Summary
Background
Although mortality due to COVID-19 is, for the most part, robustly tracked, its indirect effect at the population level through lockdown, lifestyle changes, and reorganisation of health-care systems has not been evaluated. We aimed to assess the incidence and outcomes of out-of-hospital cardiac arrest (OHCA) in an urban region during the pandemic, compared with non-pandemic periods.
Methods
We did a population-based, observational study using data for non-traumatic OHCA (N=30 768), systematically collected since May 15, 2011, in Paris and its suburbs, France, using the Paris Fire Brigade database, together with in-hospital data. We evaluated OHCA incidence and outcomes over a 6-week period during the pandemic in adult inhabitants of the study area.
Findings
Comparing the 521 OHCAs of the pandemic period (March 16 to April 26, 2020) to the mean of the 3052 total of the same weeks in the non-pandemic period (weeks 12–17, 2012–19), the maximum weekly OHCA incidence increased from 13·42 (95% CI 12·77–14·07) to 26·64 (25·72–27·53) per million inhabitants (p<0·0001), before returning to normal in the final weeks of the pandemic period. Although patient demographics did not change substantially during the pandemic compared with the non-pandemic period (mean age 69·7 years [SD 17] vs 68·5 [18], 334 males [64·4%] vs 1826 [59·9%]), there was a higher rate of OHCA at home (460 [90·2%] vs 2336 [76·8%]; p<0·0001), less bystander cardiopulmonary resuscitation (239 [47·8%] vs 1165 [63·9%]; p<0·0001) and shockable rhythm (46 [9·2%] vs 472 [19·1%]; p<0·0001), and longer delays to intervention (median 10·4 min [IQR 8·4–13·8] vs 9·4 min [7·9–12·6]; p<0·0001). The proportion of patients who had an OHCA and were admitted alive decreased from 22·8% to 12·8% (p<0·0001) in the pandemic period. After adjustment for potential confounders, the pandemic period remained significantly associated with lower survival rate at hospital admission (odds ratio 0·36, 95% CI 0·24–0·52; p<0·0001). COVID-19 infection, confirmed or suspected, accounted for approximately a third of the increase in OHCA incidence during the pandemic.
Interpretation
A transient two-times increase in OHCA incidence, coupled with a reduction in survival, was observed during the specified time period of the pandemic when compared with the equivalent time period in previous years with no pandemic. Although this result might be partly related to COVID-19 infections, indirect effects associated with lockdown and adjustment of health-care services to the pandemic are probable. Therefore, these factors should be taken into account when considering mortality data and public health strategies.
Funding
The French National Institute of Health and Medical Research (INSERM)
Introduction
Since the emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, the virus responsible for COVID-19),1 initially reported in China in December, 2019,2 and subsequently qualified as a global pandemic by WHO on March 11, 2020,3 almost 5·1 million cases of COVID-19 have been reported worldwide, with more than 333 446 deaths as of May 23, 2020.3, 4
Beyond the direct mortality caused by COVID-19, there are growing concerns regarding the consequences of the COVID-19 pandemic on health systems.5, 6 Lockdown and movement restrictions imposed in several countries, as well as the fear of contamination in hospitals, could have led to a reluctance by patients to call emergency medical services (EMS) or present to emergency departments, resulting in suboptimal health care and delays. Additionally, entire health-care systems have been reorganised to cope with this unprecedented surge of patients with a novel disease that is highly contagious. Deferable routine medical activity, including scheduled hospitalisations and consultations, were cancelled to focus on care for patients with COVID-19, and avoid unnecessary exposure of stable patients to the risk of contamination at the hospital. Altogether, these indirect effects of the COVID-19 pandemic could have detrimental effects on population health.
Out-of-hospital cardiac arrest (OHCA) could be a valuable surrogate for both population health and efficacy of the health-care system in handling emergencies. Although a few media reports have suggested an increase in the incidence of OHCA in several cities, to the best of our knowledge, only one original report described an increase in OHCA incidence in Lombardy, Italy, a setting where the infection has been particularly devastating.6, 7 In this study, we aimed to assess the incidence and outcomes of OHCA during the ongoing COVID-19 pandemic, compared with non-pandemic periods using a real-time multisource surveillance system set up in 2011, in an urban region (Paris and its suburbs, France).
Research in context.
