Letter:
The coronavirus disease 2019 or COVID-19 pandemic has affected more than 200 countries and territories, including the Philippines. As of May 11, 2020, the country has reported 11,086 cases, with the burden of disease in Metro Manila, which includes the capital city of Manila and its surrounding metropolitan areas.1 Metro Manila has been placed on “enhanced community quarantine” since March 16, 2020. This meant classes at all levels, nonessential businesses, and public transportation were suspended to restrict mobility and exposure, and all individuals except essential workers were under “stay at home” orders. To address the rapidly rising number of cases, the government designated 3 public hospitals as COVID-19 referral centers. These included our institution, the Philippine General Hospital, a 1500-bed tertiary referral center that normally caters to 600,000 patients annually. As a result of the restructuring, our institution had to modify and streamline operations and dedicate 110 beds in the wards and 20 beds in the intensive care units for confirmed COVID-19 cases. Outpatient clinics were temporarily closed and elective surgeries were suspended. In this letter, we summarize the experience of the Philippine General Hospital Division of Neurosurgery in dealing with the COVID-19 pandemic and discuss changes in service and training from the perspective of a neurosurgical center in a developing country.
Patient Management Protocol
All elective neurosurgical admissions at our institution were suspended starting March 18, 2020. One wing of the hospital's operating room (OR) complex was dedicated to urgent and emergent surgeries of confirmed and suspected COVID-19 cases, whereas the other wing was used for emergency surgeries of non-COVID patients already admitted in the hospital. The hospital's Operating Room Management Team defined emergency cases as any condition that can result in loss of life or limb if surgery was deferred by more than 24 hours. For neurosurgery, emergency surgeries included: 1) craniotomy and evacuation or excision of hematoma/tumor/abscess for patients in impending herniation; 2) decompressive craniectomy for patients in impending herniation; 3) cerebrospinal fluid diversion procedures for patients with acute hydrocephalus; 4) craniotomy and clipping of ruptured aneurysm; 5) laminectomy for excision of a spinal tumor in patients with deteriorating neurologic function; and 6) reoperations for currently admitted patients.
The protocols for preoperative assessment of patients requiring surgery evolved rapidly during this period. Initially, all patients had to be seen by the Infectious Disease service and assessed if they were either a confirmed case or a “person under investigation.” If they were, the surgeries had to be performed in the COVID wing of the OR, where personnel had to don Level 4 personal protective equipment (PPE). Level 4 PPE includes a cleanroom suit, hair cover, goggles, improvised face shield, and an N95 mask. Otherwise, the patient was operated on in the non-COVID wing, where personnel only had to don Level 3 PPE, which includes a surgical gown in place of a cleanroom suit. With the recognition of the increasing community transmission of the infection, this protocol was revised, in that all patients were required to undergo the gold standard real-time polymerase chain reaction testing of specimens taken from nasopharyngeal swabs. However, because of the limited number of testing centers in Metro Manila, the turnaround time for tests was between 3 and 7 days. As such, many of the emergent cases had a yet undetermined COVID-19 status at the time of surgery and were presumed to be “persons under investigation,” warranting the enhanced infection control measures adopted for confirmed COVID-19 cases. Level 4 precautions were later adopted for surgeries in both wings to protect health care workers from possible false-negative cases.
In the 6 weeks since it has been designated a COVID-19 referral center, the hospital has admitted a total of 265 confirmed COVID-19 cases. In this time period, the neurosurgical service has had 4 referrals of confirmed COVID-19 cases and performed surgery in 3. The surgeries performed were clipping of a ruptured aneurysm, evacuation of a traumatic intraparenchymal hematoma with an overlying subdural hematoma, and evacuation of a spontaneous intracerebral bleed. In the same time period, the service has had 19 admissions and 16 referrals of non-COVID cases, on whom 22 operations were performed. For context, in the same time period last year, the neurosurgical service had 234 admissions and 138 referrals, and performed 54 emergency and 139 elective surgeries. This represents a reduction of 92% in admissions, 88% in referrals, and 54% in emergency surgeries.
