After allogeneic transplantation, comprehensive clinical follow-up is recommended for early detection of post-transplantation infections and other common complications such as endocrine disease or metabolic syndrome, and to ensure patients can enjoy quality of life. Long-term follow-up relies on a combination of primary disease monitoring, graft-versus-host disease (GVHD) surveillance and treatment, and long-term complications, such as secondary malignancy surveillance.
The pandemic of coronavirus disease 2019 (COVID-19) started spreading around the world in Feb 2020, presenting an unexpected challenge for transplantation services. In Italy, the first positive patient was identified on Feb 21, 2020, and as of Apr 23, 2020 more than 190 000 people have been diagnosed and over 25 000 have died. Northern Italy, where our stem cell transplantation programme is located, was rapidly overwhelmed. When the first patient with COVID-19 was diagnosed, we were faced with the dilemma of how to minimise the risk of infection while ensuring the delivery of the essential clinical care to our onco-haematological patients who received transplantation with a curative intent and were at high risk of developing clinically significant COVID-19 disease. Could we use telemedicine to follow-up patients after transplantation during the pandemic? Telemedicine can facilitate the interactions between patients, caregivers, and health-care providers, but could it be used to manage transplantation recipients, who are generally frail and have multiple comorbidities? Italy has the privilege of having a national health system (Servizio Sanitario Nazionale) since 1978, which relies on three fundamental principles: universality, solidarity, and uniformity. Even though much has been discussed on the potential benefit of telemedicine in the country in the past decade, little has been implemented so far. However, the COVID-19 pandemic has urgently pushed for the need to rethink the classic model of in-person consultations. Within 48 hours from the first COVID-19 diagnosis in Italy, physicians of our long-term follow up clinic organised telephone consultations with transplantation recipients, prioritising contact on the basis of time from transplantation and known individual post-transplantation complications. The first planned telephone call focused on areas of urgent intervention: assessment of signs or symptoms of infection, GVHD, or any signs of organ damage. The suggestion of infections or GVHD symptoms was further investigated through closed-ended questions aimed at identifying warning signs: “have you had dry mouth or difficulty swallowing dry food in the past 4 weeks?”, to address potential oral GVHD; or “have you noticed a dry cough in the past two weeks?”, to address the concern about infections. When visual examination was required (ie, onset of a skin rash), voice-only calls were replaced by video consultations. The consultations were summarised in the patients' electronic medical record.
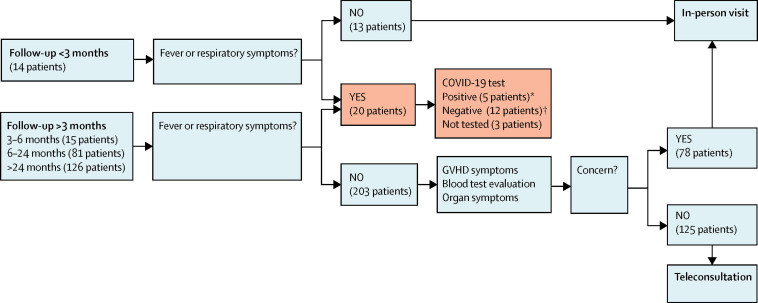
We started a risk versus benefit approach, by which patients who had less than 3 months of follow-up since transplantation and no suspected COVID-19 were all assessed through in-person visits (figure ). All patients with suspected COVID-19 were tested for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by nasopharyngeal swab and then managed by a dedicated COVID-multidisciplinary team if positive, or by the transplant physicians if negative. Patients with 3 or more months of follow-up after transplantation who did not have any COVID-19 symptoms were attended via teleconsultation if they did not show signs of transplantation-related complications, while those with organ toxicity or GVHD were assessed in-person.
Figure.
Patient distribution and decision-making flow-chart
Blue pathway=classic long-term follow-up; red pathway=COVID-19 dedicated follow-up. *Of five COVID-19-positive patients, three were hospitalised and two were followed-up via teleconsultation. †All COVID-19-negative patients were evaluated through an in-person visit.
Between Feb 24 and Mar 31, 2020, we contacted 236 (51%) of the 465 adult patients who received an allogeneic transplantation between Jan 1999 and Jan 2020 in our centre, applying our decision-making criteria (figure) to decide whether in-person visits were required. 14 (6%) patients had a follow-up of less than 3 months from transplantation, 15 (6%) had 3–6 months, 81 (34%) had 6–24 months, and 126 (53%) had more than 24 months follow-up. 50 (40%) of the 126 patients with more than 24 months follow-up were receiving immunosuppressive therapy for chronic GVHD, being at high risk of complications from infections. 21 (42%) of these 50 patients with chronic GVHD were evaluated in-person and 29 (58%) could be seen via teleconsultations. Of the 81 patients with 6–24 months follow-up, 24 (30%) are still under immunosuppressive therapy for chronic GVHD and 21 of them received an in-person visit at our long-term follow-up clinic. All patients with more than 24 months follow-up received a clinical evaluation since the outbreak started (75 [68%] of 110 patients an in-person visit and 35 [32%] had a teleconsultation). Only 20 (4%) of 465 patients who received a transplantation reported fever and respiratory symptoms suggestive of COVID-19; 17 (85%) of 20 were tested and 5 (25%) were confirmed COVID-19 cases. These patients were treated by a dedicated multidisciplinary team with full clinical resolution. The remaining 229 (49%) of 465 patients—all with a post-transplantation follow-up of more than 2 years—were contacted by e-mail to provide disease-specific information and explain how we were re-organising visits and teleconsultations in the long-term follow-up clinic.
Our next step will be to send an email survey to patients asking for feedback and preference between teleconsultations or in-person visits. We are also preparing standarised telephone questionnaires that address all possible complications post-transplantation, including physical function and quality of life, and special sections on the effect of isolation and physical distancing measures during the pandemic.
The medical emergency around COVID-19 did not allow our team to discuss important aspects of teleconsultations, such as medical liability or economic compensation for such consultations. The complete definition of the legal and financial framework for this kind of programme is our next challenge. The widespread use of internet connection, smartphones, and devices facilitate access to e-Health technologies. The sponsorship of government agencies would be crucial for the success of e-Health programmes at all levels; among multidisciplinary hospital teams, patients, caregivers, and community health providers. But ultimately, it is up to health care providers to guide patients on the virtuous use of these tools to promote equitable personalised medicine.
Our experience shows the feasibility of using telemedicine to maintain a long-term follow-up programme for transplantation patients. Physicians involved in this experience felt confident about the management of patients using teleconsultations, and patients—reassured that they were not left alone while in quarantine—provided positive feedback on our telemedicine approach. This framework was developed out of necessity in the context of COVID-19 but could be fostered in the post pandemic-era through an integrated model of care after transplantation. Similar teleconsultation programmes might be useful for managing patients undergoing intensive treatments in the future, such as those with acute leukemia or lymphoma.
For more on follow-up after allogeneic transplantation see Hematology Am Soc Hematol Educ Program 2019; 1: 626–29 and Biol Blood Marrow Transplant 2012; 18: 348–71
For more on the effect of the pandemic in Northern Italy see http://www.salute.gov.it/portale/home.html (accessed April 23, 2020)
For more on telemedicine's role during emergencies see JAMA Intern Med 2018; 178: 745–46 and N Engl J Med 2020; 382: 1679–81
Acknowledgments
The authors declare no competing interests