Abstract
Objectives
To combat SARS-CoV2 (Covid-19), policy makers worldwide have adopted different policy alternatives, often including mitigation/suppression policies. We assessed the economic impact of such policies on dental practices in Germany using a modelling approach.
Methods
A providers’ perspective within German healthcare was taken, with two provider scenarios (low/high volume practice, low/high proportion of non-statutory insurance revenue, low/high staff pool and costs; S1 and S2 scenarios) being modelled. Providers’ costs were estimated in different blocks (staff, material, laboratory, others). A telephone-based survey was conducted on 24th March to 2nd April 2020 on a random sample of 300 German dentists (response: n = 146) to determine the experienced dental services utilization changes in these service blocks. A Markov model was constructed, following 100 practices in each scenario for a total of 365 days. Different Covid-19 mitigation/suppression periods (90 days: base-case, 45, 135 days: sensitivity analyses) were modelled. Monte-Carlo micro-simulation was performed and uncertainty introduced via probabilistic and univariate sensitivity analyses.
Results
Mitigation/suppression reduced utilization of all services, the most severe for prevention (-80 % in mean), periodontics (-76 %) and prosthetics (-70 %). Within the base-case, mean revenue reductions were 18.7 %/15.7 % from the public insurance, 18.7/18.6 % from private insurers and 19 %/19 % for out-of-pocket expenses in S1/S2, respectively. If the mitigation/suppression was upheld for 135 days, overall revenue decreased by 31 %/30 % in S1/S2, respectively. In this case, 29 %/12 % S1/S2 would have a negative net profit over the course of one year.
Conclusions
Covid-19 and associated policies have profound economic effect on dental practices.
Clinical signifiance
Policy makers will want to consider our findings when designing governmental subsidy and safety nets with immediate and midterm economic relieve effects. Dentists may consider practice re-organization to reduce costs and maintain minimum profitability.
Keywords: Dental public health, Economic evaluation, Health services research, Infectious disease(s), Mathematic modelling, Practice management
1. Introduction
In Germany, around 850,000 jobs are associated with the more than 50,000 German dental practices [1]. Each dental practice is privately run for profit with a mean of five or more employees per licensed practice [2]. German dentistry is characterized by high practice costs (mean >330,000 Euro per licensed dentists and year), but also high revenue (mean >530,000 Euro). All dentists offer their patients services covered completely or partially by statutory, private, employed-based or other insurance schemes. Patients can top-up these insured services or pay completely out-of-pocket if requesting a qualitatively higher alternative of care [2].
More than 175 countries worldwide have reported cases of Covid-19. As of 8th April 2020, nearly 1,405,000 cases have been reported, and >82,000 deaths [3]. Governments have implemented strict policies to contain the pandemic, mainly by physical distancing including curfews. In Germany, federal state governments have implemented a range of mitigation and suppression policies, which have reduced mobility significantly [4].
These policies will have a profound impact on dental practices: On the demand side, patients’ services utilization is likely to contract short-term and shift towards public insurances as financial losses reduce the availability of disposable income for out-of-pocket spending. On the supply side, the pandemic may affect the availability of labor, impact on protocols to operate, alter the supply chain of materials and generate cash-flow problems.
Governments worldwide are not only aiming to reduce the spread of the pandemic, but to alleviate the economic burden of Covid-19. So far in Germany, dental practices have not been included in specific governmental support or protection schemes. We aimed to analyze the economic impact of Covid-19 on dental practices in Germany.
2. Methods
A modelling study was performed, which allows to vary input parameters in scenario and sensitivity analyses and thereby to gauge uncertainty and its impact as well as to extrapolate data into the future. Reporting of this study follows the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) [5].
2.1. Setting, perspective, population, horizon
This study adopted a dental providers’ perspective. In Germany, most individuals (>87 %) are publicly insured (statutory insurance) and only a minority is privately insured [6]; the latter group may benefit from complementary employer-based health insurance schemes. German insurances (except employer schemes) are largely financed by mandatory insurances contributions. For members of the statutory insurance, most dental procedures are covered; only few (e.g. preventive treatments in adults, prosthetics) need to be partially or fully paid out-of-pocket (or by private additional insurances). The private insurances and employer-based schemes usually have an even wider coverage, often fully covering also preventive treatments in adults and prosthetics.
