Abstract
Objectives
N95 mask is essential for healthcare workers dealing with the coronavirus disease 2019 (COVID-19). However, N95 mask causes discomfort breathing with marked reduction in air exchange. This study was designed to investigate whether the use of N95 mask affects rescuer's fatigue and chest compression quality during cardiopulmonary resuscitation (CPR).
Methods
After a brief review of CPR, each participant performed a 2-minute continuous chest compression on a manikin wearing N95 (N95 group, n = 40) or surgical mask (SM group, n = 40). Compression rate and depth, the proportions of correct compression rate, depth, complete chest recoil and hand position were documented. Participants' fatigue was assessed using Borg score.
Results
Significantly lower mean chest compression rate and depth were both achieved in the N95 group than in the SM group (p < 0.05, respectively). In addition, the proportion of correct compression rate (61 ± 19 vs. 75 ± 195, p = 0.0067), depth (67 ± 16 vs. 90 ± 14, p < 0.0001) and complete recoil (91 ± 16 vs. 98 ± 5%, p = 0.0248) were significantly decreased in the N95 group as compared to the SM group. At the end of compression, the Borg score in the N95 group was significantly higher than that in the SM group (p = 0.027).
Conclusion
Wearing a N95 mask increases rescuer's fatigue and decreases chest compression quality during CPR. Therefore, the exchange of rescuers during CPR should be more frequent than that recommended in current guidelines when N95 masks are applied.
Keywords: N95 mask, COVID-19, Chest compression, Fatigue
1. Introduction
High-quality cardiopulmonary resuscitation (CPR) is a major part in the historical “survival chain” [1]. Effective chest compression (CC) is one of the most important aspect of CPR. The 2015 guidelines of the American Heart Association (AHA) emphasized the concept of high-quality CPR, with more stringent requirements on the depth and frequency [2]. Chest compression quality can be affected by rescuer's characteristics (e.g., gender, weight, muscular fitness) [3,4] and decreased along with the time of performance due to fatigue [5]. Therefore, the current guidelines recommended that rescuers should take turns every 2 min [6,7]. On the other side, it has been suggested that the hand-off time adversely affects cardiac arrest survival and neurological outcome [8,9]. The new guidelines highlighted reducing interruption in order to maintain the quality of chest compression [2].
The emergence of novel coronavirus disease (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) had affected millions of people. Since the transmission of the COVID-19 is mainly through respiratory droplets [10], wearing surgical masks or N95 masks can effectively reduce the chance of human-to-human transmission [11]. However, a previous study suggested that the N95 mask causes discomfort breathing with an average reduction of 37% in air exchange volume [12]. Very recently, an interim guidance for basic and advanced life support in COVID-19 cases has been published, which also recommended all rescuers should don personal protective equipment including a N95 mask during CPR [13]. In the present study, we aim to evaluate whether wearing a N95 mask alters the chest compression quality and rescuer's fatigue during simulated CPR.
2. Materials and methods
2.1. Ethics
This study was performed in Zhongnan Hospital of Wuhan University in Wuhan between April 28 to 29, 2020. The study protocol was approved by the Ethics Committee of Zhongnan Hospital, and each participant signed an informed consent at the time of recruitment.
2.2. Participants recruitment
Posters were used to recruit volunteers in Zhongnan Hospital of Wuhan University (Wuhan, China). Participants aged <65 years old were eligible for inclusion. Participants with physical disabilities or other health problems which might affect the quality of chest compression were excluded. Pre-designed questionnaire was sent to each participant for following information: age, sex, height, weight, years of career experience and professional position.
2.3. Review of chest compression-only CPR
American Heart Association (AHA) basic life support (BLS) certificated instructor performed a 45-minute review about CPR based on 2015 guidelines, especially one single-rescuer CPR sequence and skills to high-quality chest compression. Then, each participant practiced one single-rescuer chest-compression only CPR under the supervision of instructors for a total period of 30 min and passed skill test for BLS certification.
