Clinical Implications.
-
•
In the first 3 weeks of coronavirus disease 2019 restrictions, 45% of scheduled patients cancelled, with remaining patients evaluated by telephone (36%), telemedicine (17%), and in person (2%). Follow-up visits were more likely to be considered to be adequate than new patient visits.
Novel coronavirus disease 2019 (COVID-19) was first identified in Wuhan city, China, and rapidly spread throughout China1 and globally. The first case in the United States was confirmed on January 20, 2020.2 To curb the exponential growth of COVID-19, the Centers for Disease Control and Prevention made the recommendation of social distancing.3 By March 16, 2020, New York state had declared a public-health emergency, and Governor Andrew Cuomo enacted the NYS on PAUSE order,4 closing schools and nonessential businesses. In addition to societal considerations, these recommendations had an immediate impact on all medical practices, including allergy/immunology. In this communication, we report our allergy/immunology office experience in the immediate aftermath of COVID-19 restrictions.
We retrospectively collected encounter data for the 3-week period from March 16 to April 3, 2020, for 3 physicians at Rochester Regional Health Allergy and Immunology. Data on appointment cancellations, new patient (NP) visits, follow-up (FU) visits, sex, age, primary diagnoses, type of visit (telephone, telehealth, in person), billing code, and allergist opinion of encounter adequacy were collected from the electronic health record (Epic, Verona, Wis). The encounter was deemed to be incomplete if desired diagnostic testing (skin testing, spirometry, amoxicillin challenge) would have affected management but could not be completed because of the modality of the evaluation. Data from the 3 weeks preceding COVID-19 restrictions were also collected. A χ2 test and 2-proportion calculator were used to determine the significance of association between encounter completeness and visit type. Of note, capability for telehealth visits using Skype (Palo Alto, Calif) and FaceTime (Apple, Cupertino, Calif) started at Rochester Regional Health during the second week of data collection.
There were 60 half days of clinic among 3 physicians. Of 495 scheduled patients, 225 (45%) chose to cancel whereas 270 (55%) patients underwent evaluation. Of the 270 evaluations, 99 (36.7%) were NP visits and 171 (63.3%) were FU visits, with 98 (36.3%) males and 172 (63.7%) females. The median age of patients was 26 years (interquartile range, 8-54 years). Telephone encounters were most frequently performed in 176 (36%) patients. There were 85 (17%) telemedicine visits, and 9 (2%) in person visits (Figure 1 ). In addition to the 225 cancelled appointments, all 44 food and drug challenges were cancelled by our office. The primary diagnoses were chronic rhinitis/sinusitis (71 [26.3%]), asthma (69 [25.6%]), food allergy (42 [15.6%]), urticaria (26 [9.6%]), drug allergy (11 [4.1%]), and immunodeficiency (10 [3.7%]). Forty-one (15.2%) patients had other diagnoses.
Figure 1.
Evaluation types during COVID-19 restrictions.
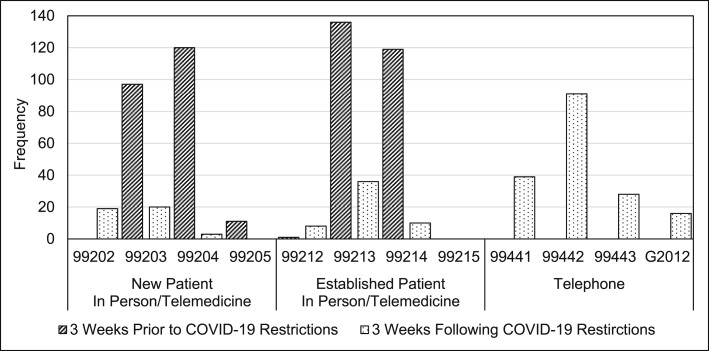
There were a total of 484 patients seen by the same physicians in the 3 weeks preceding COVID-19 restrictions. There was a marked difference in billing codes in the 3 weeks preceding COVID-19 restrictions compared with the 3 weeks of COVID-19 restrictions (Figure 2 ). Before COVID-19 restrictions, the vast majority of NP visits were billed as 99203 (97 patients) or 99204 (120 patients), and most FU visits were 99213 (136 patients) and 99214 (119 patients). Telephone encounters were the most common visit type for both NP and FU evaluation (99441, 99442, 99443, G2012) during the first 3 weeks of COVID-19 restrictions. NP visits done via telemedicine during COVID-19 restrictions were billed as 99202 (19 patients) and 99203 (20 patients), with FU visits being most frequently billed as 99213 (36 patients).
Figure 2.
