Abstract
Adjustment disorder with anxiety (ADA) is a common psychiatric pathology worldwide, but it is often undertreated. Cognitive behavioral therapy (CBT) is the first-line treatment, but very few studies have been carried out for the treatment of ADA. Internet-delivered CBT (iCBT) appears to be an effective treatment option, with the potential to reach a larger proportion of individuals suffering from ADA. Guidance is a beneficial feature of iCBT, provided in most studies by email or telephone (traditional guided iCBT). Blended CBT, which combines an online intervention and therapeutic guidance provided in person (face-to-face), could be a way to benefit from both the advantages of face-to-face CBT regarding human interactional quality and the advantages of internet-based CBT in terms of improved access to treatment.
In this randomized controlled trial, the effectiveness of two forms of administration of Seren@ctif, a 5-week CBT program for patients with ADA according the DSM-5, was examined: one delivered through face-to-face sessions (face-to-face CBT) and the other delivered online and guided with face-to-face contact with a nurse (blended CBT); these formats were compared with a wait-list control group (WLC). A total of 120 patients were included and randomized to one of these three conditions. Measures were administered before treatment, after treatment and 6 months after inclusion in the study. Both treatment conditions displayed significant decreases in anxiety, depression, worry and perceived stress at posttreatment when compared to the WLC group. The decrease in symptoms was mostly maintained 6 months after inclusion for the two experimental groups. Blended CBT showed significantly greater reductions in anxiety and depression than did face-to-face CBT on some secondary outcome measures.
We conclude that both face-to-face CBT and blended CBT are effective treatments for patients with ADA, and we suggest that blended CBT may be slightly more effective than classical face-to-face CBT.
Trial Registration: Clinicaltrials.gov NCT02621775;https://clinicaltrials.gov/ct2/show/NCT02621775(Archived by WebCite at http://www.webcitation.org/6tQrkPs1u).
Keywords: Cognitive behavioral therapy, Guided internet-based treatment, Adjustment disorder with anxiety, Psychological stress, Randomized controlled trial
Highlights
-
•
Adjustment disorder with anxiety (ADA) is a common disorder that is undertreated, Internet interventions is of interest.
-
•
Internet-based cognitive behavioral therapy with human guidance and delivered face-to-face are both effective for ADA.
-
•
Blended CBT is a way to benefit from the advantages of human interaction that face-to-face CBT offers.
-
•
Combining online and face-to-face intervention may be a cost-effective alternative to face-to-face CBT for patients with ADA.
-
•
Blended CBT could be more effective than other intervention formats, such as face-to-face CBT or traditional guided iCBT.
1. Introduction
Adjustment disorder with anxiety (ADA) is a frequent stress-related psychiatric disorder. In primary care and in consultation liaison psychiatry, the prevalence ranges from 11% to 18% and from 10% to 35%, respectively (Casey, 2009). According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), a diagnosis of ADA is appropriate for the finding of anxiety occurring within 3 months of a psychosocial stressor or life event (e.g., divorce, job loss, serious physical illness), with symptoms generally abating by 6 months after the event (American Psychiatric Association, 2013). ADA occurs when someone has pronounced emotional and/or behavioral symptoms in response to the stressor that exceed an expected stress response and/or when there is significant impairment in social or occupational functioning. These symptoms can include excessive worry, nervousness or behavioral disorders.
In addition to its negative impact on health, well-being and quality of life, ADA is responsible for significant direct and indirect costs from treatment, work hiatuses, and productivity losses (Sauter et al., 1990). Given the significant negative consequences of this pathology linked to stress and prevalence rates, effective treatments addressing psychological symptoms are needed. However, research is lacking regarding treatments for adjustment disorders (Casey, 2014).
Cognitive behavioral therapy (CBT) is the first-line treatment for anxiety disorders (Cuijpers et al., 2014; Otte, 2011). It combines behavioral and cognitive interventions in a problem- and action-oriented approach (Beck, 2011). Numerous studies have shown that CBT is an effective treatment for reducing stress and anxiety in subjects with somatic pathologies such as cardiovascular disease (Turner et al., 1995; Campbell et al., 2012), diabetes (Attari et al., 2006), and chronic fatigue syndrome (Lopez et al., 2011), as well as in subjects with a high level of perceived stress or anxiety, particularly in the workplace (Bhui et al., 2012).
Few studies have evaluated the effectiveness of CBT in the treatment of ADA (O'Donnell et al., 2018). Two uncontrolled case studies provide preliminary evidence of its effectiveness (Hirsh et al., 2009; Powell and McCone, 2004). A small RCT in 57 patients with various types of cancer with abnormal adjustment showed that CBT produced greater changes in anxiety than a nondirective supportive intervention over an 8-week period of treatment (Moorey et al., 1998). In another controlled trial in Dutch employees on sick leave, 67% had adjustment disorder, highlighting that CBT and work-focused CBT are both effective in improving anxiety and depression (Lagerveld et al., 2012).
Numerous barriers can hinder an individual from seeking or receiving CBT treatment. One significant barrier is the ability to access this evidence-based treatment. Internet-delivered CBT (iCBT) interventions are a relatively new development that could help with increasing access to treatments. iCBT is gradually disseminated from research settings to routine care (Titov et al., 2019). Recently, a review of 9 meta-analyses gathering 166 studies (Andersson et al., 2019) suggested that iCBT is an effective treatment for anxiety and mood disorders, such as panic disorder, social anxiety disorder, generalized anxiety disorder, posttraumatic stress disorder and major depression, compared to different control conditions, typically a wait-list control group or patients receiving usual treatments. Several meta-analyses have suggested that iCBT may be as effective as face-to-face therapy (e.g., Andersson et al., 2014; Carlbring et al., 2018; Cuijpers et al., 2010; Andrews et al., 2018). While the overall results indicate equivalence, there are still only a few studies for each psychiatric and somatic condition and many conditions for which iCBT has not been compared to face-to-face treatment.
In psychiatric pathologies such as social phobia or depression, guidance is a beneficial feature of internet-based interventions (Baumeister et al., 2014) and might decrease attrition rates (Zagorscak et al., 2018). Likewise, in stress and anxiety associated with somatic pathologies or stress at work, guided web-based mental health interventions are significantly superior and have higher adherence rates than unguided interventions do (Heber et al., 2017). An RCT of unguided internet-based self-help interventions in subjects with adjustment disorder (according to the International Classification of Diseases, 11th Revision (ICD-11)) who were recruited by announcement via newspaper and Facebook showed a very high dropout rate (86%) (Eimontas et al., 2018).
In all studies, therapeutic guidance is provided by email or telephone or via discussion forums (traditional guided iCBT). According to Mohr et al.'s (2011) accountability model, to promote adherence and credibility to treatment, a social presence is necessary. Therapeutic guidance provided in person (face-to-face) could be a way to benefit from the human interactional quality of face-to-face CBT. “Blended interventions” or “technology-supported care”, which combine an online intervention and a face-to-face component, seem to be an effective solution to obtain optimal benefit from the advantages of these two treatment modalities (Erbe et al., 2017; Wentzel et al., 2016). However, thus far, no studies have directly compared face-to-face CBT with the same blended CBT for the treatment of ADA.
Hence, the aim of the study was to examine the effectiveness of two forms of administration of a cognitive behavioral intervention for ADA (Seren@ctif): one delivered through face-to-face sessions (face-to-face CBT) and the other delivered via e-learning guided by face-to-face contact with a nurse (blended CBT). These two forms of intervention were compared with a wait-list control (WLC) group in their ability to reduce symptoms of anxiety, depression, perceived stress and worry in patients with a diagnosis of ADA according the DSM-5.