Evidence before this study
After emerging in late-2019, the world has been struggling with an outbreak of a novel disease, COVID-19, declared a pandemic in March, 2020. The pandemic has led to worldwide lockdowns, reorganisation of health-care systems, and postponement of non-urgent medical consultations and interventions. We searched the press media daily and PubMed from database inception, up to May 7, 2020, for reports on out-of-hospital cardiac arrest (OHCA) during the pandemic, using the keywords “cardiac arrest”, “sudden death”, “healthcare”, “emergency medical services”, AND “COVID-19”, “SARS-CoV-2”, “lockdown” with no language restrictions. Although some media outlets have suggested an increase in OHCA in some regions, only one peer-reviewed article described an increase in OHCA incidence in Lombardy, an Italian province where the pandemic was particularly damaging with severe overwhelming of the health-care system, beyond what was experienced in most other regions thus far.
Added value of this study
Our study showed the course of OHCA incidence and outcomes during the COVID-19 pandemic in Paris and its suburbs (6·8 million inhabitants), from the beginning of the surge in infections and lockdown, until the decrease in its incidence. Our results showed a transient two-times increase in OHCA incidence, coupled with a significant reduction in survival, followed by a return to normal towards the end of the study period. Although our findings might be partly related to direct COVID-19 deaths—patients suspected to have or had received a diagnosis of COVID-19 accounted for a third of the increase in cases of OHCA—indirect effects related to lockdown and adjustment of health-care services to the pandemic are probable.
Implications of all the available evidence
This increase in OHCA incidence highlights the collateral deaths, not taken into account in COVID-19 death statistics, and that should be considered when establishing public health strategies for dealing with the pandemic.
Methods
Study design and participants
This population-based, observational study is reported according to the strengthening the reporting of observational studies in epidemiology guidelines.8
The Paris-Sudden Death Expertise Center (Paris-SDEC) ongoing registry has been previously described.9, 10, 11 All cases of sudden OHCA occurring among adults (aged 18 years and older) in the city of Paris and its three suburbs (Hauts-de-Seine, Seine-Saint-Denis, and Val-de-Marne), an area covering 762 km2, have been included in the Paris-SDEC registry since May 15, 2011. Each case was reviewed separately by two investigators to ensure accuracy of classification. Several quality assessments were done to ascertain the completeness of collection in the area.9
In Paris and its suburbs (6·8 millions inhabitants), patients with OHCA are managed by the Paris EMS, a two-tiered response system, coordinated via a unique dispatch centre (not changed during the pandemic period):12, 13 (1) a basic life support tier provided by 197 basic life support teams from the Paris Fire Brigade (Brigade des Sapeurs Pompiers de Paris), who can apply an automatic external defibrillator, and (2) an advanced cardiac life support function provided by ambulance teams with a physician, a nurse, and a paramedic (Paris Fire Brigade or Service d'Aide Médicale Urgente). The Paris Fire Brigade teams usually arrive on scene first and provide basic life support according to the guidelines for OHCA management. The Paris Fire Brigade then calls for advanced life support if considered useful according to case presentation.
Non-traumatic OHCA was defined as any cardiac arrest, after exclusion of cases with obvious accidental causes, irrespective of whether resuscitation was attempted or not. Data were collected using Utstein templates.14
Although there has been no change in the system configuration and case detection during the study period, including during the pandemic, firefighters from the Paris Fire Brigade have had to constantly adapt their practices. They have had to take contagiousness into account, while complying with international recommendations for which a dedicated COVID-19 version has been published.15 Dispatchers from the Paris Fire Brigade were instructed to investigate when receiving the call whether the patient was known to be COVID-19-positive or had symptoms suggestive of COVID-19 infection (fever lasting >48 h before OHCA, with cough, dyspnoea, or both). When COVID-19 infection was confirmed or suspected, EMS personnel were instructed to protect themselves by wearing personal protective equipment before initiating attempted resuscitation.15
The review boards approved the Paris-SDEC registry (Commission Nationale de l'Informatique et des Libertés approval #912309 and Comité Consultatif sur le Traitement de l'Information en matière de Recherche dans le domaine de la Santé approval #12336). No informed consent was required.
Procedures
General data, including Utstein characteristics of the OHCA, were recorded prospectively.14 Response time is defined as the delay between EMS call and arrival (ie, call answer to arrival time).