We modelled a population of German dental practice providers (“practices”). To reflect on the different impact the Covid-19 mitigation/suppression policies have on different practices, two scenarios of practices (low/high volume practice, low/high proportion of non-statutory insurance revenue, low/high staff pool and costs) were modelled. The horizon of the study was 1 year, i.e. 365 days, assuming mitigation/suppression policies to conclude during this period. Modelling was performed using TreeAge Pro Healthcare 2020 (TreeAge Software, Williamstown, MA, USA).
2.2. Model and assumption
We used a binary Markov chain model. The model allowed each practice to be followed over time in discrete daily cycles. In each cycle, costs and revenue were estimated, as described below. The model allowed variation in the period of mitigation/suppression policies (thereby reflecting on the short-term impact of Covid-19 on practices) and to simulate longer-term utilization changes. Specifically, a longer-term reduction in out-of-pocket expenses was modelled in a sensitivity analysis, building on data on the alteration of consumption as a consequence of the Greek financial crisis of 2010 [7]. Notably, it is also conceivable that given the expected societal financial losses, contractions in statutory and private health insurance expenditure may occur in the future; this was not reflected on in our analysis.
The following logic was applied in the model: (1) Covid-19 mitigation/suppression policies, including curfews and physical distancing, were legally implemented stepwise in Germany, with nationwide implementation being concluded by 22nd March 2020. Note that policies differ to some degree between federal states, while our model does not reflect this in detail. We assumed these policies to be upheld for a range of periods (90 days: base case; 45, 135 days: sensitivity analyses). (2) These policies were assumed to short-term impact on practices’ revenue, with differential impact on different services type (see below). We assumed this impact to be lifted once the measures are not upheld any longer. (3) We analyzed the effect of longer-term reduced out-of-pocket spending for dentistry in a sensitivity analysis. This analysis was grounded on data from Greece, as described, showing that dental out-of-pocket spending may well contract up to 50 % in all services blocks except those related to pain and emergency treatments. It needs highlighting that the economic crisis in Greece lasted for an extended period; we hence consider this a “worst case scenario” analysis for Germany and the Covid-19 crisis [7]. Note that any further analyses on spending shifts from out-of-pocket to insurances spending were not feasible given the current paucity in data. (4) We did not consider possibly increased costs, e.g. those for intensified hygiene measures, or decreases in the usage of other materials or laboratory services, which may also affect costs. We did also not consider that staff would be temporarily laid off or working time reductions implemented, as these measures are all rather a consequence of the revenue stream reduction and should be considered as such when applying the results of this study.
Model validation was performed internally by varying key parameters to check their impact on the results and by performing sensitivity analyses.
2.3. Input variables
Costs were estimated using data from the national association of statutory German dentists (KZBV) as well as the federal association of German dentists (Bundeszahnärztekammer). We considered costs for staff, material, laboratory, and other costs (including those for office rent, redemption payments, interest etc.). Revenue was estimated according to different source (statutory insurance, private insurance and employed-based schemes and other revenue, out-of-pocket expense revenue). Revenue was then subsetted in the described seven different services groups in each source [2,8].
Bases on costs and revenue, the “mean” dental practice in Germany can be reflected in economic terms. To reflect the differential economic impact of Covid-19 on different practices, two scenarios were modelled, as described: Low/high volume, low/high proportion of non-statutory insurance revenue, low/high staff pool and costs. Based on data from KZBV [2,9], we varied the cost in both practices accordingly and checked the resulting overall mean values for Germany for consistency. Moreover, the reported distribution in revenue across practices [9] was additionally reflected, assuming revenue and costs (see below) to correlate (i.e. a practice at the higher end of the revenue spectrum was assumed to also have higher costs). Overall, we aimed to introduce the observed variability in cost-revenue structures in German dental practices.