The primary objective was to assess the effectiveness of face-to-face CBT and blended CBT compared with a WLC group in reducing anxiety after 2 months of treatment in patients with a diagnosis of ADA. The secondary objectives of this study were as follows: (1) to assess the effectiveness of face-to-face CBT and blended CBT compared with a WLC group in reducing worry, perceived stress and depression after 2 months of treatment in patients with a diagnosis of ADA; (2) to compare the psychological symptoms between the 2 therapeutic programs after 2 months of treatment and 6 months after inclusion in the study; (3) to evaluate the maintenance of the gains 6 months after inclusion in the study; and (4) to compare the overall satisfaction of participants between the 2 therapeutic programs after 2 months of treatment and 6 months after inclusion in the study.
2. Material and methods
A more detailed description of the methodology was provided in the study protocol paper (Servant et al., 2017).
2.1. Design
This was a multicenter, comparative, prospective, unblended, randomized, controlled study of 3 parallel groups: (1) an experimental group receiving iCBT supported by minimal face-to-face contact time with a nurse (blended CBT), (2) an experimental group receiving the same stress management module through face-to-face sessions performed by a therapist trained in clinical psychology (face-to-face CBT), and (3) a wait-list control (WLC) group.
2.2. Ethics
The project was approved by the local ethics committee (approval number CPP 15/12), which is required for medical intervention research in France. Data processing was conducted in accordance with the requirements (reference methodology 06001).
2.3. Participants
2.3.1. Eligibility
Each newly referred patient was asked to complete the optional adjustment disorder section of the French version (Lecrubier et al., 1997) of the Mini International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998) to confirm that he or she met the ADA criteria according to the DSM-5. The MINI was administered during a face-to-face interview by a clinical investigator who was trained in psychiatry.
2.3.2. Inclusion criteria
The inclusion criteria were as follows: (1) ambulatory patient; (2) male or female aged 18 to 60 years; (3) diagnosis of adjustment disorder with anxiety (ADA) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; (4) not supported by structured psychotherapeutic treatment for ADA or any other problem; (5) taking no new psychotropic drug therapy or stabilized for at least 3 months (in the latter case, the patient was informed of the need to keep the same dosages for the duration of the study); (6) a minimum score on the Hospital Anxiety and Depression scale (HADS) anxiety subscale greater than or equal to 10 and a maximum score on the HADS depression subscale of <10; and (7) access to a computer.
2.3.3. Exclusion criteria
The exclusion criteria were as follows: (1) inability to read or use a computer with support (the platform is easy-to-use, and a nurse is available to guide the patient in the navigation of the computer program); (2) pregnancy (as recommended by the French ethics committee; urine pregnancy test performed on female patients); (3) being incapable of consenting, not having legal protection, or being deprived of liberty; and (4) diagnosis of another psychiatric disorder (according to the Mini International Neuropsychiatric Interview).
2.4. Recruitment
The study was conducted in a stress and anxiety unit (a psychiatric consultation service) at Lille University Hospital in France. Patients were referred by their general practitioner for the psychological treatment of anxiety symptoms in the context of recent stress. To improve recruitment, general practitioners in the area were informed of the study by a local investigator during continuing medical education, during scientific meetings, and through all types of collaborative contacts between primary care and psychiatry services.
2.5. Randomization
Immediately after inclusion and assessment, patients were randomly allocated in a 1:1:1 ratio into 3 groups using a web-based central randomization process: patients using a digital stress management module guided by face-to-face contact with a nurse (blended CBT), patients following the stress management module guided by a therapist in attendance (face-to-face CBT), and patients on a waiting list and benefiting from usual care through their attending physician (WLC). The randomization sequence was provided by an independent statistician (who did not take part in assessing the patients at any point in the study) using computer-generated random numbers with block sizes of 6 and center stratification consistent with the Consolidated Standards of Reporting Trials (CONSORT) (Moher et al., 2001). The randomization sequence was implemented in the electronic case report form (eCRF) system to ensure a centralized, real-time randomization procedure. A document describing the randomization procedure was kept confidential in the Clinical Investigation Centre of Lille University Hospital.
2.6. Agreement of the subjects
During a medical interview, participants received oral and written information detailing the progress of the trial and were allowed a period of reflection. Informed consent was collected from each subject before they entered the study.
2.7. Choice of the follow-up
The duration of the program was 6 weeks (5 sessions, one session per week). We therefore carried out the posttreatment evaluation 2 months after inclusion to provide slight flexibility in the planning of the sessions. The 6-month evaluation is the reference generally found in the literature for follow-up measurement.
2.8. Intervention
The content of the 2 programs was identical: one was delivered by computer and the other through face-to-face sessions. A more detailed description of the Seren@ctif content is provided in Supp Table 1.
2.8.1. Face-to-face CBT
The program included 5 weekly individual sessions lasting 45 min or 1 h with trained clinical psychologists (graduate of a master's program in cognitive and emotional therapy with a minimum of 1 year of practice in CBT and cognitive behavioral stress management). Information, exercises, and homework assignments were delivered by the therapist without self-help support. At the beginning of each session, the therapist asked the participant about adverse events and changes in drug doses since the last session.
2.8.2. Blended CBT
The program included 5 weekly individual sessions lasting for 1 h that patients completed on a computer in our unit. They performed each session via self-help supports (videos, audio files, e-books, exercises, etc.) delivered on a USB key to avoid connection problems. The subjects benefited from a short intervention of 10 min on average with a nurse (5 min before the e-learning session and 5 min after the e-learning session). The aim of this face-to-face contact was to provide adherence-focused guidance (by strengthening the social presence) and technical-focused guidance. The nurse investigated the adverse events and drug dose changes since the last session, answered any questions, discussed the progress of the session, and possibly guided participants in the navigation of the computer program. The patient was encouraged to practice 1 or more daily exercises for 20 min each on 5 or 6 days of the week. For home training between sessions, patients could use a website via a username and a password that was previously given to them.
2.8.3. Wait-list control group (WLC)
Control group patients received usual care, consisting of contact with their general practitioner. After the 2-month evaluation, they were able to choose one of the two therapeutic programs.
2.9. Outcome measures
Given that ADA is a reactional disorder that raises diagnostic problems, the symptoms are not precisely described as in anxiety disorders (for example, as in generalized anxiety disorder). The approach used for assessment of ADA must therefore be multidimensional (measurement of several dimensions of stress and anxiety).
The primary outcome measure for the current study was the State-Trait Anxiety Inventory-Trait (STAI-T) (Spielberger, 1983). This is a 20-item questionnaire with 4 levels of ratings (from 1 = not at all to 4 = much; total score of 20 to 80) that captures how the subjects generally feel (9 reverse-scored items). The higher the score is, the higher the level of anxiety.
The following instruments served as secondary outcome measures. The Hospital Anxiety Depression Scale (HADS) (Zigmond and Snaith, 1983) is a questionnaire that assesses anxiety and depressive disorders using 14 items rated on a 0-to-3 scale, with 7 questions related to anxiety (total A) and 7 questions related to depressive symptoms (total D). A score between 8 and 10 on each of the subscales is considered to indicate a risk (possible or probable) of anxiety or depressive disorders.
The Penn State Worry Questionnaire (PSWQ) (Meyer et al., 1990) is a self-assessment questionnaire consisting of 16 items measuring the general tendency to worry, with answers based on a 5-point Likert scale ranging from 1 = not at all characteristic to 5 = extremely characteristic (scores range from 16 to 80). The higher the score is, the higher the level of worry.
The Perceived Stress Scale (PSS) (Cohen et al., 1983) comes from the stress transactional model and contains 14 items. The total score ranges from 0 to 56, and a higher score represents a higher stress level. Two dimensions emerge from this scale: perceived threat and perceived personal effectiveness.