2.4. Randomization
After CPR review and BLS skill test, participants were randomly assigned into two groups in a 1:1 ratio. Randomization was performed by assigning the random numbers. Participants in the SM group wear a surgical mask (Evereast Medical Products Group CO., LTD, Xinxiang, China) during chest compression, whereas those in the N95 group wear a N95 mask (8210PluxMX, 3 M Company, MN, USA).
2.5. Outcome measurements
Standardized CPR outcome measures from the 2015 International Liaison Committee on Resuscitation were used in this study [15]. Resusci Anne QCPR manikins (Laerdal China Ltd., Hangzhou, China) were used to assess chest compression quality. Each manikin was equipped with a real-time feedback system (SimPad system) to provide parameters including compression depth, rate, chest recoil and correct hand position. Based on the international guidelines, correct chest compression requires a depth between 5 and 6 cm, a rate between 100 and 120 compressions per minute, and a complete chest recoil [2,15]. Participants' CPR scores (range: 0–100) were generated by the SimPad reports. Rescuer's fatigue was determined using Borg scale as we previously described [16]. Heart rate, respiration rate, blood pressures and oxygen saturation were recorded before and immediately after chest compression. Study diagram was presented in Fig. 1 .
Fig. 1.
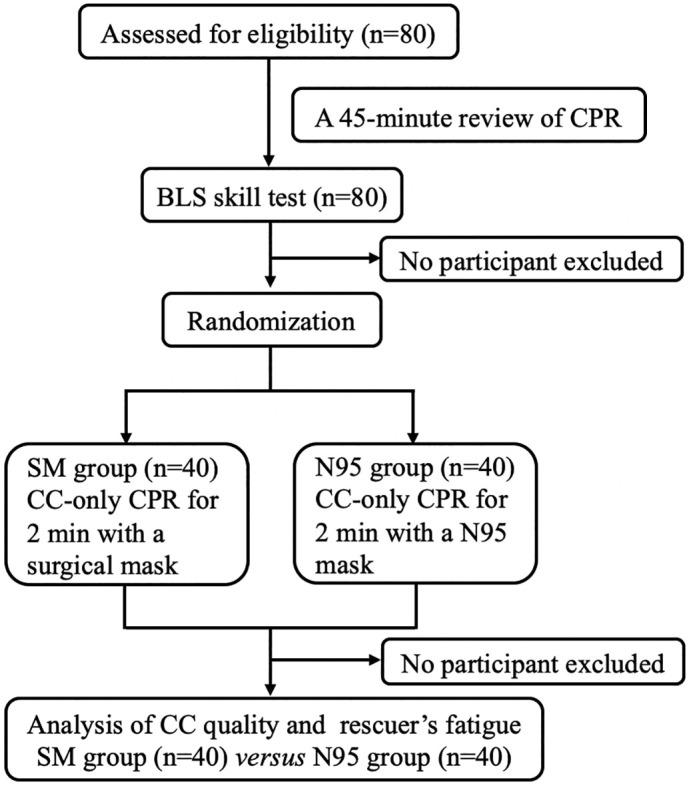
Flow diagram of the study. BLS: basic life support; SM: surgical mask; CC: chest compression; CPR: cardiopulmonary resuscitation.
2.6. Sample size calculation
To detect an important difference of 50% in the correct compression depth proportion at 2 min between the SM and the N95 groups with a power of 0.9, and a type I error of 0.05, the sample size calculation yielded 70 participants. Finally, we planned to include 80 participants, anticipating some loss for various reasons. The data regarding the proportion of correct compression depth at 2 min in a manikin study (75 ± 35%) [14] were used to estimate the sample size.
2.7. Statistical methods
Non-parametric continuous variables were analyzed using the Mann–Whitney U test while parametric continuous variables were analyzed using the student t-test. Categorical variables were compared using the chi-squared test. A two-tailed P value <0.05 was considered statistically significant. Statistical analyses were processed by the IBM SPSS version 20.0 (IBM Corporation, New York, USA).
3. Results
3.1. Study population demographics
In total, 80 healthcare workers including 23 doctors and 57 nurses participated in this study. Mean age of participants in the N95 and the SM group were 32 and 31 years old, respectively. There were 18 (45.0%) male in the N95 group and 19 (47.5%) male in the SM group. There were no significant differences in age and gender distribution between groups. Body weight, height and body mass index were also similar between the SM and the N95 group. In addition, there were no significant differences in career experience and professional position between groups. Data were summarized in Table 1 .