To inform our model as to the reduction in the utilization of different services, a telephone-based survey was conducted between 24th March and 2nd April 2020. A random sample of 300 dentists was drawn from a comprehensive address lists of German dentists (note that not all dentists had provided their telephone contact). Three interviewers contacted the practices and used a pre-tested interview guide to inquire dentists or qualified dental administrative staff as to the absolute and relative reduction in the utilization of different services they experienced. Of the 300 contacted dentists, a total of 146 responded. The yielded relative reductions in utilization were transformed into probability density functions using kernel density estimations. The bandwidths of the Gaussian kernels were selected based on Scott’s rule [10]. The probability function was cut at the thresholds 0 and 1. The probability outside of these boundaries was uniformly added on a percentage scale to the probabilities within them, hence probabilities summed up to 1 (i.e., 100 %). No detailed non-responder analysis was performed, and as many practices were unwilling to provide socio-demographic data as to the provider, it remains unclear if our sample was representative. However, given the observed consistency in responses within this sample and with other surveys conducted on the Covid-19 impact on businesses in Germany [11], we assume the risk of selection bias to be limited.
2.4. Outcomes and discounting
The outcomes of our study were practice costs and revenue (in Euro 2020). Additionally, the cost-revenue ratio was estimated. A ratio of 1 indicates costs and revenue being equal, values below or above 1 indicate that costs are lower or higher than revenue, respectively. Given the horizon of our study, no discounting was applied.
2.5. Analytical methods
Monte-Carlo microsimulations were performed to estimate cost-effectiveness, with 100 practices being modelled in each scenario and followed over a year. Parameter uncertainty was introduced by random sampling of transition probabilities [12]. Samples were drawn 100 times. Univariate and joint-probability sensitivity analyses were performed to assess the relevance of a range of parameters on our outcome and to evaluate the robustness of our findings.
3. Results
3.1. Study parameters
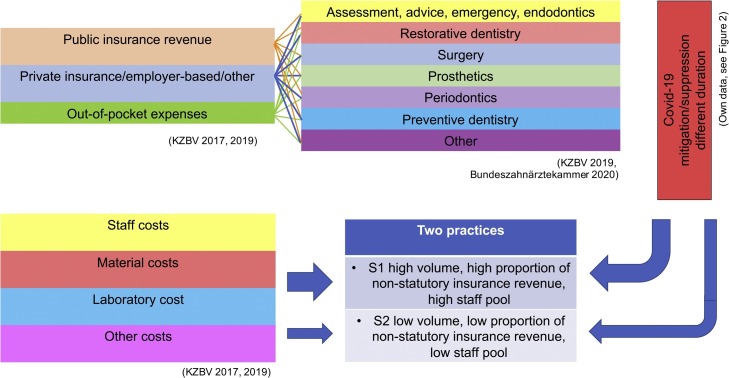
The data input and flow are summarized in Fig. 1 . A Markov model with two stages; “pandemic mitigation/suppression policies upheld” or” pandemic mitigation/suppression policies concluded”, was constructed. The duration of the policies being upheld was varied between 45, 90 and 135 days. For two different practice scenarios (S1, S2), revenue and costs over 365 days were estimated, with variability in costs and revenue being introduced by random sampling from distributions reported by the KZBV [9]. Revenue was generated from three different sources and in seven subsets, as described. Table 1 summarizes costs and revenues.
Fig. 1.
Modelling strategy and data input. We considered three revenue streams, each with seven different services subsets. The Covid-19 mitigation/suppression policies were modelled over different time periods and impacted on services utilization in different services subsets. Different costs were considered and assumed to not be reduced during these measures. Two different practices were modelled, allowing to assess the practice-specific economic impact of Covid-19 mitigation/suppression policies. Data sources can be found in the reference list.
Table 1.
Input parameter on costs and revenue in different practices, stratified by revenue stream and service subset (expected costs and revenue without any Covid-19 mitigation/suppression policies).