For the current analysis, given the French COVID-19 epidemic trajectory, we considered the period from March 16 (Paris Lockdown began March 17) to April 26, 2020, as the 6 weeks of the pandemic in the Paris region (corresponding to weeks 12–17 of 2020). We compared patient characteristics, setting of occurrence, and outcome of this period for OHCA reported by the Paris Fire Brigade with the mean for weeks 12–17 of each year from 2012 to 2019 (non-pandemic reference period 1). We also reported data for patients in the Paris-SDEC registry from 2011 to 2020, excluding weeks 12–17 (non-pandemic reference period 2).
A new variable was added to the EMS database, related to COVID-19 status (confirmed or suspected), which allowed us to trace COVID-19 status among patients who had an OHCA (either witnessed or admitted alive).
Statistical analysis
Continuous data are presented as mean (SD) or median (IQR), depending on distribution, and categorical data are presented as n (%). Continuous variables were compared with Student's t test, the Mann-Whitney test, or the Kruskal-Wallis test as appropriate, and categorical variables were compared using the χ2 test.
The maximum weekly incidence of OHCA during the pandemic period (weeks 13 and 14) was compared with the incidence of OHCA during the non-pandemic period 1 (weeks 13 and 14, from 2012–19). The incidences of OHCA and their 95% CIs were estimated by considering the population aged 18 years or older of the four districts. For weeks 12–17, substantial population migration outside Paris and its suburbs was observed and taken into account in each district, based on the data of the National Institute of Statistics and Economic Studies (last assessed on May 6, 2020). Of note, Paris lockdown was maintained throughout the pandemic period, and the subset of the population who left did not return because of movement restrictions.
Additional data for in-hospital mortality as well as hospitalisations related to COVID-19 in the study area were also collected from the National Institute of Statistics and Economic Studies (last assessed May 1, 2020).
Multivariable logistic regression analysis was done to assess the association of the pandemic period with survival at hospital admission. Odd ratios (ORs) and their 95% CIs were calculated with adjustment for potential confounding factors including sex, age, location, bystander cardiopulmonary resuscitation, use of automatic external defibrillator before EMS arrival, shockable cardiac rhythm, and call answer to arrival delay.
p values less than 0·05 were considered statistically significant. Statistical analysis was done using R software, version 3.6.1.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Our study took place between March 16 and April 26, 2020. Overall, from May 15, 2011, to April 26, 2020, there were 30 768 cases of OHCA in the Paris area. The mean age of patients was 68·4 years (SD 18), and 19 002 (61·9%) were men. OHCA occurred at home in 23 282 (76·1%) cases and in public places in 7334 (23·9%) cases. A witness was present in 18 781 (66·1%) cases, and cardiopulmonary resuscitation was initiated in 11 184 (60·6%) cases. An automatic external defibrillator was used in 368 (3·3%) cases before EMS arrival. Overall, 4713 (19·0%) patients with OHCA presented with shockable rhythm (ventricular tachycardia or fibrillation), and 6992 (22·7%) were admitted alive in one of the 48 hospitals of the area.
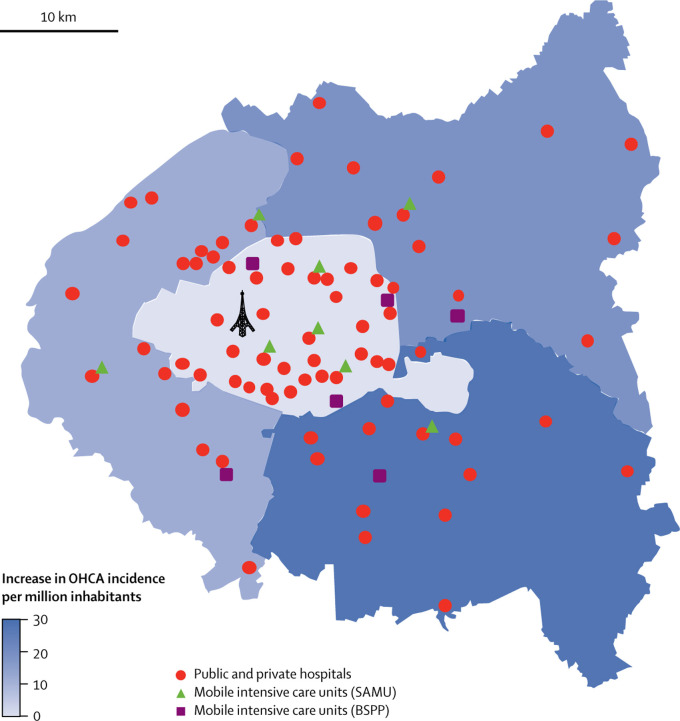
Patient characteristics and circumstances of OHCA occurrence are reported in table 1 . During the pandemic period (March 16 to April 26, 2020), 521 OHCAs occurred, giving a maximal weekly incidence of 26·64 (95% CI 25·72–27·53) per million inhabitants (weeks 13 and 14), significantly higher than the maximal weekly incidence during the same period between 2012 and 2019 (13·42, 95% CI 12·77–14·07; p<0·0001), with a rapid return to normal in the final weeks of the pandemic period (figure 1 , table 2 ). A geographical heterogeneity was found in terms of OHCA increase. A significantly greater OHCA surge was seen in the departments with a low density of medical facilities (eg, northeast of Paris) with an OHCA increase per million inhabitants of 28·33 (95% CI 26·94–29·71) compared with departments with a high density of medical facilities (eg, Central Paris and West Paris) with an OHCA increase per million inhabitants of 13·62 (12·79–14·46; p<0·0001; figure 2 ).