Table 1.
General characteristics of participants.
| N95 group (n = 40) |
SM group (n = 40) |
p Value | |
|---|---|---|---|
| Age, mean ± SD, years | 32 ± 6 | 31 ± 7 | 0.459 |
| Gender, n (%) | |||
| Male | 18 (45.0) | 19 (47.5) | 0.823 |
| Female | 22 (55.0) | 21 (52.5) | |
| Height, median (IQR), cm | 168 (160–172) | 167 (160–172) | 0.933 |
| Weight, mean ± SD, kg | 61 ± 11 | 61 ± 10 | 0.965 |
| BMI, median (IQR), kg/m2 | 21.4 (20.2–24.1) | 21.9 (19.7–23.5) | 0.828 |
| Professional position, n (%) | |||
| Doctors | 11 (27.5) | 12 (30.0) | 0.805 |
| Nurses | 29 (72.5) | 28 (70.0) | |
| Career experience, mean ± SD, years | 8.9 ± 6.7 | 8.0 ± 6.7 | 0.570 |
Data were expressed as number, percentage, mean ± SD or median (IQR). SM: surgical mask; BMI: body mass index.
3.2. Chest compression quality
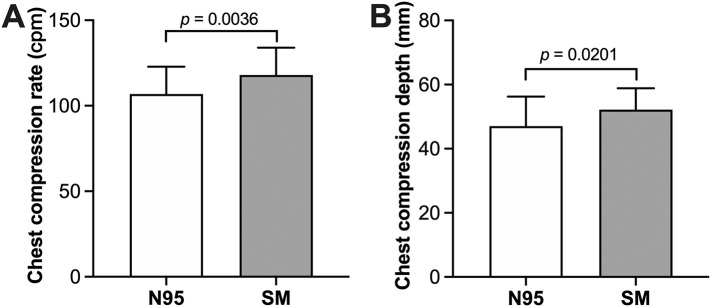
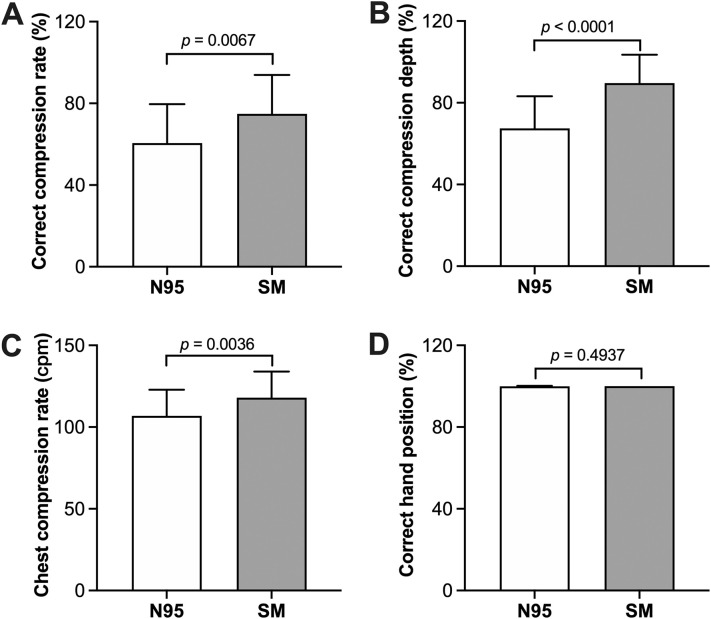
The mean chest compression rate (107 ± 16 vs. 118 ± 16, p = 0.004) and depth (47 ± 9 vs. 52 ± 7, p = 0.020) were significantly decreased in the N95 group as compared to the SM group (Fig. 2 ). In order to evaluate the quality of chest compression in two groups, we calculated the proportion of correct chest compression rate, depth, chest recoil and hand position. As seen in Fig. 3 , the proportion of correct chest compression rate (61 ± 19% vs. 75 ± 19%, p = 0.0067), depth (67 ± 16% vs. 90 ± 14%, p < 0.0001) and recoil (91 ± 16% vs. 98 ± 5%, p = 0.0248) were significantly lower in the N95 group than that in the SM group. However, no difference in the proportion of correct hand position has been observed between the N95 and the SM groups (100 ± 0 vs 100 ± 0, p = 0.4937).