Current Procedural Terminology coding used during COVID-19 restrictions.
There were 261 evaluations included for physician impression of encounter adequacy/completeness because 9 visits were in person. A total of 178 (68.2%) evaluations were considered complete, and 83 (31.8%) were incomplete. Of the 93 NP visits, 50 (53.8%) were deemed complete and 43 (46.2%) were deemed incomplete. The most common complete diagnoses were chronic rhinitis (13 [26%]), food allergy (14 [28%]), and urticaria (9 [18%]). The most common incomplete visit diagnoses were chronic rhinitis (15 [34.9%]), food allergy (11 [25.6%]), and drug allergy (6 [14%]). For FU visits, 128 (76.2%) visits were complete, compared with 40 (23.8%) incomplete. The most common completed evaluation diagnoses were allergic rhinitis (31 [24.2%]), asthma (54 [42.2%]), and urticaria (13 [10.2%]). The most common incomplete diagnosis was food allergy in 13 (32.5%) patients. FU encounters were deemed to be complete more often than NP encounters (P = .0002). There was no difference in completeness of visits completed via telephone versus telemedicine (P = .400).
Guidelines suggesting allergy/immunology office response to the COVID-19 pandemic are in press.5 Telemedicine has emerged as a strategy to continue allergy/immunology patient evaluations6 in the COVID-19 era. Our analysis provides early information on the implementation of some of these recommendations.
There is good news to be gleaned from our data. Although almost half of scheduled patients cancelled, 55% of patients received medical care. In patients with immediate need, such as an asthma exacerbation, acute urticaria, or acute sinusitis, remote care aids in social distancing efforts and unburdens emergency departments. Remote care also reinforces to patients the message of the necessity of social distancing. In addition, more than 75% of our FU encounters were considered complete. This is helpful information given the uncertainty of COVID-19 restriction duration. Furthermore, although allergists have been slow to adopt telemedicine,7 telemedicine for FU encounters may be a feasible option after resolution of the COVID-19 pandemic. Certain diagnoses lend themselves particularly well to these types of encounters. Telemedicine can also offer care to areas without allergy access.
Unfortunately, despite some good news, our data highlight the unsustainability of the current approach. Nearly half the patients had evaluations cancelled, including all food and drug challenges. In addition, almost half the NP evaluations were deemed incomplete. Although skin testing is not always completed for NP evaluations, most of these incomplete visits were due to the inability to perform skin testing, a diagnostic modality of considerable importance to our specialty, and cannot be done with a telemedicine evaluation of a patient at home. Despite our office encouraging telemedicine encounters to patients, telephone encounters were the most common. We suspect patients did not have the comfort level and/or access to the needed technology. Among other shortcomings, telephone encounters do not provide viable reimbursement to maintain a medical practice.
Our analysis helps define what allergists across the country faced during the immediate aftermath of the COVID-19 pandemic, and this is the main strength of our report. We acknowledge that the retrospective nature of our study is a limitation. Although the generalizability and implications of our findings will be different among academic, employed, and private practice settings, we hope these data highlight the marked patient care and financial ramifications of the immediate response to the COVID-19 pandemic. These metrics can be used to guide our evolving response in the coming weeks and months, and also potentially aid in important advocacy efforts for our specialty. It will remain imperative to monitor the ongoing response to the COVID-19 pandemic, and we hope ours and future data will identify successes, challenges, and areas of needed focus and advocacy.
Footnotes
Conflicts of interest: A. Ramsey has received a research grant from CSL Behring and is on speaker's bureau for Sanofi/Regeneron. S. S. Mustafa has received a research grant from CSL Behring and is on speaker's bureau for Sanofi/Regeneron, Genentech, AstraZeneca, and CSL Behring. The rest of the authors declare that they have no relevant conflicts of interest.
References
- 1.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. Washington State 2019-nCoV Case Investigation Team, First case of 2019 novel coronavirus in the United States. N Engl J Med. 2000;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19) situation summary. https://www.cdc.gov/coronavirus/2019-ncov/index.html Available from:
- 4.New York State Department of Health New York State information on novel coronavirus. https://coronavirus.health.ny.gov/home Available from:
- 5.Shaker M.S., Oppenheimer J., Grayson M., Stukus D., Hartog N., Hsieh E.W.Y. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. 2020;8:1477–1488.e5. doi: 10.1016/j.jaip.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Portnoy J., Waller M., Elliott T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lackman N., Rosen D. 2017 Telemedicine and Digital Health Survey. 2017. https://www.foley.com/en/files/uploads/2017-Telemedicine-Survey-Report-11-8-17.pdf Available from: