Abstract
It is widely believed that infection with the SARS-CoV-2 virus triggers a disproportionate immune response which causes a devastating systemic injury, particularly in individuals with obesity, itself a chronic, multi-organ inflammatory disease. Immune cells accumulate in visceral adipose tissue and together with paracrine adipocytes release a wide range of biologically active cytokines (including IL-1β, IL5, IL6 and IL8) that can result in both local, pulmonary and systemic inflammation. A more intense ‘cytokine storm’ is postulated as the mechanism behind the extreme immune response seen in severe COVID-19.
It is striking how dangerous the combination of obesity and COVID-19 is, resulting in a greater risk of ICU admission and a higher mortality. Furthermore, patients from a BAME background appear to have increased mortality after SARS-CoV-2 infection; they also have a higher prevalence of central obesity and its metabolic complications.
In the absence of an effective vaccine, the therapeutic potential of immune-modulating drugs is a priority, but the development of new drugs is expensive and time-consuming. A more pragmatic solution would be to seek to repurpose existing drugs, particularly those that might suppress the heightened cytokine activity seen in obesity, the major risk factor for a poor prognosis in COVID-19.
Montelukast is a cysteinyl leukotriene receptor antagonist licensed to treat asthma and allergic rhinitis. It has been shown to diminish pulmonary response to antigen, tissue eosinophilia and IL-5 expression in inflammatory cells. It has also been shown to decrease elevated levels of IL-1β and IL8 in humans with viral upper respiratory tract infections compared with placebo-treated patients. In addition, in silico studies have demonstrated a high binding affinity of the montelukast molecule to the terminal site of the virus’s main protease enzyme which is needed for virus RNA synthesis and replication.
Montelukast, which is cheap, safe and widely available would appear to have the potential to be an ideal candidate drug for clinical trials, particularly in early stage disease before irreparable tissue damage has already occurred.
Hypothesis
Through a direct anti-viral effect, or by suppression of heightened cytokine release in response to SARS-CoV-2, montelukast will reduce the severity of immune-mediated multiorgan damage resulting from COVID-19, particularly in patients with central obesity and metabolic syndrome.
Background
It is widely believed that infection with the SARS-CoV-2 virus triggers a disproportionate immune response which causes a devastating systemic injury, particularly in individuals with obesity, itself a chronic, multi-organ inflammatory disease. Immune cells accumulate in visceral adipose tissue and together with paracrine adipocytes release a wide range of biologically active cytokines (including IL-1β, IL5, IL6 and IL8) that can result in both local, pulmonary and systemic inflammation [1], [2], [3]. A more intense ‘cytokine storm’ is postulated as the mechanism behind the extreme immune response seen in severe COVID-19.
It is striking how dangerous the combination of obesity and COVID-19 is, resulting in a greater risk of ICU admission and a higher mortality [4], suggesting that the already heightened background inflammatory process resulting from obesity might prime the immune system for a more catastrophic response to SARS-CoV-2 infection. Furthermore, patients from a BAME background appear to have increased mortality after SARS-CoV-2 infection[5], an observation that has at least partly been explained by the higher prevalence of central obesity and its metabolic complications in this group [6], [7].
In the absence of an effective vaccine, exploring the therapeutic potential of immune-modulating drugs is a priority, but the development of new drugs is expensive and time-consuming. A more pragmatic solution would be to seek to repurpose existing drugs, particularly those that might suppress heightened cytokine activity as seen in obesity, the major risk factor for a poor prognosis in COVID-19.
Montelukast is a cysteinyl leukotriene receptor antagonist licensed to treat asthma and allergic rhinitis. It has been shown to diminish pulmonary response to antigen, tissue eosinophilia and IL-5 expression in inflammatory cells [8]. It has also been shown to decrease elevated levels of IL-1β and IL8 in humans with viral upper respiratory tract infections compared with placebo-treated patients [9]. In addition, in silico computer modelling studies have demonstrated a high binding affinity of the montelukast molecule to the SARS-CoV2 virus’s main protease enzyme substrate-binding pocket that is involved in virus RNA synthesis and replication [10], [11].