Fig. 2.
Chest compression rate and depth. The average chest compression rate and depth in the N95 group were significantly decreased as compared to the SM group. SM: surgical mask; cpm: compression per minute.
Fig. 3.
Proportions of correct chest compression. After a 2-min chest compression, the proportion of correct chest compression rate (A), depth (B) and chest recoil (C) were significantly higher in the SM group than that in the N95 group. However, no difference in correct hand position was observed between two groups (D). SM: surgical mask.
3.3. Fatigue
The Borg score has been used to assess rescuer's fatigue before and immediately after each performance. Our results showed that the median Borg score were similar between the two groups before chest compression (9 vs. 10, p = 0.435). However, the median Borg score after 2-min of chest compressions was significantly higher in the N95 group than that in the SM group (16 vs. 14, p = 0.027) (Table 2 ). At the end of chest compression, participants in the N95 group had insignificantly higher heart rate and respiration rate than that in the SM group (p > 0.05, respectively). No significant difference was observed in oxygen saturation and mean arterial blood pressures between two groups (p > 0.05, respectively).
Table 2.
Assessment of rescuers' fatigue before and after chest compression.
| Pre-compression |
p Value | Post-compression |
p Value | |||
|---|---|---|---|---|---|---|
| N95 group (n = 40) | SM group (n = 40) | N95 group (n = 40) | SM group (n = 40) | |||
| Heart rate, beats/min | 87 ± 10 | 84 ± 10 | 0.145 | 122 ± 20 | 118 ± 19 | 0.480 |
| Respiration rate, breaths/min | 17 ± 3 | 16 ± 3 | 0.218 | 21 ± 5 | 19 ± 5 | 0.061 |
| Mean arterial pressure, mmHg | 92 ± 8 | 95 ± 10 | 0.208 | 98 ± 10 | 98 ± 12 | 0.962 |
| Oxygen saturation, % | 99 (98–100) | 99 (98–100) | 0.704 | 98 (97–100) | 99 (98–99) | 0.224 |
| Borg score | 9 (6–12) | 10 (7–13) | 0.435 | 16 (14–18) | 14 (13–16) | 0.027 |
Data were expressed as mean ± SD or median (IQR). SM: surgical mask.
4. Discussion
The major findings of this study can be summarized as follows: (1) the mean chest compression rate and depth in the N95 group were significantly decreased as compared to the SM group; (2) a significantly lower proportion of correct chest compression rate, depth and complete chest recoil were both achieved in the N95 group than in the SM group after a 2-min continuous chest compression; (3) the Borg score was significantly higher in the N95 group than that in the SM group, indicating an increased fatigue of these participant performing chest compression with N95 masks.
According to a recently published interim guidance of basic and advanced Life support in adults, children, and neonates with suspected or confirmed COVID-19 [13], all rescuers should don personal protective equipment (PPE) to guard against contact with both airborne and droplet particles before entering the scene. In addition, limit personnel are recommended to reduce provider exposure. The International Liaison Committee also suggested that healthcare professionals should use PPE for aerosol generating procedures during resuscitation [15]. Therefore, during this epidemic, providing high-quality chest compression for COVID-19 patients undergoing cardiac arrest is quite a challenge for healthcare workers. A previous study based on the 2010 AHA guidelines suggested that the use of PPE decreases adequate chest compressions and increases rescuer's fatigue [16]. In that study, participants in the PPE group don a complete set of equipment including safety gloves, protective clothing, a respirator mask with active filter, and safety gumboots. However, in our present study, participants in the interventional group wear only a N95 mask. Our results found that the mean chest compression rate and depth were both deceased in the N95 group as compared to the SM group. In addition, the proportion of correct chest compression in the N95 group was significantly decreased as compared to the SM group. Importantly, our results were similar with that published by Chen and colleagues [16]. These results suggested that the use of N95 mask could be the major factor affecting chest compression quality and rescuer's fatigue.