Table 1.
Baseline characteristics, initial management, and outcome of OHCA
| Pandemic period | Non-pandemic period 1 | Non-pandemic period 2 | p value | ||
|---|---|---|---|---|---|
| Sex | 0·038 | ||||
| Women | 185/519 (35·6%) | 1221/3047 (40·1%) | 10 309/27 151 (38·0%) | .. | |
| Men | 334/519 (64·4%) | 1826/3047 (59·9%) | 16 842/27 151 (62·0%) | .. | |
| Age, years | 69·7 (SD 17) | 68·5 (SD 18) | 68·7 (SD 18) | 0·20 | |
| Home location | 460/510 (90·2%) | 2336/3042 (76·8%) | 20 486/27 027 (75·8%) | <0·0001 | |
| Witness | 294/500 (58·8%) | 1887/2908 (64·9%) | 16 600/24 999 (66·4%) | 0·0030 | |
| Cardiopulmonary resuscitation initiated | 239/500 (47·8%) | 1165/1822 (63·9%) | 9780/16 150 (60·6%) | <0·0001 | |
| Public automatic external defibrillator use | 2/500 (0·4%) | 33/1092 (3·0%) | 333/9522 (3·5%) | 0·0012 | |
| Shockable rhythm | 46/500 (9·2%) | 472/2471 (19·1%) | 4195/21 863 (19·2%) | <0·0001 | |
| Median response time, min | |||||
| Call answer to arrival | 10·4 (8·4–13·8) | 9·4 (7·9–12·6) | 9·3 (7·8–12·4) | <0·0001 | |
| On road | 6·4 (4·3–8·5) | 5·1 (3·0–8·1) | 5·0 (3·0–7·1) | <0·0001 | |
| Survival at hospital admission | 67/521 (12·9%) | 695/3052 (22·8%) | 6230/27 195 (22·9%) | <0·0001 | |
| Survival at hospital discharge | 16/517 (3·1%) | 164/3052 (5·4%) | 1450/5731 (5·3%) | 0·0001 | |
Data are n (%), mean (SD), or median (IQR). The pandemic period was defined as the period from March 16 to April 26, 2020, considered as the 6 weeks of the pandemic in the Paris region. Paris lockdown began on March 17. The non-pandemic period 1 was defined as weeks 12–17 of each year from 2012 to 2019. The non-pandemic period 2 was defined as data for patients included in the Paris-Sudden Death Expertise Center registry from 2011 to 2020, excluding weeks 12–17. OHCA=out-of-hospital cardiac arrest.
Figure 1.
Weekly incidences of OHCA during the first 17 weeks of years 2012 to 2020
Compared with previous years and with the beginning of 2020, there was a surge in OHCA incidence starting week 12 of 2020, with a rapid return to normal by week 15. OHCA=out-of-hospital cardiac arrest.
Table 2.