Perioperative and Intraoperative Safety Precautions
To reduce infection risk, the number of persons in the OR was kept to a minimum. A preoperation huddle with all members of the operating team was done, with all members briefed regarding their role during the operation in view of the enhanced infection control measures. During intubation and extubation, the protocol allowed only 2 anesthesiologists to be present inside the OR. The intubation was done with the patient's head under an acrylic “aerosol box” and with the use of a video laryngoscope.
It was assumed that anything that entered the OR with the COVID patient inside was contaminated, including personnel. The operating team members were not allowed to bring in mobile phones, laptops, or other personal belongings. Opening of the OR door was limited while the patient was inside, with handover of supplies done in an anteroom. Personnel within the OR were able to communicate with the ones outside through a 2-way radio or white board shown through a glass panel.
We always looked for strategies to reduce operating time and exposure risk, which factored into surgical decision-making. In the COVID-positive patient with acute subdural and parenchymal hematoma, the decision was made to evacuate the hematoma using a smaller opening rather than a large craniotomy, in order to reduce operative time.
Patel et al2 have raised caution regarding the possible increased exposure risk with endonasal approaches for skull base lesions presumably due to the viral load in the upper respiratory tract. Although we have yet to manage a pituitary tumor patient requiring emergency surgery, we will preferentially consider transcranial approaches. In our craniotomies, care is taken not to expose the frontal sinus. Six cases of ruptured aneurysms were clipped since the hospital's designation as a COVID-19 referral center, one of which was in a confirmed COVID-19 case. In all these cases, a minipterional craniotomy measuring 2.5–3 cm in greatest diameter was used, and the total operative time was between 2 and 3 hours. These minimally invasive approaches have the dual advantages of reducing operative time and the risk of opening the frontal sinus.
Powered air-purifying respirators are recommended to be worn by the operating team, but this was not readily available in our setting.2 Instead, we used a 3M 6200 half face respirator with P100 filters, goggles, and face shield at the start of surgery, with the face shield and goggles removed when the microscope is used. In cases where an operating microscope was not necessary, a 3M 6800 full face respirator with P100 filter was used. For additional protection, we have also used a sterile transparent plastic sheet held over the operative field by a sterilized Mayo table. We posit that this could shield the operating team from viral particles that can be aerosolized by activities such as the use of high-speed drills, irrigation, and monopolar cautery (Figure 1). Some staff members have also used impermeable occlusive dressing to cover the nose and mouth of intubated patients to act as another barrier against aerosolized viral particles (Figure 2 ).
Figure 1.
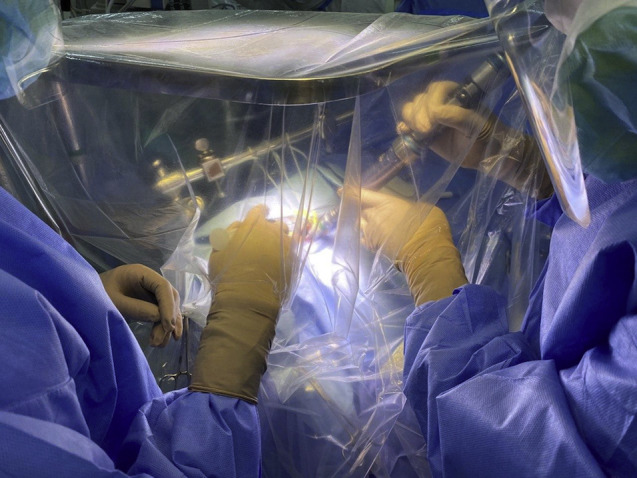
Sterile transparent plastic sheet placed over a Mayo table holder acts as a barrier to reduce exposure of the operative team to aerosolized viral particles.
Figure 2.

Water impermeable occlusive dressing was applied over the nose and mouth and wrapped around the endotracheal tube.
Personnel and Training Considerations
The hospital adopted a rationalized call schedule for personnel. Physicians, nurses, and other health care workers were assigned to 3 teams, with 1 team going on week-long calls, followed by a 2-week quarantine period spent in nearby lodging areas. Similarly, neurosurgery personnel were organized into teams of 3 residents supervised by a consultant staff member going on call for 1 week at a time.