Evidence supporting montelukast as a candidate COVID-19 therapy in individuals with obesity
Hyperinflammation in COVID-19 patients
Patients affected by severe obesity share a common physiological response with patients with COVID-19 as both have raised concentrations of pro-inflammatory cytokines (e.g., TNF-a, IL1 and IL6) and T-helper-2 cytokines (IL4, IL10) [12], [13], [14]. Whilst it is impossible to exclude increased viral burden as the driver for this inflammatory response in COVID-19, there is evidence that some patients develop ‘cytokine storm (release) syndrome’, described as an uncontrolled and overwhelming release of proinflammatory mediators by an overly-activated immune system [12], [13], [15].
An overwhelming production of proinflammatory mediators in the lungs causes localised pulmonary injury characterised by diffuse alveolar damage with epithelial and endothelial apoptosis, and thrombosis due to dysregulated coagulation and fibrinolysis. These mediators may also leak into the systemic circulation leading to cardiac, renal and hepatic inflammation and multiorgan failure [16]. The background chronic inflammatory state associated with obesity could act as a catalyst for a massive inflammatory response to SARS-CoV-2 by priming an immune system subsequently triggered by the ‘second hit’ of COVID-19, and explaining why those with obesity are more likely to become severely ill, require ICU care and die. Severe lymphopenia with hyperactivated proinflammatory T cells and decreased regulatory T cells are commonly seen in critically ill COVID-19 patients supporting the likelihood of a dysregulated immune response to the viral infection [12].
The immune modulatory role of montelukast
Leukotrienes (LTC4, LTD4, and LTE4) are peptide-conjugated lipids that are prominent products of activated eosinophils, basophils, mast cells and macrophages [17], [18]. They are generated de novo from cell membrane phospholipid-associated arachidonic acid via the 5-lipoxygenase pathway. Known to cause contraction of bronchial smooth muscle, leukotrienes are now also recognised as potent inflammatory mediators that initiate and propagate a diverse array of biologic responses including macrophage activation, mast cell cytokine secretion and dendritic cell maturation and migration [17], [18].
Animal studies indicate a significant role for leukotrienes in adaptive immunity, particularly the induction of Th2 response in the lung via their effect on dendritic cells and cytokine generation (mainly IL4), the recruitment and/or activation of effector cells (especially eosinophils and mast cells), pulmonary inflammation, microvascular permeability and pulmonary fibrosis [17], [19].
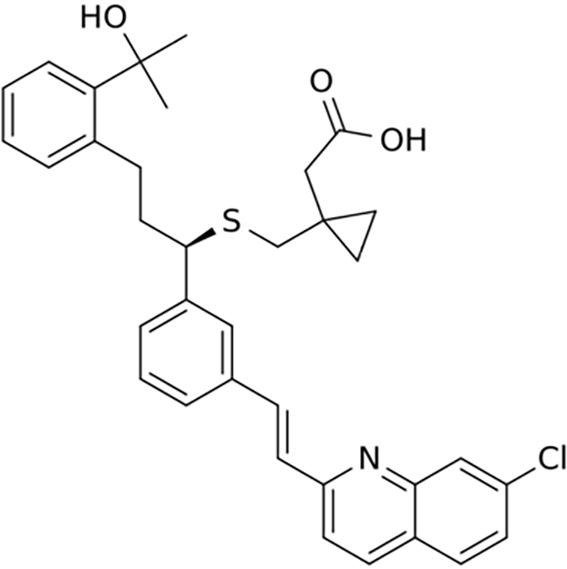
Montelukast [20], [21] (montelukast sodium: C35H36ClNO3S) is a leukotriene receptor antagonist which demonstrates a marked affinity and selectivity to the cysteinyl leukotriene receptor type-1, thus it elicits substantial blockage of any LTD4 leukotriene-mediated effect, resulting in reduced inflammation and relaxation of smooth muscle. It has also been shown to diminish the pulmonary response to antigen, tissue eosinophilia and the number of inflammatory cells expressing IL-5 [8]. Montelukast decreases elevated levels of IL-1β and IL8 in nasal washouts in humans with viral upper respiratory tract infections compared with placebo-treated patients [9]. Montelukast was first approved for clinical use by the US FDA in 1998. It is currently licensed to treat asthma, exercise-induced bronchospasm and allergic rhinitis.