A visual analog scale is often used to measure the intensity of various symptoms, especially pain. The visual analog scale for stress (VAS-stress) (Lesage et al., 2012) was used for the first time in 1996 for a subjective assessment of stress. It comprises a horizontal segment whose ends are defined as the limits of the parameter to be measured (from 0 = no stress to 100 = maximum stress).
The abbreviated Beck Depression Inventory (BDI) (Beck et al., 1961) is a self-assessment questionnaire measuring the severity of depression with 13 items rated from 0 to 3. The higher the score is, the higher the level of depression.
The VAS for satisfaction (from 0 = not at all satisfied to 100 = very satisfied) was used to measure the subjects' overall satisfaction with the two therapeutic programs.
3. Statistical analysis
A total of 120 patients (40 per group) were required to have a statistical power of 80% with a two-sided alpha level of 0.025 to show a mean difference of 11.5 in the 2-month STAI change between each experimental group and the WLC group. The sample size was calculated by assuming a standard deviation of 14.6 in the 2-month STAI change and considering 20% missing data (the study protocol paper provides more details).
All statistical analyses were performed independently in the Department of Biostatistics of the University Hospital of Lille by using SAS 9.4 (SAS Institute Inc) software. Qualitative variables were expressed as frequencies and percentages. Quantitative variables were described either by the mean and standard deviation in case of a Gaussian distribution or by the median and interquartile range if not. The normality of the distributions was verified graphically and by the Shapiro-Wilk test. The qualitative variables were described by the numbers and percentages of each category. Patient characteristics at baseline were described for each of the 3 arms. All analyses for the primary and secondary objectives were performed on all randomized patients in their original group of randomization according to intention-to-treat (ITT) principles. All statistical tests between each experimental group and control group were 2-sided at the 2.5% significance level; all other statistical tests were 2-sided at the 5% significance level. No adjustment for multiple testing regarding the number of secondary outcomes was applied, and thus, all secondary objectives are considered exploratory.
Comparisons of 2-month changes from baseline in primary and secondary outcomes between each experimental group and the control group were performed using the constrained longitudinal data analysis (cLDA) model proposed by Liang and Zeger. We choose to use the cLDA model regarding the potential advantages of this model compared to the conventional longitudinal analysis of covariance (ANCOVA) model (Liu et al., 2009). In the cLDA, both the baseline and post-baseline values are modeled as dependent variables using a linear mixed model (an unstructured covariance pattern model), and the true baseline means are constrained to be the same for the 3 groups. Hence, the cLDA provides an adjustment for the baseline values in estimating the treatment effect. The treatment effect (mean difference in 2-month changes between groups) was estimated by the time-by-arm interaction.
Comparisons of 2- and 6-month changes from baseline in primary and secondary outcomes between the two experimental groups were also performed using cLDA models.
Finally, we assessed the change in scores (primary and secondary outcomes) from 2-month to 6-month visits separately in each experimental group by using a linear mixed model (an unstructured covariance pattern model) including the 3 repeated measures (baseline, 2-month, 6 month); post hoc comparisons between 2- and 6-month visits were performed using linear contrast. The same methodology was used to assess the change in scores between 2 months and 6 months in patients from the control group who chose face-to-face CBT at the 2-month visit.
For primary and secondary efficacy analyses, missing outcome values were handled by multiple imputation procedures. Missing data were imputed under the missing-at-random assumption using a regression-switching approach (chained equation with m = 20 imputations) with a predictive mean matching method for continuous variables and logistic regression (binary, ordinal, or polynomial) for qualitative variables (Buuren and Groothuis-Oudshoorn, 2011). The imputation procedure was performed using the main baseline characteristics, outcomes, and allocated group, and the estimates obtained in the different imputed data sets were combined using Rubin's rules (Rubin, 1989; Li et al., 1991). Sensitivity efficacy analyses were conducted for the primary outcome by using all available STAI measurements (complete case analysis) and by excluding patients with major protocol deviations (per-protocol analysis).
4. Results
4.1. Baseline characteristics
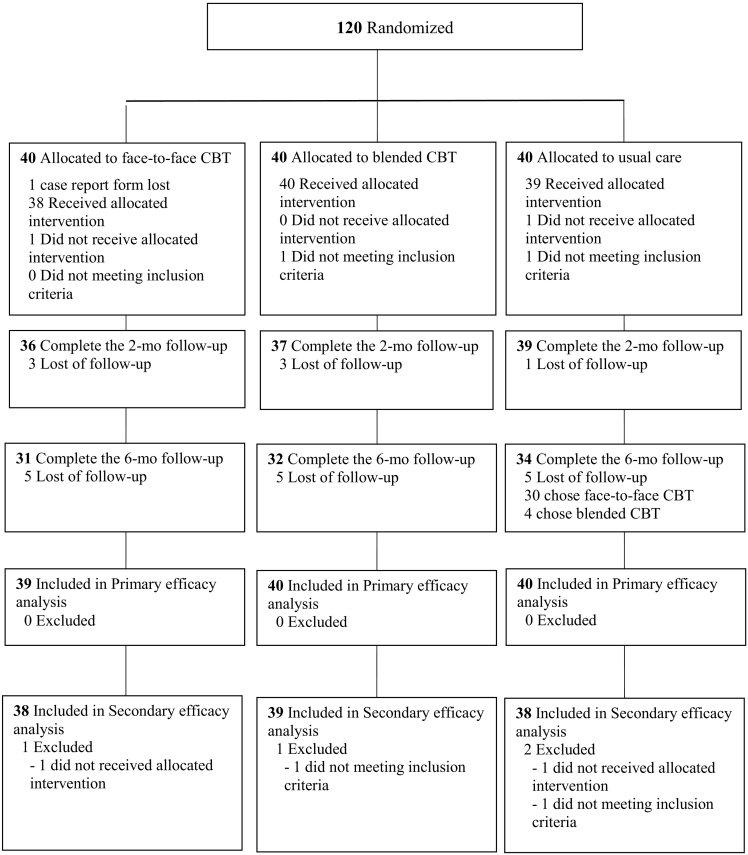
A total of 120 patients were included from January 2016 to October 2018 and were randomly assigned to either face-to-face CBT, blended CBT or a wait-list control (WLC) condition (Fig. 1). Of these patients, one patient (allocated to face-to-face CBT) was excluded from the primary efficacy analysis due to the loss of the case report form. The clinical and sociodemographic characteristics of the 119 patients included in the primary efficacy analysis are presented in Table 1, overall and according to the allocated arm. A total of 64.7% of the patients were women, and the most common cause of ADA was stress at work (76.5%). Managerial staff is the most represented socio-professional category (31.1%). There were no major differences between the 3 groups at baseline. We can note a small imbalance in socio-professional categories, with a less active population in the WLC arm.
Fig. 1.
Study flow chart.
Table 1.