To augment the limited workforce assigned to the dedicated COVID wards and intensive care units, a neurosurgical resident was redeployed to take one 8-hour shift in the dedicated COVID critical care unit for 1 week at a time. Our hospital has employed the “task-sharing” model to quickly address the issue of manpower to run the dedicated COVID units. Task-sharing describes a duty redistribution scheme where qualified personnel take on clinical responsibilities along with less trained personnel, facilitating training of the latter.3 In this context, the neurosurgical resident learns the principles of critical care management of COVID-19 patients while working closely with a senior resident and staff from internal medicine. Neurosurgical staff members also took on additional roles. The Chief of Neurosurgery, who is also the hospital director, is spearheading the hospital's COVID-19 response, whereas many staff members sit in ad hoc committees set up to coordinate the response.
In terms of training, all the teaching activities for residents have shifted online, with weekly topic conferences, residents' lectures, and case reviews done via teleconferencing. Operative training opportunities have also decreased markedly, especially for junior residents. Because of the need to decrease operative time and minimize the number of personnel in the OR, the most capable and experienced team members were the ones performing the surgery.
Challenges and Future Directions
The Philippines has a neurosurgeon-to-population ratio of 1:807,000, which is less than ideal,4 and there are only a handful of centers nationwide that have the capacity to manage complex neurosurgical cases. Our institution is one of these, being the largest among the 10 neurosurgical training centers in the country. Our center is also a public hospital, which means that service patients get free medical care. In a country with no universal health coverage and with out-of-pocket expenditures accounting for up to 54% of total health expenditure,5 our center is a lifeline for many of the poor in the population. Intuitively, the cancellation of elective surgeries in our center would worsen the backlog of patients requiring neurosurgical care, and is untenable in the long term.
We expect neurosurgical services to be resumed in a gradual and measured manner while the hospital and the community at large adapt to a “new normal.” Issues include the following: 1) maintenance of the safety of both patients and health care personnel with strict measures to prevent health care–associated infections, 2) active management of patients in the backlog and continuous reprioritization of patients for surgery, and 3) provision of adequate resources in terms of both hospital supplies and manpower for the health care needs of both COVID and non-COVID patients. These are particularly challenging for low-resource settings. The large volume of PPE required by enhanced infection control measures has considerably increased health care expenditure. Telehealth services being set up to facilitate patient consultation with the health care team are also inaccessible to many of our poor patients with no reliable internet access. The health care workforce also remains strained with the massive burden brought about by the dedicated COVID care units. At present, providing essential service has taken priority over training as the hospital's resources are redirected to address the pandemic.
Conclusion
The COVID-19 pandemic has resulted in disruptions in the service and training of neurosurgical centers worldwide. The effects are particularly grave for low-middle income countries. Even so, centers such as ours are exhausting all means to give the best possible outcomes to neurosurgical patients.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.World Health Organization Coronavirus Disease (COVID-19) Situation Report—108. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200507covid-19-sitrep-108.pdf?sfvrsn=44cc8ed8_2 Available at:
- 2.Patel Z.M., Fernandez-Miranda J., Hwang P.H. Letter: Precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery. 2020;87:E66–E67. doi: 10.1093/neuros/nyaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robertson F.C., Briones R., Mekary R.A. Task-sharing for emergency neurosurgery: a retrospective cohort study in the Philippines. World Neurosurg X. 2020;6:100058. doi: 10.1016/j.wnsx.2019.100058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferraris K.P., Matsumura H., Wardhana D.P.W. The state of neurosurgical training and education in East Asia: analysis and strategy development for this frontier of the world. Neurosurg Focus. 2020;48:E7. doi: 10.3171/2019.12.FOCUS19814. [DOI] [PubMed] [Google Scholar]
- 5.The World Bank Data Base Out-of-pocket expenditure. https://data.worldbank.org/inddicator/SH.XPD.OOPC.CH.ZS Available at:


