGME-Statement-on-Furloughs-Resulting-from-the-COVID-19-Pandemic-Emergency
- 23.Association of University Professors of Ophthalmology Fellowship Compliance Committee Surgical retina and vitreous case volumes. https://aupofcc.org/fellowship-programs-residentssubspecialties/surgical-retina-and-vitreous
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.