In our study, the proportion of correct chest compression depth in the N95 and the SM group were 67 ± 16% and 90 ± 14%, respectively. A very recent study suggested that the proportion of sufficient chest compression depth was 75 ± 35% [14], which is lower than that we observed in the SM group. In fact, there were only 20 participants in that study, whereas we recruited 80 participants. In our study, a 45-min review of CPR and chest compression practice on manikin were performed prior to the experiment. Therefore, these differences in study design may result in different chest compression quality. The proportion of correct compression rate in the N95 group was 61 ± 19%, which was lower than that in the SM group (75 ± 19%). In addition, the complete chest recoil was also decreased in the N95 group as compared to the SM group. However, we found no differences in the proportion of correct hand position between two groups. In fact, both the N95 and the SM group have nearly 100% correct hand position. Together, our results suggested that the quality of chest compression was decreased when participants don a N95 mask.
Rescuer's fatigue commonly occurs at 1 min and markedly worsens at 2 min after the initiation of chest compression [17]. It has been widely accepted that rescuer's fatigue is an important factor in determining the quality of chest compressions [18]. In the present study, all participants performed a 2-min continuous chest compression. Our results found that participants performed chest compression with N95 mask had an increased Borg score as compared to those wearing a surgical mask. Although there were no significant differences in vital signs including heart rate, respiration rate, mean arterial pressure and oxygen saturation. This can be explained by two following reasons: (1) the effectiveness of these parameters in the evaluation of rescuer's fatigue have not been verified; (2) the small sample size has insufficient power to determine the differences. However, a significantly lower Borg score and decreased chest compression quality suggested that wearing a N95 mask increases rescuer's fatigue during chest compression. In a recently published guideline [18], compressors should be changed every 2 min, or sooner if fatigue. Our study tested the hypothesis that during a 2-min continuous chest compression, rescuer wearing a N95 mask shows increased fatigue and decreased chest compression quality.
Our study had three major limitations in this study. Firstly, our participants performed chest compressions in a simulated scenario, which differs from real clinical practice. However, the PPE is essential to stop the transmission of infectious diseases, healthcare workers should perform chest compressions under the protection of N95 masks, gloves, gowns and face shields in clinical practice. Therefore, the situation would be worse than that we simulated in the present study. Secondly, we only assessed the chest compression quality during the whole 2-min chest compression instead of at several different time points. Therefore, we are unable to see the changes in chest compression quality along with the time. Thirdly, we performed chest compression-only CPR instead of conventional CPR. Therefore, we were unable to determine the changes in ventilation.
5. Conclusions
Wearing a N95 mask increases rescuers' fatigue and decreases chest compression quality during simulated CPR. Therefore, the exchange of rescuers during CPR should be more frequent than that recommended in current guidelines when N95 masks are applied.
Funding
This study was supported by the National Natural Science Foundation of China (81900097), the Emergency Response Project of Hubei Science and Technology Department (2020FCA002, 2020FCA023) and the Emergency Diagnostic and Therapeutic Center of Central China.
CRediT authorship contribution statement
Yu Tian: Conceptualization, Methodology, Visualization, Investigation, Formal analysis, Writing - original draft. Xiaopeng Tu: Software, Investigation. Xianlong Zhou: Software, Investigation. Jiangtao Yu: Software, Investigation. Shan Luo: Visualization, Investigation, Formal analysis. Liping Ma: Visualization, Investigation, Formal analysis. Chang Liu: Visualization, Investigation, Formal analysis. Yan Zhao: Conceptualization, Methodology, Writing - original draft. Xiaoqing Jin: Conceptualization, Methodology, Supervision, Writing - review & editing.
Declaration of competing interest
None.
Acknowledgments
The authors would like to thank all the participants who made this study possible.