Number, population, and weekly incidences in the different districts of Paris and its suburbs
| Week 10 | Week 11 | Week 12 | Week 13 | Week 14 | Week 15 | Week 16 | Week 17 | ||
|---|---|---|---|---|---|---|---|---|---|
| Number of OHCAs in 2020 | 87 | 83 | 89 | 125 | 128 | 71 | 52 | 56 | |
| Incidence of OHCAs in 2020, per million | 16·14 | 15·40 | 18·38 | 25·81 | 26·43 | 14·66 | 10·74 | 11·56 | |
| Population in 2020, in millions | 5·39 | 5·39 | 4·84 | 4·84 | 4·84 | 4·84 | 4·84 | 4·84 | |
| Paris (district 75) | 1·80 | 1·80 | 1·39 | 1·39 | 1·39 | 1·39 | 1·39 | 1·39 | |
| Hauts-de-Seine (district 92) | 1·26 | 1·26 | 1·18 | 1·18 | 1·18 | 1·18 | 1·18 | 1·18 | |
| Seine-Saint-Denis (district 93) | 1·23 | 1·23 | 1·21 | 1·21 | 1·21 | 1·21 | 1·21 | 1·21 | |
| Val-de-Marne (district 94) | 1·09 | 1·09 | 1·06 | 1·06 | 1·06 | 1·06 | 1·06 | 1·06 | |
| Number of OHCAs in 2019 | 68 | 72 | 74 | 58 | 68 | 58 | 62 | 75 | |
| Incidence of OHCAs in 2019, per million | 12·62 | 13·36 | 13·73 | 10·76 | 12·62 | 10·76 | 11·50 | 13·73 | |
| Population in 2019, in millions | 5·39 | 5·39 | 5·39 | 5·39 | 5·39 | 5·39 | 5·39 | 5·39 | |
| Paris (district 75) | 1·81 | 1·81 | 1·81 | 1·81 | 1·81 | 1·81 | 1·81 | 1·81 | |
| Hauts-de-Seine (district 92) | 1·26 | 1·26 | 1·26 | 1·26 | 1·26 | 1·26 | 1·26 | 1·26 | |
| Seine-Saint-Denis (district 93) | 1·23 | 1·23 | 1·23 | 1·23 | 1·23 | 1·23 | 1·23 | 1·23 | |
| Val-de-Marne (district 94) | 1·09 | 1·09 | 1·09 | 1·09 | 1·09 | 1·09 | 1·09 | 1·09 | |
| Mean number of OHCAs between 2012–18 | 73 | 65 | 63 | 63 | 68 | 66 | 65 | 55 | |
| Mean incidence of OHCAs between 2012–18, per million | 13·69 | 12·22 | 11·78 | 11·91 | 12·77 | 12·35 | 12·26 | 10·40 | |
| Mean population between 2012–18, in millions | 5·31 | 5·31 | 5·31 | 5·31 | 5·31 | 5·31 | 5·31 | 5·31 | |
| Paris (district 75) | 1·83 | 1·83 | 1·83 | 1·83 | 1·83 | 1·83 | 1·83 | 1·83 | |
| Hauts-de-Seine (district 92) | 1·24 | 1·24 | 1·24 | 1·24 | 1·24 | 1·24 | 1·24 | 1·24 | |
| Seine-Saint-Denis (district 93) | 1·17 | 1·17 | 1·17 | 1·17 | 1·17 | 1·17 | 1·17 | 1·17 | |
| Val-de-Marne (district 94) | 1·06 | 1·06 | 1·06 | 1·06 | 1·06 | 1·06 | 1·06 | 1·06 | |
OHCA=out-of-hospital cardiac arrest.
Figure 2.
Density of medical facilities and surge in OHCA incidence across Paris and its suburbs during the pandemic period
Significant differences exist in the density of hospitals and mobile intensive care units in the Paris area, with the highest density observed in central Paris. The highest increase in OHCA incidence was observed in areas with a low density of medical facilities. BSPP=Brigade de Sapeurs-Pompiers de Paris. SAMU=Service d'Aide Médicale Urgente. OHCA=out-of-hospital cardiac arrest.
Patient characteristics did not substantially differ during the pandemic compared with the same non-pandemic period in terms of age (69·7 years [SD 17] vs 68·5 years [18]; p=0·061) and proportion of men (334 [64·4%] vs 1826 [59·9%], p=0·057). By contrast, differences were observed in the circumstances of occurrence of the OHCA. 460 OHCAs occurred at home (460 [90·2%] vs 2336 [76·8%] for the same non-pandemic period; p<0·0001). Additionally, less shockable cardiac rhythm at EMS arrival (46 [9·2%] vs 472 [19·1%]; p<0·0001), and less use of an automatic external defibrillator was observed (0·4% vs 3·0%, p=0·0009; table 1). Response time, defined as call answer to EMS arrival, was significantly longer (p<0·0001).
During the pandemic period, the proportion of OHCAs with resuscitation attempt and advanced life support was lower than usual (53·1% vs 66·2%, p<0·0001), and survival at hospital admission decreased from 22·8% to 12·8% (p<0·0001), with a return to usual incidence followed by a return to usual survival range towards the end of the period (figure 3 ). In multivariable logistic regression analysis, after considering potential confounding factors including sex, age, location, bystander cardiopulmonary resuscitation, use of automatic external defibrillator before EMS arrival, shockable cardiac rhythm, and call answer to arrival delay, the pandemic period remained significantly associated with lower survival at hospital admission (odds ratio 0·36, 95% CI 0·24–0·52; p<0·0001). Survival status at hospital discharge was known in 63 (94·0%) of 67 patients admitted alive. Overall, 16 (3·1%) were discharged alive, compared with 164 (5·4%) in the same non-pandemic period (p=0·029).
Figure 3.
Proportion of patients admitted alive at hospital during weeks 5–17 of 2020 compared with the same period in previous years
Compared with similar periods in the previous years, there was a decrease in OHCA survival at hospital admission during the pandemic period of 2020. OHCA=out-of-hospital cardiac arrest.
In the Paris area, the maximal number of new hospitalisations related to COVID-19 was reached in weeks 13 and 14 (4402 patients; both intensive and non-intensive care units; appendix p 1), whereas maximal COVID-related in-hospital mortality was observed during weeks 14 and 15 (1383 in-hospital deaths overall), then it decreased afterwards.
42 patients were suspected to have COVID-19 (n=17) or had received a diagnosis of COVID-19 (n=25); these numbers account for approximately a third of the increase in cases of OHCA observed in Paris and its suburbs during the pandemic period. Of note, among those admitted alive, screening for COVID-19 was done in 20 (32%) patients whereas 43 (68%) were not tested.
Discussion
During the COVID-19 pandemic, the number of OHCAs occurring in Paris and its suburbs within the specified peak period almost doubled. OHCA survival rate to hospital admission was markedly reduced as well, leading to a major rise in OHCA-related deaths during the pandemic, which started declining at the end of the study period. Although these findings might be partly related to direct COVID-19 deaths, indirect effects through lockdown, behaviour changes, and pandemic-related health system issues (overwhelming of EMS and postponement of consultations and scheduled non-urgent procedures) are probable.
Data from the past 9 years of the Paris-SDEC registry indicate that the incidence of OHCA has been stable over time in Paris and its suburbs, which is in contrast with the major increase observed during the pandemic period. Both direct and indirect effects of COVID-19 might explain this increased incidence.
The lethality of COVID-19 through acute respiratory distress syndrome or an excessive immune response is well established.16 It is therefore possible that some of the OHCAs observed during the pandemic are actually respiratory deaths among patients with COVID-19 who were not hospitalised. Additionally, COVID-19 can lead to cardiovascular injury and myocarditis; experimental treatments such as hydroxychloroquine or azithromycin might also lead to increased cardiac events.17 Acute cardiac events have been observed in patients with COVID-19, including acute coronary syndromes, heart failure, and arrhythmias, therefore making OHCA a possible direct complication of COVID-19. Finally, a major prothrombotic state has been reported during COVID-19 infections, with a consequent increase in thromboembolic events including pulmonary embolisms and acute coronary syndromes.18 To the best of our knowledge, only one original report described an increase in OHCA incidence in Lombardy, Italy, a specific setting where the pandemic was more prolific than what was observed in most regions worldwide.6, 7 Overwhelming of medical services occurred and rules were set to prioritise hospital admissions and intubation among patients with COVID-19. This issue could have led to several deaths from COVID-19 occurring at home and being counted as OHCA, as suggested by the high rate of COVID-19 suspicion or diagnosis among patients who had an OHCA, which accounted for 77% of the surge in OHCA cases in Lombardy. Conversely, in our study, we provide a picture of the surge of OHCA in a setting where a severe pandemic was observed, but the health-care system was still able to handle all known COVID-19 cases without specific limitations, leading to a much lower proportion of cases being related to COVID-19 infection.
Among patients who were negative for COVID-19, an indirect effect, related to changes in public behaviour and reorganisation of the health-care system, might have led to an increase in OHCA in the pandemic setting.19 With lockdown and movement restrictions, patients have more difficulty in seeking medical advice. They might also be reluctant to present to emergency departments or doctors' offices because of fears of COVID-19 infection, or long waiting times. In addition, stable interventions and consultations had to be postponed to prioritise COVID-19-related issues and avoid exposing patients to an unnecessary risk of contamination at the hospital or medical office. Finally, the effect of increased psychological stress during a pandemic, brought about by fear, restriction of movement, and grief due to loss of loved ones, can also potentially trigger adverse cardiac events and arrhythmias, ultimately leading to OHCA.