Clinical and sociodemographic characteristics.
| Variables | Overall N = 119 |
Face-to-face CBT N = 39 |
Blended CBT N = 40 |
WLC N = 40 |
|---|---|---|---|---|
| Men, n(%) | 42 (35.3) | 14 (35.9) | 14 (35.0) | 14 (35.0) |
| Age, year, mean ± SD | 37.9 ± 10.2 | 37.3 ± 9.3 | 37.4 ± 11.6 | 39.1 ± 9.7 |
| Socio-professional category, n (%) | ||||
| Farmers | 1 (0.9) | 1 (2.6) | 0 (0.0) | 0 (0.0) |
| Craftsmen | 4 (3.5) | 2 (5.1) | 1 (2.7) | 1 (2.6) |
| Managerial staff | 41 (36.0) | 12 (30.8) | 13 (35.1) | 16 (42.1) |
| Intermediate professions | 15 (13.1) | 7 (17.9) | 5 (13.5) | 3 (7.9) |
| Employees | 37 (32.4) | 12 (30.8) | 9 (24.3) | 16 (42.1) |
| Workers | 15 (13.2) | 5 (12.8) | 8 (21.6) | 2 (5.3) |
| Other | 1 (0.9) | 0 (0.0) | 1 (2.7) | 0 (0.0) |
| Active population, n(%) | 96 (82.8) | 36 (92.3) | 31 (81.6) | 29 (74.4) |
| Cause of ADA | ||||
| Work | 91 (76.5) | 30 (76.9) | 29 (72.5) | 32 (80.0) |
| Family | 23 (19.3) | 11 (28.2) | 7 (17.5) | 5 (12.5) |
| Health | 19 (16.0) | 8 (20.5) | 7 (17.5) | 4 (10.0) |
| Sentimental life | 18 (15.1) | 5 (12.8) | 8 (20.0) | 5 (12.5) |
| Finances | 8 (6.7) | 2 (5.1) | 3 (7.5) | 3 (7.5) |
| Friends | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Legal issues | 2 (1.7) | 1 (2.6) | 0 (0.0) | 1 (2.5) |
| Transport network | 2 (1.7) | 1 (2.6) | 1 (2.5) | 0 (0.0) |
| Maintenance | 5 (4.2) | 0 (0.0) | 3 (7.5) | 2 (5.0) |
| Hobbies | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Other causes | 19 (16.0) | 7 (17.9) | 6 (15.0) | 6 (15.0) |
4.2. Effectiveness of the two therapeutic programs after 2 months of treatment on the primary outcome measure (primary objective)
As presented in Table 2, the State-Trait Anxiety Inventory score improved significantly in the two therapeutic groups after two months of treatment compared to in the control group, with a mean absolute change of −11.7 (95% CI, −16.0 to −7.4) in the CBT group, −15.8 (95% CI, −19.1 to −12.6) in the blended CBT group and −0.5 (95% CI, −2.9 to 1.9) in the WLC group. The effect size (mean between-group difference in change using the WLC group as the control) associated with face-to-face CBT was −11.0 (95% CI, −15.5 to −6.5; p < 0.001), and the effect size associated with blended CBT was −14.1 (95% CI, −18.6 to −9.7; p < 0.001). The same results were obtained in per-protocol analyses and in complete case analyses (see Supp Table 2).
Table 2.
Comparisons of change scores from baseline to 2 months between controls and the two experimental groups.
| Variables | WLC |
Face-to-face CBT |
Difference with controls in change from baseline, adjusted for baseline value |
Blended CBT |
Difference with controls in change from baseline, adjusted for baseline value |
||
|---|---|---|---|---|---|---|---|
| Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | p-value | Mean (95%CI) | Mean (95%CI) | p-value | |
| STAI | |||||||
| Baseline | 54.7 (51.8 to 57.5) | 55.2 (52.1 to 58.2) | 57.9 (55.3 to 60.4) | ||||
| 2 months | 54.2 (51.3 to 57.1) | 43.5 (39.4 to 47.7) | 42.0 (38.5 to 45.5) | ||||
| Change | −0.5 (−2.9 to 1.9) | −11.7 (−16.0 to −7.4) | −11.0 (−15.5 to −6.5) | <0.001 | −15.8 (−19.1 to −12.6) | −14.1 (−18.6 to −9.7) | <0.001 |
| Anxiety HAD | |||||||
| Baseline | 12.6 (11.9 to 13.3) | 13.3 (12.5 to 14.2) | 14.1 (13.2 to 14.9) | ||||
| 2 months | 12.5 (11.4 to 13.5) | 9.1 (8.0 to 10.2) | 8.6 (7.7 to 9.5) | ||||
| Change | −0.1 (−0.9 to 0.7) | −4.1 (−5.1 to −3.1) | −3.8 (−5.0 to −2.6) | <0.001 | −5.4 (−6.4 to −4.4) | −4.9 (−6.1 to −3.7) | <0.001 |
| Depression HAD | |||||||
| Baseline | 5.6 (4.8 to 6.4) | 5.9 (5.1 to 6.7) | 6.3 (5.5 to 7.0) | ||||
| 2 months | 5.9 (4.9 to 6.8) | 5.2 (3.9 to 6.5) | 3.4 (2.5 to 4.3) | ||||
| Change | 0.3 (−0.6 to 1.2) | −0.7 (−1.9 to 0.5) | −0.8 (−2.1 to 0.5) | 0.41 | −2.9 (−3.7 to −2.1) | −2.8 (−4.2 to −1.6) | <0.001 |
| Score PSS | |||||||
| Baseline | 47.0 (44.8 to 49.1) | 47.7 (45.7 to 49.7) | 47.9 (45.5 to 50.2) | ||||
| 2 months | 46.1 (44.2 to 48.1) | 39.4 (36.5 to 42.4) | 38.2 (35.9 to 40.4) | ||||
| Change | −0.8 (−2.7 to 1.0) | −8.3 (−11.0 to −5.5) | −7.0 (−10.0 to −4.0) | <0.001 | −9.7 (−12.2 to −7.2) | −8.4 (−11.4 to −5.4) | <0.001 |
| Score PSWQ | |||||||
| Baseline | 47.0 (44.9 to 49.0) | 47.4 (45.5 to 49.4) | 48.4 (46.8 to 50.0) | ||||
| 2 months | 46.2 (44.5 to 47.9) | 43.4 (41.1 to 45.7) | 42.3 (40.5 to 44.0) | ||||
| Change | −0.8 (−2.8 to 1.2) | −4.0 (−6.2 to −1.9) | −3.0 (−5.5 to −0.5) | 0.034 | −6.1 (−7.9 to −4.4) | −4.7 (−7.1 to −2.2) | <0.001 |
| Score BDI | |||||||
| Baseline | 7.8 (6.4 to 9.1) | 8.9 (7.3 to 10.4) | 9.4 (7.6 to 11.1) | ||||
| 2 months | 7.5 (6.1 to 8.8) | 6.1 (4.5 to 7.6) | 6.1 (4.6 to 7.6) | ||||
| Change | −0.3 (−1.5 to 0.9) | −2.8 (−4.5 to −1.2) | −2.0 (−3.7 to −0.4) | 0.032 | −3.2 (−4.5 to −2.0) | −2.3 (−4.0 to −0.6) | 0.014 |
| VAS-stress | |||||||
| Baseline | 71.7 (66.8 to 76.5) | 73.8 (69.0 to 78.6) | 75.1 (71.4 to 78.8) | ||||
| 2 months | 66.9 (62.1 to 71.7) | 38.5 (30.6 to 46.5) | 34.9 (28.9 to 40.8) | ||||
| Change | −4.8 (−9.9 to 0.3) | −35.2 (−43.1 to −27.4) | −29.1 (−37.9 to −20.4) | <0.001 | −40.3 (−46.7 to −33.8) | −34.0 (−42.4 to −25.6) | <0.001 |
Note. 95%CI: 95% Confidence Interval. Values are reported after handling missing values by multiple imputations. Bonferroni correction was applied for all comparisons. STAI: State Trait Anxiety Inventory; Anxiety HAD: Hospital Anxiety Depression scale - Anxiety subscale; Depression HAD: Hospital Anxiety Depression scale – Depression subscale; PSS: Perceived Stress Scale; PSWQ: Pen State Worry Questionnaire; BDI: Beck Depression Inventory; VAS-stress: Visual Analog Scale – stress.
4.3. Effectiveness of the two therapeutic programs after 2 months of treatment on the secondary outcome measures (secondary objective 1)
As presented in Table 2, a significant improvement in all the other self-report scales in favor of two intervention arms (face-to-face CBT and blended CBT) compared to the control arm was also found, except for the effect of face-to-face CBT on the HADS depression subscale. Indeed, subjects in the face-to-face CBT group did not significantly improve their scores at 2 months on this subscale (mean absolute change of −0.7 (95% CI, −1.9 to 0.5)) compared to subjects in the control group (mean absolute change, 0.3 (95% CI, −0.6 to 1.2); mean between-group difference, −0.8 (95% CI, −2.1 to 0.5), p = 0.41).