| Parameter | Practice S1 |
Practice S2 |
||
|---|---|---|---|---|
| Na | 39.244 |
7.701 |
||
| Euro | % | Euro | % | |
| Total costs/year | 360,747 | 100 | 245,016 | 100 |
| Staff costs/year | 151,587 | 42 | 86,991 | 35 |
| Material costs/year | 28,800 | 8 | 28,175 | 12 |
| Laboratory costs/year | 90,000 | 25 | 56,350 | 23 |
| Others (office, redemption, interest) costs/year | 90,360 | 25 | 73,500 | 30 |
| Statutory revenue | ||||
| Assessment, advice, endodontics, emergencies etc. | 125,123 | 43.2 | 99,401 | 43.2 |
| Restorations | 48,124 | 16.6 | 38,231 | 16.6 |
| Surgery | 8,354 | 2.9 | 6,636 | 2.9 |
| Prosthetics | 72,697 | 25.1 | 57,752 | 25.1 |
| Periodontology | 10,847 | 3.7 | 8,617 | 3.7 |
| Preventive dentistry | 12,431 | 4.3 | 9,875 | 4.3 |
| Others | 11,802 | 4.1 | 9,375 | 4.1 |
| Total | 289,378 | 100.0 | 229,887 | 100.0 |
| Private insurance, employer schemes, others revenue | ||||
| Assessment, advice, endodontics, emergencies etc. | 36,877 | 27.0 | 20,324 | 27.0 |
| Restorations | 14,184 | 10.4 | 7817 | 10.4 |
| Surgery | 2,462 | 1.8 | 1,357 | 1.8 |
| Prosthetics | 22,689 | 16.6 | 12,505 | 16.6 |
| Periodontology | 12,468 | 9.1 | 6,872 | 9.1 |
| Preventive dentistry | 21,644 | 15.8 | 11,929 | 15.8 |
| Others | 26,010 | 19.0 | 14,335 | 19.0 |
| Total | 136,334 | 100.00 | 75,139 | 100.00 |
| Out-of-pocket revenue | ||||
| Assessment, advice, endodontics, emergencies etcb | 0 | 0 | 0 | 0 |
| Restorations | 53,871 | 38.1 | 31,985 | 38.1 |
| Surgery | 2,598 | 1.8 | 1,542 | 1.8 |
| Prosthetics | 23,271 | 16.5 | 13,857 | 16.5 |
| Periodontology | 12,788 | 9.0 | 7,615 | 9.0 |
| Preventive dentistry | 22,199 | 15.7 | 13,219 | 15.7 |
| Others | 26,677 | 18.9 | 15,886 | 18.9 |
| Total | 141,404 | 100.0 | 84,104 | 100.0 |
Licensed dentists excluding orthodontists. Orthodontic revenues were also excluded. Note that due to random sampling from distributions, modelled revenue (Table 2) will deviate minimally.
Assumed this subset to be zero and shifted to out-of-pocket expenses for restorations, as patients in Germany usually only pay treatments not fully or partially covered out of their own pockets. Note that this shift may affect consistency between subsets to a minor degree.
3.2. Cost and revenue
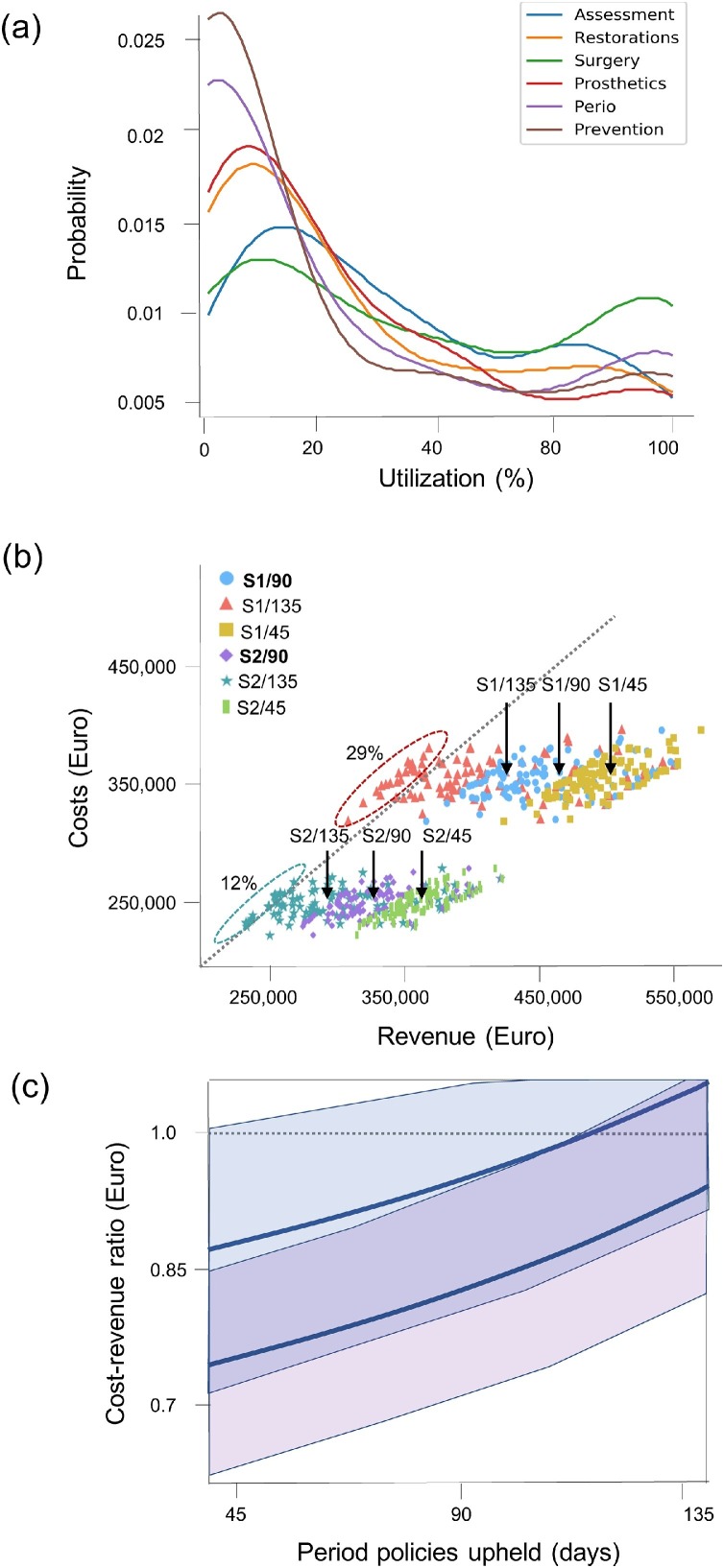
Based on our survey, probability distributions for utilization of different services subsets were estimated (Fig. 2 a). Utilization was reduced across services; the mean utilization was 41 % for assessment, advice, emergency and endodontic and other treatment, 32 % for restorations, 48 % for surgery, 30 % for prosthetics, 24 % for periodontal services and 20 % for prevention. Over the course of 365 days and within the base case scenario, this had profound impact on the revenue stream. While costs were assumed to remain stable in practice S1 (at 356,090 Euro in mean) and S2 (at 248.339 Euro), revenue decreased to a total of 458,592 Euro and 333,232 Euro, respectively. Compared with the expected revenue (without any mitigation/suppression policies) and in S1, reductions of 42,694 Euro (-18.7 %) in public, 21,162 Euro (-18.6 %) in private and 22,290 Euro (-19 %) in out-of-pocket expenses revenue were noted, respectively (Table 2 ). In S2, reductions were 35,720 Euro (-15.7 %) in public, 11,920 Euro (-18.7 %) in private and 13,556 Euro (-19 %) in out-of-pocket expenses revenue, respectively.
Fig. 2.
Utilization reduction (a), cost-revenue plane (b), and cost-revenue ratios of practices in sensitivity analysis (c). (a) The probabilities of the relative dental services utilization (in percentage) of different services associated with Covid-19 and implemented mitigation/suppression policies in Germany (based on n = 146 interviewed dentists). For each % of utilization (x-axis), the probability is given (i.e. the surface under the curve is 1, or 100 %). It is obvious that while for the majority of services, utilization was decreased to 0-20 %, there were service-specific decreases (e.g. surgical services and assessment, advice, endodontic and emergency therapies were less affected than preventive or periodontal services). (b) The costs (x-axis) and revenue (y-axis, both in Euro) of the two different modelled practices (S1, S2) were plotted. Different periods of Covid-19 associated mitigation/suppression measures were assessed (base case: 90 days, sensitivity analyses: 45, 135 days). The mean cost-revenue per analysis are indicated by arrows. Practices above the bisectional show higher costs than revenues over 365 days (i.e, a negative net profit); this was only the case in the scenarios where measures were upheld for 135 days. Such practices are indicated by ellipses (%: share of practices in this scenario with negative net profit). (c) Sensitivity analysis, showing the mean (line) and 2.5-97.5 percentiles (shaded areas) cost-revenue ratio depending on the time period Covid-19 measures are upheld. Two scenario practices (S1 blue, S2 purple) were modelled. In this sensitivity analysis, a contraction of out-of-pocket spending by 50 % after the policies are concluded was assumed. A cost-revenue ratio of >1 indicates a net negative profit of a practice over the 365 days period. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
Table 2.
