The coronavirus 2019 (COVID-19) outbreak hit Asia with little warning. The first cluster of cases was reported in Wuhan, China, on December 31, 2019. By January 23, 2020, Singapore had recorded its first case. The painful memories and experience with the severe acute respiratory syndrome outbreak in 2003 had prepared Asia for this eventuality. Our immediate priorities were to protect the health and safety of patients and staff, to defer nonurgent cases and prioritize visits and treatment, to continue managing sight-threatening conditions, to provide continuity of care for existing patients unable to come for their appointments, and to ensure business continuity.
Protecting the Health and Safety of Patients and Staff
We assumed all patients were potential coronavirus carriers. We established only 1 entry and exit point and set up a triage station outside the clinic. Screening included travel and contact declaration and temperature check. We allowed only 1 accompanying person, and all patients and visitors were masked. Patients were called 1 day before their appointments to enquire about symptoms of fever, sore throat, cough, rhinorrhea, anosmia, and dysgeusia. If present, patients were asked to visit dedicated coronavirus assessment centers in Singapore, rather than the clinic. Strict safe distancing was practiced in the clinic waiting areas: marking out seats to block their use to maintain safe distancing, 1-meter spacing for queues, and so forth.
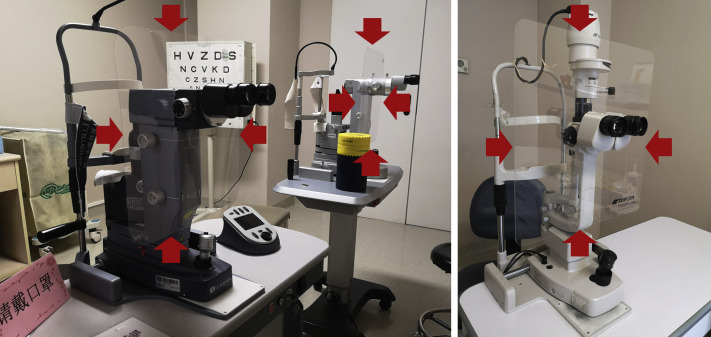
All conjunctivitis patients were treated as high risk. Triage staff and doctors were to don N95 masks (subject to availability), goggles, gown, and gloves in a dedicated examination room with room disinfection and aeration after the visit. We minimized tests and visit time (ideally, less than 15 minutes). Specific measures taken during consultation included minimizing diagnostic tests, disinfecting all equipment used, using disposable eye drops for pupil dilation and topical anesthesia, and using large shields (e.g., plastic) on slit lamps (Fig 1 ).
Figure 1.
Breath shields installed on all slit lamps and laser machines reduce exposure of viral particles for both physician and patient.
The staff was divided into teams to minimize contact. Temperatures were logged daily for all staff. Staff practiced meticulous hygiene and social distancing: wearing masks at all times when on public transportation, practicing frequent hand washing and disinfection, and taking part in refresher training for proper technique for donning and disposing of protective equipment.
Long-term impact: We will maintain emphasis on the importance of public health and personal hygiene practices, especially among healthcare workers. Many staff, including ophthalmologists, may have become complacent about strict infection control in the routine of day-to-day clinical care.
Deferring Nonurgent Cases and Prioritizing Visits and Treatment
Case notes for upcoming appointments were reviewed by the attending doctor to determine suitability for deferment. If the case was deemed nonurgent, staff called the patient, enquiring if the patient’s symptoms were stable and if he or she had any concerns. The necessity for elderly patients, diabetics, and others who are immunocompromised to attend clinics was scrutinized carefully.
Long-term impact: Increased efficiency and reduced waiting time for patients will continue and is the result of streamlining clinic processes. This crisis compelled us to reassess our workflow and eliminate redundancy.
Management of Sight-Threatening Conditions
We provided ongoing care for patients with sight-threatening conditions (e.g., neovascular age-related macular degeneration, especially in the first 2 years of treatment) and new cases of significant vision loss, including new cases of central retinal vein occlusion. Monocular patients were prioritized. Specific to neovascular age-related macular degeneration, we considered fixed dosing for those taking variable regimens; new patients were treated with loading doses as per standard of care. Treatment of patients with diabetic and branch retinal vein occlusion macular edema were eligible for deferment for 1 to 2 months given their lower risk of rapid vision loss. Prolonged postponement of treatment for these cases was avoided.
Long-term impact: This crisis highlighted the need for longer-acting agents and more effective ways of managing chronic eye conditions such as neovascular age-related macular degeneration and diabetic retinopathy.
Use of Telemedical Consultation to Ensure Continuity of Care
We used telemedicine to arrange for prescription refills and home delivery of medications, as well as to teach self-monitoring techniques (e.g., Amsler grid). Regular assessment of patient conditions took place via telemedical consults: patients were reassured by seeing and speaking with their physician. We collaborated with local optometrists and ophthalmologists to monitor vision and intraocular pressure.
Long-term impact: Telemedical consultations will become increasingly crucial in the future. Refinements in telemedicine are needed to enable home-based monitoring, for example, to carry out OCT, intraocular pressure measurement, and vision testing as well as to improve in security and encryption to safeguard patient data and integrity of clinic records.
Business Continuity and Contingency Planning
Significant reduction in revenue occurred during the lockdown associated with reduced patient volume (including patients traveling from abroad for treatment). The impact was severe for institutions that do not receive financial support from the government. Many clinics may not be able to sustain their business costs without financial help.
In terms of unemployment, the Singapore government paid 75% of the wages of all workers during the month-long lockdown, in addition to assisting businesses by deferring company tax payments and offering property tax rebates to landlords, who had to pass the benefit to their tenants; evictions for failure to pay rent were prohibited.
Long-term impact: Developing several streams of income (e.g., telemedical consultations, artificial intelligence-assisted eye screening, online pharmacy) will help to mitigate acute revenue loss, as will taking out insurance to cover for unexpected situations (including key person [individual critical to the running and viability of a business or company] loss) and having an adequate financial buffer such as overdraft and emergency loan options available to the clinic. Government assistance also will be crucial in protecting healthcare workers’ jobs.
Conclusions
Every crisis has a silver lining. As the proverb says, “Necessity is the mother of invention,” so, too, has this unprecedented situation forced us to rethink our old ways of managing our patients. The Chinese word for crisis, 危机, comprises 2 characters, one meaning danger and the other meaning opportunity. With the help of rapidly evolving digital technology, we will be able to overcome many of our current problems. In addition, artificial intelligence will help us triage our patients more accurately so that our time and resources can be used optimally for those who need our personal care and attention. The future has just become much closer than we anticipated.
Footnotes
Financial Disclosure(s): The author(s) have no proprietary or commercial interest in any materials discussed in this article.