4.4. Comparisons between the two therapeutic groups of the outcome measures after two months of treatment and 6 months after the end of the treatment (secondary objective 2)
As presented in Table 3, no significant difference was found between the two therapeutic groups on the State-Trait Anxiety Inventory after 2 months of treatment (mean between-group difference, −3.2 (95% CI, −7.8 to 1.3), p = 0.16) and at 6 months posttreatment (mean between-group difference, −4.6 (95% CI, −10.3 to 1.1), p = 0.12). No significant difference was found between the face-to-face CBT and blended CBT groups on the HADS anxiety subscale score after 2 months of treatment (mean between-group difference, −1.1 (95% CI, −2.3 to 0.1), p = 0.076); however, there was a significant difference between the two groups at 6 months posttreatment. Indeed, the mean absolute change between baseline and 6 months following the treatment was −6.2 (95% CI, −7.2 to −5.3) in the blended CBT group (falling below the risk threshold for developing an anxiety or depressive disorder (<8)), while the mean absolute change between baseline and 6 months following the treatment was −3.6 (95% CI, −4.6 to −2.6) in the face-to-face CBT group (mean between-group difference, −2.2 (95% CI, −3.8 to −0.7), p = 0.004). A significant difference between the two therapeutic groups was found in the change from baseline on the HADS depression subscale score after 2 months of treatment (mean between-group difference, −2.1 (95% CI, −3.4 to −0.7), p = 0.003). This significant difference remained at 6 months posttreatment (mean between-group difference, −1.8 (95% CI, −3.2 to 0.4), p = 0.014). No significant difference was found between the face-to-face CBT and blended CBT groups on the Perceived Stress Scale, neither after 2 months of treatment (p = 0.36) nor at 6 months following the treatment (p = 0.76). No significant difference was found between the face-to-face CBT and blended CBT groups on the Penn State Worry Questionnaire, the Beck Depression Inventory and the visual analog scale for stress at 2 months and 6 months after treatment.
Table 3.
Comparisons of change scores from baseline between face-to-face CBT group and blended CBT group.
| Variables | Face-to-face CBT |
Blended CBT |
Difference in change from baseline, adjusted for baseline value |
|
|---|---|---|---|---|
| Mean (95%CI) | Mean (95%CI) | Mean (95%CI) | p-value | |
| STAI | ||||
| Baseline | 55.2 (52.1 to 58.2) | 57.9 (55.3 to 60.4) | ||
| 2 months | 43.5 (39.4 to 47.7) | 42.0 (38.5 to 45.5) | ||
| 6 months | 43.5 (38.7 to 48.3) | 39.8 (36.2 to 43.3) | ||
| Change (2 months – baseline) | −11.7 (−16.0 to −7.4) | −15.8 (−19.1 to −12.6) | −3.2 (−7.8 to 1.3) | 0.16 |
| Change (6 months – baseline) | −11.7 (−16.2 to −7.1) | −18.1 (−21.7 to −14.4) | −4.6 (−10.3 to 1.1) | 0.12 |
| HAD anxiety | ||||
| Baseline | 13.3 (12.5 to 14.2) | 14.1 (13.2 to 14.9) | ||
| 2 months | 9.1 (8.0 to 10.2) | 8.6 (7.7 to 9.5) | ||
| 6 months | 9.7 (8.3 to 11.1) | 7.8 (6.9 to 8.8) | ||
| Change (2 months – baseline) | −4.1 (−5.1 to −3.1) | −5.4 (−6.4 to −4.4) | −1.1 (−2.3 to 0.1) | 0.076 |
| Change (6 months – baseline) | −3.6 (−4.6 to −2.6) | −6.2 (−7.2 to −5.3) | −2.2 (−3.8 to −0.7) | 0.004 |
| HAD depression | ||||
| Baseline | 5.9 (5.1 to 6.7) | 6.3 (5.5 to 7.0) | ||
| 2 months | 5.2 (3.9 to 6.5) | 3.4 (2.5 to 4.3) | ||
| 6 months | 4.9 (3.5 to 6.2) | 3.3 (2.3 to 4.3) | ||
| Change (2 months – baseline) | −0.7 (−1.9 to 0.5) | −2.9 (−3.7 to −2.1) | −2.1 (−3.4 to −0.7) | 0.003 |
| Change (6 months – baseline) | −1.1 (−2.4 to 0.2) | −3.0 (−3.9 to −2.1) | −1.8 (−3.2 to 0.4) | 0.014 |
| Score PSS | ||||
| Baseline | 47.7 (45.7 to 49.7) | 47.9 (45.5 to 50.2) | ||
| 2 months | 39.4 (36.5 to 42.4) | 38.2 (35.9 to 40.4) | ||
| 6 months | 46.7 (44.9 to 48.5) | 47.0 (45.6 to 48.4) | ||
| Change (2 months – baseline) | −8.3 (−11.0 to −5.5) | −9.7 (−12.2 to −7.2) | −1.4 (−4.5 to 1.6) | 0.36 |
| Change (6 months – baseline) | −1.0 (−3.8 to 1.8) | −0.9 (−3.4 to 1.7) | 0.3 (−1.9 to 2.6) | 0.76 |
| Score PSWQ | ||||
| Baseline | 47.4 (45.5 to 49.4) | 48.4 (46.8 to 50.0) | ||
| 2 months | 43.4 (41.1 to 45.7) | 42.3 (40.5 to 44.0) | ||
| 6 months | 43.4 (40.9 to 45.9) | 41.4 (39.3 to 43.5) | ||
| Change (2 months – baseline) | −4.0 (−6.2 to −1.9) | −6.1 (−7.9 to −4.4) | −1.7 (−4.3 to 0.9) | 0.19 |
| Change (6 months – baseline) | −4.0 (−6.2 to −1.8) | −7.0 (−8.9 to −5.2) | −2.4 (−5.5 to 0.6) | 0.11 |
| Score BDI | ||||
| Baseline | 8.9 (7.3 to 10.4) | 9.4 (7.6 to 11.1) | ||
| 2 months | 6.1 (4.5 to 7.6) | 6.1 (4.6 to 7.6) | ||
| 6 months | 5.5 (3.6 to 7.3) | 3.9 (2.9 to 4.9) | ||
| Change (2 months – baseline) | −2.8 (−4.5 to −1.2) | −3.2 (−4.5 to −2.0) | −0.3 (−2.0 to 1.4) | 0.74 |
| Change (6 months – baseline) | −3.4 (−5.3 to −1.5) | −5.4 (−6.6 to −4.2) | −1.7 (−3.6 to 0.2) | 0.078 |
| VAS-stress | ||||
| Baseline | 73.8 (69.0 to 78.6) | 75.1 (71.4 to 78.8) | ||
| 2 months | 38.5 (30.6 to 46.5) | 34.9 (28.9 to 40.8) | ||
| 6 months | 39.1 (30.4 to 47.7) | 32.2 (25.4 to 39.1) | ||
| Change (2 months – baseline) | −35.2 (−43.1 to −27.4) | −40.3 (−46.7 to −33.8) | −4.8 (−13.4 to 3.7) | 0.27 |
| Change (6 months – baseline) | −34.8 (−43.5 to −26.1) | −42.9 (−49.4 to −36.4) | −7.1 (−18.0 to 3.8) | 0.20 |
Note. 95%CI: 95% Confidence Interval. Values are reported after handling missing values by multiple imputations. STAI: State Trait Anxiety Inventory; Anxiety HAD: Hospital Anxiety Depression scale - Anxiety subscale; Depression HAD: Hospital Anxiety Depression scale – Depression subscale; PSS: Perceived Stress Scale; PSWQ: Pen State Worry Questionnaire; BDI: Beck Depression Inventory; VAS-stress: Visual Analog Scale – stress.