Costs and revenues over the modelled 365 days in different practices. The period of Covid-19 mitigation/suppression policies was varied. Different revenue streams are displayed.
| Duration | S1 | S2 | |
|---|---|---|---|
| Days | Euro (Mean) (2.5 %–97.5 %) | ||
| Costs totala | n/a | 356,090 (324,360–386,640) | 248,339 (227,850−270,235) |
| Revenue total | 90 | 458,592 (396,318−546,736) | 333,232 (277,806−403,473) |
| 45 | 500,971 (452,026−558,389) | 363,830 (321,665−409,861) | |
| 135 | 416,212 (331,903−544,073) | 302,634 (233,708−400,336) | |
| Public revenue | 90 | 227,351 (196,031−270,823) | 123,874 (57,159−232,665) |
| 45 | 248,698 (224,002−276,094) | 141,734 (83,271−233,828) | |
| 135 | 206,698 (164,219−268,991) | 106,013 (29,390−231,283) | |
| Private, employer-based, other revenue | 90 | 113,693 (98,325−135,703) | 64,237 (53,615−77,899) |
| 45 | 124,274 (112,087−138,586) | 70,197 (62,095−79,899) | |
| 135 | 103,112 (82,319−135,046) | 58,277 (45,058−77,292) | |
| Out-of-pocket expenses revenue | 90 | 117,547 (101,790−140,717) | 71,695 (59,964−87,201) |
| 45 | 128,692 (115,936−143,708) | 78,473 (69,483−88,588) | |
| 135 | 106,401 (85,364−140,035) | 64,918 (50,334−86,522) |
Costs deviate from those in Table 1 to some minor degree given the random sampling from distributions.
3.3. Sensitivity analyses
If measures and associated impact on utilization were upheld for different time periods (Fig. 2b), the revenue impact de- or increased. For a period of 45 days, the mean revenue decrease was only 42,379 Euros (-8.4 %) in S1 and 30,528 (-8.6 %) in S2, respectively. If the period was 135 days, this decrease was 127,137 (-31 %) in S1 and 91,584 (-30 %) in S2, respectively. In this case, 29 % S1 and 12 % S2 practices would have a negative net profit over the 365 days period. If assuming out-of-pocket spending to contract by 50 % after Covid-19 policies being concluded (without any shifts to insured spending), the mean cost-revenue ratio increased to 88 % for S1 and 74 % for S2 practices if policies were upheld for 90 days, and was at 95 % (in mean) in S1 and 81 % in S2 if the same measures were upheld for>130 days (Fig. 2c).
4. Discussion
The Covid-19 pandemic and the subsequently implemented policies worldwide are unprecedented in modern times. Mitigation and suppression, necessary to contain the spread, are likely to impact on the economy, with catastrophic results for many small- and middle-sized businesses. In most countries affected by Covid-19, Germany being one of them, dental practices are predominantly small to medium-sized business operated privately. Our study shows that the longer these measures are extended, the more likely they seem to affect the economic capacity of dental practices, which may translate into job losses and qualitative and quantitative changes in care provision. Currently, decision making is hampered by a lack of data such as the case fatality rate of Covid-19 as well as the contribution to its spread by dentists. We aimed to inform decision makers about the economic impact of policies of mitigation/suppression on dental practices. This may assist them in preparing appropriate countermeasures during and after the pandemic.
We show that mitigation/suppression policies put dental practices under a financial stress directly proportional to the time they are in place. In our base case analysis, after 90 days of reduced clinical activity, the majority of the dental practices generate very reduced profits before taxes; if upheld for longer, a relevant proportion of practices will yield negative profits in 2020, the consequences of which we did not assess further. Reflecting on the possibly reduced out-of-pocket spending resulted in even worse cost-revenue ratios, with a relevant share of practices not being profitable any longer (even the mean S1 practice was barely profitable in such scenario if measures were upheld for 135 days).
This study has a number of limitations. First, we did not model the gradual transition between the stages (policies upheld/lifted). It is likely that full operability of practices after lifting the policies will take time, and that utilization will not be immediately normalised. Also, lifting of policies is likely to be done on a progressive manner since the risk of contagion will not disappear after 45, 90 or 135 days. Overall, we expect an adjustment of processes and protocols for a long period after the pandemic has been contained [13]. We did not estimate the economic impact measures of progressive normalisation, such as operating within limited indications, forcing the use of FFP2 masks or requiring extensive testing and further isolation measures for dental workers contracting Covid-19. Similarly, the data used to construct our cost-revenue framework stemmed from the time before Covid-19 pandemic. The assumption that practices continue to operate under normal costs, for example, during mitigation/suppression measures, without adapting protocols, is unlikely. As mentioned, it is likely that certain costs (e.g. for hygiene) will increase, and others decrease (other materials, laboratory costs given the decrease in prosthetic services utilization, for example). The larger blocks, staff and other costs, however, will be rather constant unless wider economic policies like short term work reduction (as offered on a broad scale by the federal government of Germany) are adopted in dental practices, too. Third, this model is a simplification and built on a range of assumptions, most of them involving the future. It serves to demonstrate the possible effects of Covid-19 associated policies and will, with some chance, be proven wrong (at least to some degree and especially if our findings are used to mitigate the demonstrated consequences). We encourage to revisit our findings when the crisis is over and to validate or refute the applied methods, thereby contributing to this rather new field of research and its development. Lastly, our study focused on the German healthcare setting. This was done, as costs and revenue data are granularly available, and as given the specific two-tiered outline, aspects of different other healthcare systems are reflected (statutory insurance schemes, out-of-pocket expenses etc). Comparative studies in other healthcare systems that do not have statutory dental health insurance remain warranted, though. Moreover, each individual practice in Germany will have its own cost-revenue setup, and our findings merely reflect the mean practice in each scenario.
A range of aspects demand appropriate consideration. First, we find that after 90 days of mitigation/suppression, the majority of the dental clinics in Germany will show only minimal profitability over the next year. However, and to be highlighted, these estimates do not include any compensation for practice owners, who normally retain the net benefits of their practice as income before tax. It should be noted that a significant number of practices with minimal net profit would run into a negative overall financial result over the modelled year if the average dentist’s salary was deduced from the practice’s revenue.
We also show that the cost-structure and the level of alteration of revenue will vary significantly and generate significant differences in the impact of the measures between practices. Specifically, practices operating at higher costs more often showed low or even negative balances compared with those with lower costs. This is consistent with our expectations since smaller enterprises accrue costs at a slower rate than bigger enterprises when their operability is restricted. Also, larger and high-volume practices suffer from the service-specific reduction in utilization. In our sensitivity analysis, and assuming out-of-pocket expenses to contract beyond the Covid-19 measures being upheld, a large share of these practices will run into severe profitability problems even in the 90 days scenario, and nearly every second practice will not be profitable any longer if measures were upheld for >135 days.
Our data can also offer some insights when analysing the changes and challenges during the adaptation period to the implemented measures. A significant percentage of a dental practices’ income is obtained through highly complex services such as oral rehabilitation including prosthetics. These take several months to be completed and were among the most Covid-19 affected services according to the dentists’ self-reports. It remains unclear if this is due to dentists rejecting treating patients to comply with recommendations, for example towards the reduction of aerosol generation, or if patients are refusing these treatments because they consider themselves at risk by receiving dental care. In general, we demonstrate that service patterns changed dramatically, while in opposite to data reported for dental clinics in China, a general shut-down for all services except emergencies has not occurred yet [14]. We assume that practices so far decided to remain open, which mitigates the financial damage to some degree, while overall the revenue dent generated by suppression/mitigation policies remains relevant, as our data show. If, however, Covid-19 measures remain upheld for longer, or the pandemic spreads further, closing down practices temporarily will likely be an alternative for financial and infection control reasons. In this case, we assume a centralization of dental services in specialized practices (such practices have already been commissioned in Germany for treating confirmed Covid-19 cases requiring dental care). Such centralization could potentially contribute to aggravate the economic impact if no measures for financial support for those forced to close down are in place.