Montelukast 10 mg is given orally once daily (oral bioavailability 64%). It is highly metabolised in the liver by cytochrome P450. The drug and its metabolites are almost exclusively excreted in the bile and into the faeces. With its prominent effect in reducing leukotriene-mediated cytokine release montelukast would have the potential to moderate the background inflammation associated with obesity and the body’s inflammatory response to SARS-CoV-2.
Targeted-effect of montelukast against SARS-CoV-2 main protease enzyme
Coronaviruses are enveloped viruses with a positive RNA genome. The virus contains at least four structural proteins: Spike (S) protein, envelope (E) protein, membrane (M) protein, and nucleocapsid (N) proteins [22], [23]. SARS-CoV-2 entry into the host cells is mediated by an interaction between the spike protein and angiotensin-converting enzyme 2 (ACE2) receptors [24], [25], cell surface proteins highly expressed in the lung, heart and kidney.
Wu et al. [10] performed in silico, target-based virtual ligand screening for SARS-CoV-2 main proteins including the main protease, spike protein, RNA-dependent RNA polymerase and papain-like protease. The authors screened approved drugs from a subset of the ZINC database which contains 2924 compounds [26]. They also screened a natural product database of 1,066 chemicals separated from traditional Chinese herbals and 78 known anti-viral drugs.
Their computer modelling study found that montelukast should demonstrate binding energy to the virus’s main protease enzyme. It fitted well into the active pocket of the main protease, in which hydrophobic amino acids would create a relatively hydrophobic environment to contain the drug and stabilise its conformation [10].
Similarly, a report by Farag et al. [11] predicted a high affinity of montelukast to the same binding domain in the main protease enzyme with hydrophobic-hydrophobic and hydrogen bond-interactions. Farag et al. [11] focussed on targeting the SARS-CoV-2 main protease enzyme at its two potential binding sites in the main substrate-binding pocket: the central site and terminal site.
The authors screened >2000 FDA-approved drugs to identify potential hits based on drug molecules’ binding energies, binding modes and the predicted interaction of amino acids with the enzyme’s substrate binding pockets. Whilst antiviral drugs unsurprisingly had the best binding to the central site of the main protease enzyme substrate-binding pocket, montelukast demonstrated a very high affinity for the terminal site, better than any other drug tested at this site
Whist drug binding in in silico modelling studies such as these may not translate into clinical effect, the protease enzyme is essential for the SARS-CoV-2 virus RNA synthesis and replication and if montelukast was shown to confer benefit in clinical studies it may be, at least in part, due to drug-induced disruption of the virus replication cycle.
Discussion
One of the main treatment strategies for COVID-19 is to identify new targeted anti-viral drugs based on the genomic information and pathological characteristics of SARS-CoV-2. These drugs are likely to be the most effective against the virus. However, anti-viral drug development and registration is time-consuming, the drug might not be available for the current outbreak and it is likely to be very expensive, an important factor particularly in poorer countries afflicted by COVID-19.
An alternative, faster strategy is ‘drug repurposing’. This relies on identification of potential therapeutic characteristics of drugs currently licensed for other purposes. There are many clinical trials enrolling patients with COVID-19 worldwide investigating the potential benefits of established antimicrobial, antiviral and anti-inflammatory drugs [27].
The strong association between the pro-inflammatory state found in metabolic syndrome and obesity and a more aggressive clinical course in COVID-19 suggests a potential treatment role for drugs that inhibit cytokine release and macrophage activation. There is, however, so far no convincing clinical evidence to support the use of corticosteroids, one of the most widely utilised anti-inflammatory agents. If anything, there is concern about patients being harmed with such a treatment [28], [29]. Anti-cytokines (interleukin 6 inhibitors, e.g., tocilizumab) have also attracted much interest recently [30] with a few ongoing clinical trials assessing their role [27]. However, these monoclonal antibodies are expensive and like corticosteroids have the potential for promoting secondary infections. Cost and complications are likely to limit their application on a global scale, other than selective use in severely ill patients [30], [31].
We believe there is a good theoretical basis to consider montelukast as a therapeutic candidate, with a hypothetical dual mode of action through suppression of cytokine activity and interference with viral replication. To date, the Cochrane COVID-19 Study Register does not identify any studies exploring the clinical benefits of montelukast.