4.5. Evolution of the outcome measures between 2 and 6 months posttreatment for the two therapeutic groups separately (secondary objective 3)
As presented in Table 4, no significant difference in the scores between 2 and 6 months following the treatment was found on all self-report scales, except for the Perceived Stress Scale in each therapeutic group (mean absolute change of 7.5 (95% CI, 3.5 to 11.6) in the face-to-face CBT group and mean absolute change of 8.7 (95% CI, 5.6 to 11.7) in the blended CBT group) and for the Beck Depression Inventory in the blended CBT group only (the latter continued to show improvements in its score at the 6-month visit compared to the 2-month visit, decreasing from 6.1 to 3.7). For this group, the BDI score ranges from the category “mild depression” at the 2-month follow-up to “absence of depression” at the 6-month follow-up.
Table 4.
Change score between 2 and 6 months in the face-to-face CBT group and the blended CBT group separately.
| Variables | Face-to-face CBT |
Blended CBT |
||||
|---|---|---|---|---|---|---|
| N | Mean (95%CI) | p-value | N | Mean (95%CI) | p-value | |
| STAI | ||||||
| 2 months | 36 | 43.3 (38.9 to 47.6) | 37 | 42.0 (38.3 to 45.7) | ||
| 6 months | 31 | 44.2 (38.9 to 49.5) | 32 | 39.5 (36.0 to 42.9) | ||
| Change (6–2 months) | 31 | 2.4 (−2.1 to 7.0) | 0.28 | 32 | −1.9 (−5.5 to 1.8) | 0.30 |
| HAD anxiety | ||||||
| 2 months | 36 | 9.2 (8.0 to 10.4) | 36 | 8.4 (7.6 to 9.2) | ||
| 6 months | 31 | 9.7 (8.0 to 11.3) | 32 | 7.7 (6.7 to 8.6) | ||
| Change (6–2 months) | 31 | 0.9 (−0.4 to 2.3) | 0.17 | 32 | −0.6 (−1.5 to 0.3) | 0.17 |
| HAD depression | ||||||
| 2 months | 36 | 5.3 (3.8 to 6.7) | 36 | 3.4 (2.4 to 4.3) | ||
| 6 months | 31 | 4.8 (3.3 to 6.2) | 32 | 3.1 (2.1 to 4.1) | ||
| Change (6–2 months) | 31 | −0.1 (−1.6 to 1.3) | 0.86 | 32 | −0.2 (−1.0 to 0.7) | 0.69 |
| Score PSS | ||||||
| 2 months | 36 | 39.6 (36.5 to 42.8) | 37 | 37.8 (35.5 to 40.2) | ||
| 6 months | 31 | 46.9 (44.9 to 48.8) | 32 | 46.9 (45.6 to 48.2) | ||
| Change (6–2 months) | 31 | 7.5 (3.5 to 11.6) | <0.001 | 32 | 8.7 (5.6 to 11.7) | <0.001 |
| Score QIPS | ||||||
| 2 months | 36 | 43.4 (41.0 to 45.7) | 37 | 42.1 (40.2 to 44.0) | ||
| 6 months | 31 | 43.1 (40.4 to 45.8) | 32 | 40.6 (38.4 to 42.9) | ||
| Change (6–2 months) | 31 | 0.1 (−2.4 to 2.5) | 0.97 | 32 | −1.4 (−3.7 to 0.9) | 0.23 |
| Score BDI | ||||||
| 2 months | 36 | 6.2 (4.5 to 7.9) | 37 | 6.1 (4.5 to 7.6) | ||
| 6 months | 31 | 5.6 (3.6 to 7.6) | 32 | 3.7 (2.7 to 4.7) | ||
| Change (6–2 months) | 31 | 0.1 (−1.6 to 1.7) | 0.95 | 32 | −2.3 (−3.7 to −0.9) | 0.002 |
| VAS-stress | ||||||
| 2 months | 36 | 38.6 (30.4 to 46.9) | 37 | 33.9 (27.8 to 40.0) | ||
| 6 months | 31 | 40.2 (31.3 to 49.1) | 32 | 31.5 (24.0 to 39.0) | ||
| Change (6–2 months) | 31 | 3.2 (−6.0 to 12.3) | 0.48 | 32 | −2.4 (−10.1 to 5.4) | 0.54 |
Note. 95%CI: 95% Confidence Interval. STAI: State Trait Anxiety Inventory; Anxiety HAD: Hospital Anxiety Depression scale - Anxiety subscale; Depression HAD: Hospital Anxiety Depression scale – Depression subscale; PSS: Perceived Stress Scale; PSWQ: Pen State Worry Questionnaire; BDI: Beck Depression Inventory; VAS-stress: Visual Analog Scale – stress.
4.6. Comparison of global satisfaction between the two experimental groups (secondary objective 4)
Regarding global satisfaction, no significant difference was found between the face-to-face CBT and blended CBT groups after either two months of treatment (76.6 ± 18.3 vs 77.5 ± 14.7; p = 0.81) or 6 months following the treatment (73.1 ± 20.8 vs 78.8 ± 13.6; p = 0.21).
4.7. Additional analysis for the subjects of the control group having chosen face-to-face cognitive behavioral therapy
Among the subjects of the control group, 30/39 chose to receive face-to-face CBT. After the treatment, the subjects of the control group significantly improved their scores on all self-report scales except for the Perceived Stress Scale. Indeed, the PSS score remained the same at 6 months compared to the PSS score at 2 months (p = 0.33) (Supp Table 3).
5. Discussion
This study confirms that a CBT intervention is clearly effective for treating ADA and supports the efficacy of an internet intervention. Face-to-face CBT and blended CBT are both effective in reducing anxiety, depression, worry and perceived stress after two months of treatment in patients with a strict diagnosis of ADA according to the DSM-5. These improvements are maintained at the 6-month follow-up on most scales. Surprisingly, blended CBT showed significantly greater reductions in the HADS depression subscale scores at 2 months and 6 months and in the HADS anxiety subscale scores at 6 months compared to face-to-face CBT on these secondary outcome measures.
These findings suggest that the superiority of blended CBT may be interpreted with caution. Indeed, we considered patients with adjustment disorder with anxiety, and we excluded patients with adjustment disorder with depressive mood and with mixed anxiety and depressive mood. Changes in HADS depression subscale scores in the normal range (<7) are less studied in depressive patients under treatment and are more difficult to interpret.
However, the BDI scores continued to improve at 6 months compared to 2 months for the blended CBT group only, while for the face-to-face CBT group, the BDI scores remained stable and may indicate an improvement in mood.
Regarding anxiety, although the results of STAI are not significant, there is a greater decrease at 2 months and 6 months, suggesting superiority in the blended group.
The superiority of these results regarding the blended CBT compared to the face-to-face CBT could be explained by the unlimited access to the sessions on the platform during the study. Indeed, patients could return on each session as many times as they wanted by logging into the online platform from their home. Moreover, given that patients in the blended CBT group were able to use the platform for their home training, they could use it at the end of the treatment between the 2-month visit and the 6-month visit, thus further improving their anxiety and depression scores. This ability to perform each session without pressure and to practice the exercises in the order and timing that they preferred could have positively impacted their mood and decreased their anxiety more profoundly than their ability to perform each face-to-face CBT session only once.