As described, a contraction in out-of-pocket expenses of patients is likely even after the Covid-19 associated measures are concluded, mainly as individuals will be faced with financial constraints resulting from the short-term acute crisis but also its mid-term economic sequels. Notably, further developments are conceivable: Patients may not only utilize out-of-pocket services less often but shift their utilization to services fully covered by the statutory insurance. Data on the utilization of prosthetic services by patients receiving full instead of only partial insurance coverage in Germany validate this argument [15]. Hence, we may see higher costs in the statutory insurance as a result, while obviously insurance contributions will shrink as GDP contracts and unemployment rises. Policy makers may want to prepare the statutory insurance accordingly.
5. Conclusions
Our model shows that the longer Covid-19 mitigation/suppression measures are upheld, the greater the financial distress imposed onto dental clinics will be, affecting especially those with higher operational costs. In our model, after 135 days of upheld measures, 29 % of S1 type practices and 12 % of S2 type practices will no longer cover their operative costs before taxes. The reduction on revenue during this period will be 127,137 Euros in S1 and 91,584 Euros in S2, respectively. Additional longer-term contractions in out-of-pocket expenses may aggravate the economic impact on practices. Healthcare decision makers should consider to financially support dental practices while organizing dental care along infection control policies. Practice owners may consider practice re-organization to reduce costs and maintain minimum profitability.
Author contribitions
Falk Schwendicke contributed to conception and design, acquisition, analysis, and interpretation, drafted the manuscript and critically revised it, gave final approval and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Joachim Krois contributed to analysis and interpretation, critically revised the manuscript, gave final approval and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Jesus Gomez Rossi contributed to conception and design, acquisition, analysis, and interpretation, drafted the manuscript and critically revised it, gave final approval and agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of competing interest
The authors do not have any conflict of interest. The authors are solely responsible for the contents of this paper.
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors, but was funded by the authors and their institutions. The authors deny any conflict of interest.
References
- 1.Bundeszahnärztekammer . 2019. Nicht Systemrelevant? Zahnmedizin, Goodwill und BIP. [Google Scholar]
- 2.KZBV . 2019. KZBV Jahrbuch 2019. [Google Scholar]
- 3.Johns Hopkins University; 2020. Corona Virus Response Center. [Google Scholar]
- 4.Teralytics . 2020. Deutschland Bleibt Zu Hause. [Google Scholar]
- 5.Husereau D., Drummond M., Petrou S., Carswell C., Moher D., Greenberg D., Augustovski F., Briggs A.H., Mauskopf J., Loder E. Consolidated health economic evaluation reporting standards (CHEERS)--explanation and elaboration: a report of the ISPOR health economic evaluation publication guidelines good reporting practices task force. Value Health. 2013;16(2):231–250. doi: 10.1016/j.jval.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Gesundheitsberichtserstattung . 2018. Versicherungsverhältnisses in Der Krankenversicherung. [Google Scholar]
- 7.Kostas D., Dimitris N. The effects of economic crisis on the demand and supply of the dental services in Greece. J. Int. Soc. Prev. Community Dent. 2017;7(2):135–140. doi: 10.4103/jispcd.JISPCD_496_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bundeszahnärztekammer . 2020. BZÄK Statistisches Jahrbuch 18/19. [Google Scholar]
- 9.KZBV . 2017. KZBV Jahrbuch 2017. [Google Scholar]
- 10.Scott D.W. On optimal and data-based histograms. Biometrika. 1979;66(3):605–610. [Google Scholar]
- 11.DIHK . 2020. Auswirkungen Des Corona-virus Auf Die Deutsche Wirtschaft: DIHK-Blitzumfrage März 2022. [Google Scholar]
- 12.Briggs A.H., O’Brien B.J., Blackhouse G. Thinking outside the box: recent advances in the analysis and presentation of uncertainty in cost-effectiveness studies. Annu. Rev. Public Health. 2002;23(1):377–401. doi: 10.1146/annurev.publhealth.23.100901.140534. [DOI] [PubMed] [Google Scholar]
- 13.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J. Dent. Res. 2020 doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang Y., Zhou Y., Liu X., Tan J. Health services provision of 48 public tertiary dental hospitals during the COVID-19 epidemic in China. Clin. Oral Investig. 2020 doi: 10.1007/s00784-020-03267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hempel F., Krois J., Beuer F., Kuhlmey A., Paris S., Schwendicke F. Prosthetic treatment patterns in the very old: an insurance database analysis from Germany. Clin Oral Investig accepted. 2020 doi: 10.1007/s00784-020-03264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]