References
- 1.Koster R.W., Baubin M.A., Bossaert L.L., et al. European resuscitation council guidelines for resuscitation 2010 section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2010;81:1277–1292. doi: 10.1016/j.resuscitation.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perkins G.D., Travers A.H., Berg R.A., et al. Basic life support chapter collaborators. Part 3: adult basic life support and automated external defibrillation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2015;95:e43–e69. doi: 10.1016/j.resuscitation.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 3.Rad M., Rad M. A study of the factors related to cardiopulmonary resuscitation physical fatigue and the quality of resuscitation. Acta Facultatis Medicae Naissensis. 2017;34:43–53. [Google Scholar]
- 4.López-González A., Sánchez-López M., Garcia-Hermoso A., et al. Muscular fitness as a mediator of quality cardiopulmonary resuscitation. Am J Emerg Med. 2016;34:1845–1849. doi: 10.1016/j.ajem.2016.06.058. [DOI] [PubMed] [Google Scholar]
- 5.Liu S., Vaillancourt C., Kasaboski A., et al. Bystander fatigue and CPR quality by older bystanders: a randomized crossover trial comparing continuous chest compressions and 30:2 compressions to ventilations. CJEM. 2016;18:461–468. doi: 10.1017/cem.2016.373. [DOI] [PubMed] [Google Scholar]
- 6.Link M.S., Berkow L.C., Kudenchuk P.J., et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S444–S464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 7.Kleinman M.E., Goldberger Z.D., Rea T., et al. 2017 American Heart Association focused update on adult basic life support and cardiopulmonary resuscitation quality: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2018;137:e7–e13. doi: 10.1161/CIR.0000000000000539. [DOI] [PubMed] [Google Scholar]
- 8.Lee K., Kim M.J., Park J., et al. The effect of distraction by dual work on a CPR practitioner’s efficiency in chest compression: a randomized controlled simulation study. Medicine (Baltimore) 2017;96:e8268. doi: 10.1097/MD.0000000000008268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nichol G., Leroux B., Wang H., et al. Trial of continuous or interrupted chest compressions during CPR. N Engl J Med. 2015;373:2203–2214. doi: 10.1056/NEJMoa1509139. [DOI] [PubMed] [Google Scholar]
- 10.Lai C.C., Shih T.P., Ko W.C., et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chinese Disease Control and Prevention Center Guidance of mask use for different population for the prevention of COVID-19. http://www.nhc.gov.cn/jkj/s7916/202002/485e5bd019924087a5614c4f1db135a2.shtml
- 12.Lee H.P., Wang D.Y. Objective assessment of increase in breathing resistance of N95 respirators on human subjects. Ann Occup Hyg. 2011;55:917–921. doi: 10.1093/annhyg/mer065. [DOI] [PubMed] [Google Scholar]
- 13.Edelson D.P., Sasson C., Chan P.S., et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines(®)-resuscitation adult and pediatric task forces of the American Heart Association in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists: supporting organizations: American Association of Critical Care Nurses and national EMS physicians. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jansen G., Kipker K., Latka E., et al. High-quality chest compressions are possible during intra-hospital transport, but depend on provider position: a manikin study. Eur J Anaesthesiol. 2020;37:286–293. doi: 10.1097/EJA.0000000000001154. [DOI] [PubMed] [Google Scholar]
- 15.Couper K., Taylor-Phillips S., Grove A., et al. COVID-19 infection risk to rescuers from patients in cardiac arrest. Consensus on science with treatment recommendations: International Liaison Committee on Resuscitation (ILCOR) 2020. https://costr.ilcor.org/document/covid-19-infection-risk-to-rescuers-from-patients-in-cardiac-arrest
- 16.Chen J., Lu K.Z., Yi B., et al. Chest compression with personal protective equipment during cardiopulmonary resuscitation: a randomized crossover simulation study. Medicine (Baltimore) 2016;95:e3262. doi: 10.1097/MD.0000000000003262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ochoa F.J., Ramalle-Gómara E., Lisa V., et al. The effect of rescuer fatigue on the quality of chest compressions. Resuscitation. 1998;37:149–152. doi: 10.1016/s0300-9572(98)00057-4. [DOI] [PubMed] [Google Scholar]
- 18.Sayee N., McCluskey D. Factors influencing performance of cardiopulmonary resuscitation (CPR) by foundation year 1 hospital doctors. Ulster Med J. 2012;81:14–18. [PMC free article] [PubMed] [Google Scholar]