In addition to the marked increase in OHCA incidence, we also noted a drastic reduction in survival to hospital admission. Witnesses and emergency responders might have been reluctant to do cardiopulmonary resuscitation on potentially infected cases, as cardiopulmonary resuscitation is considered an aerosol-generating procedure with substantial risk of transmission.20 Some hospitals issued directives prohibiting cardiopulmonary resuscitation for patients who potentially have COVID-19 unless full personal protective equipment is worn,21 which could be impractical in the out-of-hospital setting. Besides, more OHCAs occurred at home where the witnesses present during the time of lockdown are most likely to be family members, and are less likely to do cardiopulmonary resuscitation due to emotional involvement and psychological factors.22, 23, 24 Finally, OHCA occurring in patients who were hypoxaemic with COVID-19, and OHCA related to advanced cardiac injury such as in late presenters of acute myocardial infarction, might have worse survival compared with OHCA of cardiac origin.
During the last 2 weeks of the study period, there was a relative decrease in OHCA incidence although survival to hospital admission remained low. The EMS had been reorganised to some extent allowing a progressively better response to non-COVID-19 related calls during the study period. Teleconsultations were developed, and public campaigns were made to encourage seeking of medical attention for symptoms not related to COVID-19, which probably prompted patients to get early medical care upon onset of cardiac symptoms, before OHCA occurrence. The delay in improvement in survival rate compared with incidence is unsurprising, given the persistent low cardiopulmonary resuscitation rate among family members and bed shortages in intensive care units, which obligated EMS to carefully triage OHCA cases likely to benefit from hospital transfer.
Although our study is one of the first to describe the indirect effect of the ongoing COVID-19 pandemic at the population level,6 some limitations need to be acknowledged. First, although we have shown a major increase in absolute OHCA numbers, this change in incidence does not account for the decrease in tourism flow known to be very important at this period in Paris; given the absence of tourists during the pandemic, we might have expected a lower number of OHCAs during the pandemic, potentially underestimating the surge of OHCA that would have occurred if tourists had been present. Second, although COVID-19 status was confirmed in less than 10% of patients, in others, COVID-19 status was either based on the patient's symptoms or unknown. The exact proportion of COVID-19 related OHCAs therefore remains unknown. Additionally, some OHCAs might have occurred in infected patients without being due to the infection. Finally, the study was done in Paris and its suburbs and specificities related to the location, including health-care system organisation, might not be generalisable to other countries.
During the COVID-19 pandemic in the Paris area, we observed a significant and transient increase in the incidence of OHCA, coupled with a major reduction in survival at hospital admission. Although this finding might be partly related to direct COVID-19 deaths, indirect effects related to lockdown and reorganisation of health-care systems might account for a substantial part.
Acknowledgments
Acknowledgments
We thank the Paris-SDEC for providing the logistical support that allowed us to access and analyse the necessary data for the manuscript in such a short period, and the Paris-SDEC collaborators for their multidisciplinary expertise that allows an optimal approach in the fight against sudden cardiac death through this collaborative network since 2011. The Paris-SDEC activities are supported by the Institut National de la Santé et de la Recherche Médicale (INSERM), University of Paris, Assistance Publique-Hôpitaux de Paris, Fondation Coeur et Artères, Global Heart Watch, Fédération Française de Cardiologie, Société Française de Cardiologie, Fondation Recherche Medicale, as well as unrestricted grants from industrial partners (Medtronic, Abbott, Boston Scientific, MicroPort, Biotronik, and Zoll). SDEC Executive Committee is part of the ESCAPE-NET project (Horizon2020 programme). We would like to aknowledge the huge effort of the Paris Fire Brigade in prospectively providing all data regarding OHCA in a real-time manner, and despite the overwhelming COVID-19 pandemic.