An unexpected result is a significant increase in the Perceived Stress Scale at the 6-month visit compared to the 2-month visit for the two experimental groups. In internet-based cognitive behavioral stress management programs, the PSS is the main criterion that improves after intervention and is maintained at follow-up (Heber et al., 2017). Increasing PSS scores in patients with ADA could be explained by the fact that stressors may persist or be reactivated even if patients continue to manage pathological anxiety. It seems important to evaluate stressful events in patients even if they no longer respond to the diagnosis of ADA. This explanation remains unclear, but the hypothesis that stress and anxiety are not always exactly correlated is possible.
This study is important because it provides new data in an area with a lack of clinical trials. This study suggests that in the psychological treatment of ADA, blended CBT may be equivalent or even slightly more effective than classical face-to-face intervention, which is the first-line recommendation. This finding is an important contribution because very few studies have compared a guided internet intervention with the same face-to-face intervention (Andersson et al., 2014).
It is also an interesting result because this blended CBT offered the advantage of reducing the amount of time spent on each patient by health professionals by 6 times compared to face-to-face CBT and could therefore be a more cost-effective solution. In France, access to CBT in psychiatry services is limited because healthcare professionals lack time for psychotherapy. A blended intervention that combines an online approach with a limited amount of time spent with a healthcare professional may be of great interest to improve access to CBT. Blended interventions may offer advantages for psychiatric patients with ADA who need human contact instead of traditional guidance by phone call or by email exchange. It may be in these situations that iCBT interventions are ideal, as they are equivalent to or more effective than face-to-face CBT, as well as more cost-effective.
Given the current context linked to the COVID-19 health crisis, the frequency of patients suffering from ADA will increase in the coming months and years. Psychiatry teams will be overwhelmed, which will lead to patients waiting longer for access to effective management of stress and anxiety. Blended CBT for ADA could provide more patients and caregivers with access to effective stress, anxiety and depression management.
A limitation of this study is the absence of a measure of adherence regarding home training between sessions and between the 2-month and 6-month visits. It would have been interesting to measure, for example, the number of exercise sessions performed, the time spent practicing daily exercises, the number of times participants logged on to the platform and the length of time they spent connected to the platform.
Moreover, even if we found no significant differences between the two experimental groups on global satisfaction, on a single VAS scale, it is difficult to interpret the meaning of global satisfaction, as satisfaction with a treatment may be comprised of several components (e.g., content delivered, format delivered, therapist relationship, frequency of visits).
Another limitation of this study is the lack of an MINI during posttreatment evaluations. Although anxiety and perceived stress improved at the end of the study, suggesting that patients no longer responded to the diagnosis of ADA, a MINI at 2-month and 6-month evaluations posttreatment may confirm that patients no longer responded to the diagnostic criteria according to the DSM-5. The identification of stressors at posttreatment is important to analyze increasing Perceived Stress Scores from 2 months to 6 months of evaluation.
Further studies are needed to replicate these findings in ambulatory psychiatric patients with ADA. Moreover, further work should be performed on the cost-effectiveness of face-to-face CBT versus blended CBT for ADA. Finally, a superiority study between face-to-face CBT and blended CBT for ADA could be conducted.
In the blended CBT intervention described in this study, patients had to move to ambulatory services to complete their sessions, which did not allow them to benefit from the main advantage of a guided internet-based intervention by telephone or e-mail. To improve this issue, human contact time could be provided by teleconsultation. Indeed, a randomized controlled trial has shown similar efficacy between CBT delivered in person or by videoconference in reducing symptoms of anxiety, stress and depression (Stubbings et al., 2013). Teleconsultation could then be an innovative internet solution that may enable patients to benefit from a blended intervention but in an entirely remote manner.
Future studies could also compare the effectiveness of blended CBT versus traditional guided iCBT and could evaluate whether blended CBT is a way to eliminate the negative effects sometimes found in unguided iCBT and traditional guided iCBT, such as nonresponse, deterioration, technical difficulties, implementation problems, negative emotional states or other adverse and unwanted events (Gullickson et al., 2019).
Finally, blended CBT may be evaluated in other psychiatric and stress-related pathologies.
6. Conclusions
The current study suggests that an internet-based CBT with human guidance by a healthcare professional (blended CBT) and the same program delivered face-to-face by a CBT therapist are both effective for patients with ADA in a psychiatric setting. Moreover, blended CBT seems to be at least as effective as the same face-to-face CBT program for patients with ADA in a psychiatric setting. Blended CBT may be a cost-effective alternative to face-to-face CBT for patients with a diagnosis of ADA and other pathologies. Finally, blended CBT could show significantly greater reductions in some psychological symptoms than other intervention formats, such as face-to-face CBT or traditional guided iCBT, for patients with a diagnosis of ADA and other pathologies.
Further work is needed to draw conclusions regarding these hypotheses.
Seren@ctif content.
Per protocol analysis and complete case analysis for primary outcome: STAI score.
Change scores between 2 and 6 months in the control group who have chosen face-to-face CBT after visit at 2 months.
Declaration of competing interest
None.
Authors certify that there is no conflict of interest related to the manuscript.
Acknowledgements
This trial was supported by funding from the French Ministry of Health (PHRC-I 2014-074). The study is sponsored by the University Hospital of Lille.
References
- American Psychiatric Association . 5th ed. American Psychiatric Association; Washington, D.C: 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. [Google Scholar]
- Andersson G., Cuijpers P., Carlbring P., Riper H., Hedman E. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 2014;13(3):288–295. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Titov N., Lindefors N. Internet interventions for adults with anxiety and mood disorders: a narrative umbrella review of recent meta-analyses. Can. J. Psychiatry. 2019;64(7):465–470. doi: 10.1177/0706743719839381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G., Basu A., Cuijpers P., Craske M.G., McEvoy P., English C.L., Newby J.M. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. Journal of Anxiety Disorders. 2018;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Attari A., Sartippour M., Amini M., Haghighi S. Effect of stress management training on glycemic control in patients with type 1 diabetes. Diabetes Res. Clin. Pract. 2006;73(1):23–28. doi: 10.1016/j.diabres.2005.11.014. [DOI] [PubMed] [Google Scholar]
- Baumeister H., Reichler L., Munzinger M., Lin J. The impact of guidance on internet-based mental health interventions—A systematic review. Internet Interv. 2014;1(4):205–215. doi: 10.1016/j.invent.2014.08.003. [DOI] [Google Scholar]
- Beck J. Guilford Press; 2011. Cognitive Behavior Therapy: Second Edition: Basics and beyond.https://www.guilford.com/books/Cognitive-Behavior-Therapy/Judith-Beck/9781609185046/reviews [Google Scholar]
- Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bhui K.S., Dinos S., Stansfeld S.A., White P.D. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J. Environ. Public Health. 2012;2012 doi: 10.1155/2012/515874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buuren S. van, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J. Stat. Softw. 2011;45(1):1–67. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- Campbell T.S., Stevenson A., Arena R., Hauer T., Bacon S.L., Rouleau C.R., Cannon C., Stone J.A. An investigation of the benefits of stress management within a cardiac rehabilitation population. Journal of Cardiopulmonary Rehabilitation and Prevention. 2012;32(5):296–304. doi: 10.1097/HCR.0b013e318265e0eb. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018;47(1):1–18. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- Casey P. Adjustment disorder: epidemiology, diagnosis and treatment. CNS Drugs. 2009;23(11):927–938. doi: 10.2165/11311000-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Casey P. Adjustment disorder: new developments. Current Psychiatry Reports. 2014;16(6):451. doi: 10.1007/s11920-014-0451-2. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cuijpers P., Donker T., van Straten A., Li J., Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol. Med. 2010;40(12):1943–1957. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- Cuijpers Pim, Sijbrandij M., Koole S., Huibers M., Berking M., Andersson G. Psychological treatment of generalized anxiety disorder: a meta-analysis. Clin. Psychol. Rev. 2014;34(2):130–140. doi: 10.1016/j.cpr.2014.01.002. [DOI] [PubMed] [Google Scholar]
- Eimontas J., Rimsaite Z., Gegieckaite G., Zelviene P., Kazlauskas E. Internet-based self-help intervention for ICD-11 adjustment disorder: preliminary findings. The Psychiatric Quarterly. 2018;89(2):451–460. doi: 10.1007/s11126-017-9547-2. [DOI] [PubMed] [Google Scholar]
- Erbe D., Eichert H.-C., Riper H., Ebert D.D. Blending face-to-face and internet-based interventions for the treatment of mental disorders in adults: systematic review. J. Med. Internet Res. 2017;19(9):e306. doi: 10.2196/jmir.6588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gullickson K.M., Hadjistavropoulos H.D., Dear B.F., Titov N. Negative effects associated with internet-delivered cognitive behaviour therapy: an analysis of client emails. Internet Interv. 2019;18 doi: 10.1016/j.invent.2019.100278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heber E., Ebert D.D., Lehr D., Cuijpers P., Berking M., Nobis S., Riper H. The benefit of web- and computer-based interventions for stress: a systematic review and meta-analysis. J. Med. Internet Res. 2017;19(2):e32. doi: 10.2196/jmir.5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsh A.T., Sears S.F., Conti J.B. Cognitive and behavioral treatments for anxiety and depression in a patient with an implantable cardioverter defibrillator (ICD): a case report and clinical discussion. J. Clin. Psychol. Med. Settings. 2009;16(3):270–279. doi: 10.1007/s10880-009-9160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagerveld S.E., Blonk R.W.B., Brenninkmeijer V., Wijngaards-de Meij L., Schaufeli W.B. Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J. Occup. Health Psychol. 2012;17(2):220–234. doi: 10.1037/a0027049. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y., Sheehan D., Weiller E., Amorim P., Bonora I., Harnett Sheehan K., Janavs J., Dunbar G. The MINI international neuropsychiatric interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. European Psychiatry. 1997;12(5):224–231. doi: 10.1016/S0924-9338(97)83296-8. [DOI] [Google Scholar]
- Lesage F.-X., Berjot S., Deschamps F. Clinical stress assessment using a visual analogue scale. Occupational Medicine (Oxford, England) 2012;62(8):600–605. doi: 10.1093/occmed/kqs140. [DOI] [PubMed] [Google Scholar]
- Li K.-H., Meng X.-L., Raghunathan T.E., Rubin D.B. Significance levels from repeated p-values with multiply-imputed datA. Stat. Sin. 1991;1(1):65–92. (JSTOR) [Google Scholar]
- Liu G.F., Lu K., Mogg R., Mallick M., Mehrotra D.V. Should baseline be a covariate or dependent variable in analyses of change from baseline in clinical trials? Stat. Med. 2009;28(20):2509–2530. doi: 10.1002/sim.3639. [DOI] [PubMed] [Google Scholar]
- Lopez C., Antoni M., Penedo F., Weiss D., Cruess S., Segotas M.-C., Helder L., Siegel S., Klimas N., Fletcher M.A. A pilot study of cognitive behavioral stress management effects on stress, quality of life, and symptoms in persons with chronic fatigue syndrome. J. Psychosom. Res. 2011;70(4):328–334. doi: 10.1016/j.jpsychores.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer T.J., Miller M.L., Metzger R.L., Borkovec T.D. Development and validation of the Penn State worry questionnaire. Behav. Res. Ther. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Moher D., Schulz K.F., Altman D.G. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet (London, England) 2001;357(9263):1191–1194. [PubMed] [Google Scholar]
- Mohr D.C., Cuijpers P., Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J. Med. Internet Res. 2011;13(1):e30. doi: 10.2196/jmir.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorey S., Greer S., Bliss J., Law M. A comparison of adjuvant psychological therapy and supportive counselling in patients with cancer. Psycho-Oncology. 1998;7(3):218–228. doi: 10.1002/(SICI)1099-1611(199805/06)7:3<218::AID-PON308>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- O’Donnell M.L., Metcalf O., Watson L., Phelps A., Varker T. A systematic review of psychological and pharmacological treatments for adjustment disorder in adults. J. Trauma. Stress. 2018;31(3):321–331. doi: 10.1002/jts.22295. [DOI] [PubMed] [Google Scholar]
- Otte C. Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues Clin. Neurosci. 2011;13(4):413–421. doi: 10.31887/DCNS.2011.13.4/cotte. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell S., McCone D. Treatment of adjustment disorder with anxiety: a September 11, 2001, case study with a 1-year follow-up. Cogn. Behav. Pract. 2004;11(3):331–336. doi: 10.1016/S1077-7229(04)80047-6. [DOI] [Google Scholar]
- Rubin D.B. Rubin, Donald B.: multiple imputation for nonresponse in surveys. John Wiley & Sons, Chichester – New York – Brisbane – Toronto – Singapore 1987, xxx, 258 S., 6 Abb., £ 30.25, ISSN 0271-6232. Biom. J. 1989;31(1):131–132. doi: 10.1002/bimj.4710310118. [DOI] [Google Scholar]
- Sauter S.L., Murphy L.R., Hurrell J.J. Prevention of work-related psychological disorders. A national strategy proposed by the National Institute for Occupational Safety and Health (NIOSH) The American Psychologist. 1990;45(10):1146–1158. doi: 10.1037//0003-066x.45.10.1146. [DOI] [PubMed] [Google Scholar]
- Servant D., Leterme A.-C., Barasino O., Rougegrez L., Duhamel A., Vaiva G. Efficacy of Seren@ctif, a computer-based stress management program for patients with adjustment disorder with anxiety: protocol for a controlled trial. JMIR Research Protocols. 2017;6(10):e190. doi: 10.2196/resprot.7976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E., Hergueta T., Baker R., Dunbar G.C. The Mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry. 1998;59(Suppl. 20):22–33. (quiz 34-57) [PubMed] [Google Scholar]
- Spielberger C. Consulting Psychologist Press; Palo Alto: 1983. Manual for the State-Trait Anxiety Inventory (Form Y) Self-Evaluation Questionnaire. [Google Scholar]
- Stubbings D.R., Rees C.S., Roberts L.D., Kane R.T. Comparing in-person to videoconference-based cognitive behavioral therapy for mood and anxiety disorders: randomized controlled trial. J. Med. Internet Res. 2013;15(11) doi: 10.2196/jmir.2564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N., Hadjistavropoulos H.D., Nielssen O., Mohr D.C., Andersson G., Dear B.F. From research to practice: ten lessons in delivering digital mental health services. J. Clin. Med. 2019;8(8) doi: 10.3390/jcm8081239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner L., Linden W., van der Wal R., Schamberger W. Stress management for patients with heart disease: a pilot study. Heart & Lung: The Journal of Critical Care. 1995;24(2):145–153. doi: 10.1016/s0147-9563(05)80009-3. [DOI] [PubMed] [Google Scholar]
- Wentzel J., van der Vaart R., Bohlmeijer E.T., van Gemert-Pijnen J.E.W.C. Mixing online and face-to-face therapy: how to benefit from blended care in mental health care. JMIR Mental Health. 2016;3(1):e9. doi: 10.2196/mental.4534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagorscak P., Heinrich M., Sommer D., Wagner B., Knaevelsrud C. Benefits of individualized feedback in internet-based interventions for depression: a randomized controlled trial. Psychother. Psychosom. 2018;87(1):32–45. doi: 10.1159/000481515. [DOI] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Seren@ctif content.
Per protocol analysis and complete case analysis for primary outcome: STAI score.
Change scores between 2 and 6 months in the control group who have chosen face-to-face CBT after visit at 2 months.