Contributors
EM, NK, DJ, WB, and XJ were responsible for the study concept and design. EM, NK, DP, and WB were responsible for the literature search. EM, NK, DJ, FB, AS, VW, BF, and CD were responsible for acquisition of data. EM, NK, DJ, DP, WB, and XJ were responsible for analysis and interpretation of data. EM, NK, KN, WB, XJ were responsible for drafting of the manuscript. DJ, AS, VW, KN, and AL were responsible for critical revision of the manuscript for important intellectual content. EM, NK, BF, and DP were responsible for statistical analysis. EM, NK, and DP were responsible for figures. EM and XJ had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Wu Y, Ho W, Huang Y. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet. 2020;395:949–950. doi: 10.1016/S0140-6736(20)30557-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Coronavirus (COVID-19) events as they happen. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 4.Johns Hopkins University and Medicine COVID-19 map. Johns Hopkins Coronavirus Resource Centre. https://coronavirus.jhu.edu/map.html
- 5.Rosenbaum L. The untold toll—the pandemic's effects on patients without Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMms2009984. published April 17. [DOI] [PubMed] [Google Scholar]
- 6.Baldi E, Sechi GM, Primi R. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020 doi: 10.1056/NEJMc2010418. published online April 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Odone A, Delmonte D, Scognamiglio T, Signorelli C. COVID-19 deaths in Lombardy, Italy: data in context. Lancet Public Health. 2020 doi: 10.1016/S2468-2667(20)30099-2. published online April 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bougouin W, Lamhaut L, Marijon E. Characteristics and prognosis of sudden cardiac death in Greater Paris: population-based approach from the Paris Sudden Death Expertise Center (Paris-SDEC) Intensive Care Med. 2014;40:846–854. doi: 10.1007/s00134-014-3252-5. [DOI] [PubMed] [Google Scholar]
- 10.Jabre P, Bougouin W, Dumas F. Early identification of patients with out-of-hospital cardiac arrest with no chance of survival and consideration for organ donation. Ann Intern Med. 2016;165:770–778. doi: 10.7326/M16-0402. [DOI] [PubMed] [Google Scholar]
- 11.Waldmann V, Bougouin W, Karam N. Characteristics and clinical assessment of unexplained sudden cardiac arrest in the real-world setting: focus on idiopathic ventricular fibrillation. Eur Heart J. 2018;39:1981–1987. doi: 10.1093/eurheartj/ehy098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jost D, Degrange H, Verret C. DEFI 2005: a randomized controlled trial of the effect of automated external defibrillator cardiopulmonary resuscitation protocol on outcome from out-of-hospital cardiac arrest. Circulation. 2010;121:1614–1622. doi: 10.1161/CIRCULATIONAHA.109.878389. [DOI] [PubMed] [Google Scholar]
- 13.Marijon E, Bougouin W, Tafflet M. Population movement and sudden cardiac arrest location. Circulation. 2015;131:1546–1554. doi: 10.1161/CIRCULATIONAHA.114.010498. [DOI] [PubMed] [Google Scholar]
- 14.Jacobs I, Nadkarni V, Bahr J. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 15.International Liaison Committee on Resuscitation 2020. https://costr.ilcor.org/document/covid-19-infection-risk-to-rescuers-from-patients-in-cardiac-arrest
- 16.Fried JA, Ramasubbu K, Bhatt R. The variety of cardiovascular presentations of COVID-19. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047164. published online April 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehra MR, Desai SS, Ruschitzka F, Patel AN. Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet. 2020 doi: 10.1016/S0140-6736(20)31180-6. published online May 22. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 18.Klok FA, Kruip MJHA, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.013. published online April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020 doi: 10.1056/NEJMp2008017. published online April 13. [DOI] [PubMed] [Google Scholar]
- 20.DeFilippis EM, Ranard LS, Berg DD. Cardiopulmonary resuscitation during the COVID-19 pandemic: a view from trainees on the frontline. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047260. published online April 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahase E, Kmietowicz Z. Covid-19: Doctors are told not to perform CPR on patients in cardiac arrest. BMJ. 2020;368 doi: 10.1136/bmj.m1282. [DOI] [PubMed] [Google Scholar]
- 22.Weisfeldt ML, Everson-Stewart S, Sitlani C. Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364:313–321. doi: 10.1056/NEJMoa1010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nakashima T, Noguchi T, Tahara Y. Public-access defibrillation and neurological outcomes in patients with out-of-hospital cardiac arrest in Japan: a population-based cohort study. Lancet. 2020;394:2255–2262. doi: 10.1016/S0140-6736(19)32488-2. [DOI] [PubMed] [Google Scholar]
- 24.Sato N, Matsuyama T, Kitamura T, Hirose Y. Disparities in bystander cardiopulmonary resuscitation performed by a family member and a non-family member. J Epidemiol. 2020 doi: 10.2188/jea.JE20200068. published online April 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.