Whilst it is unlikely that montelukast would be effective at curing COVID-19 or reversing severe immune-modulated multiorgan damage, it could have a powerful role in preventing disease progression when used at an early stage in the disease, reducing the need for hospital admission, or the requirement for the care of hospitalised patients to be escalated up to level 3 critical care. It may shorten the course of mild to moderate COVID-19 with the attendant social, economic and healthcare system benefits that would bring. Furthermore, it has a good safety profile.
But perhaps most importantly, if montelukast was shown to be of clinical benefit in well-conducted studies, it is a widely applicable treatment accessible to all patients, and at just over £4 per month [21], not just available to those who live in nations with first-world healthcare resources that can afford highly expensive new drugs.
Conflict of Interest
Neither of the authors have any conflicting interests and neither receive funding from any third party or external source.
Professor Kerrigan was the original creator of the hypothesis linking potential therapeutic benefits of montelukast in COVID-19, with the inflammatory state associated with obesity.
Both authors were involved in background research and the writing of the manuscript.
This paper did not require ethics approval.
References
- 1.Han M.S., White A., Perry R.J. Regulation of adipose tissue inflammation by interleukin 6. Proc Natl Acad Sci U S A. 2020;117(6):2751–2760. doi: 10.1073/pnas.1920004117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim C.S., Park H.S., Kawada T. Circulating levels of MCP-1 and IL-8 are elevated in human obese subjects and associated with obesity-related parameters. Int J Obes (Lond) 2006;30(9):1347–1355. doi: 10.1038/sj.ijo.0803259. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt F.M., Weschenfelder J., Sander C. Inflammatory cytokines in general and central obesity and modulating effects of physical activity. PLoS ONE. 2015;10(3) doi: 10.1371/journal.pone.0121971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Docherty A, Harrison E, Green C, et al. Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol [preprint] medRxiv 2020.04.23.20076042; doi: 10.1101/2020.04.23.20076042.
- 5.Georghiou T, Appleby J. Are more black, Asian and minority ethnic people dying with Covid-19 than might be expected? https://www.nuffieldtrust.org.uk/embed?contenttype=news&id=1290. Accessed 29th Apr 2020.
- 6.Tillin T., Forouhi N.G., McKeigue P.M., Chaturvedi N., Group S.S. Southall And Brent REvisited: cohort profile of SABRE, a UK population-based comparison of cardiovascular disease and diabetes in people of European, Indian Asian and African Caribbean origins. Int J Epidemiol. 2012;41(1):33–42. doi: 10.1093/ije/dyq175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khunti K., Singh A.K., Pareek M., Hanif W. Is ethnicity linked to incidence or outcomes of covid-19? BMJ. 2020;369 doi: 10.1136/bmj.m1548. [DOI] [PubMed] [Google Scholar]
- 8.Ihaku D., Cameron L., Suzuki M., Molet S., Martin J., Hamid Q. Montelukast, a leukotriene receptor antagonist, inhibits the late airway response to antigen, airway eosinophilia, and IL-5-expressing cells in Brown Norway rats. J Allergy Clin Immunol. 1999;104(6):1147–1154. doi: 10.1016/s0091-6749(99)70006-0. [DOI] [PubMed] [Google Scholar]
- 9.Schad C., Gentile D., Patel A., Koehrsen J., Schaffner T., Skoner D.P. Effect of montelukast on pro-inflammatory cytokine production during naturally acquired viral upper respiratory infections (vURIs) in adults. J Allergy Clin Immunol. 2008;121(2):S74. [Google Scholar]
- 10.Wu C., Liu Y., Yang Y. Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. Acta Pharm Sin B. 2020 doi: 10.1016/j.apsb/2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farag A., Wang P., Ahmed M., Sadek H. Identification of FDA approved drugs targeting COVID-19 virus by structure-based drug repositioning (Pre-print) ChemRxiv. 2020 [Google Scholar]
- 12.Qin C., Zhou L., Hu Z. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Z., Yang B., Li Q., Wen L., Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2019;2020 doi: 10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehta P., McAuley D.F., Brown M. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Channappanavar R., Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39(5):529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanaoka Y., Boyce J.A. Cysteinyl leukotrienes and their receptors: cellular distribution and function in immune and inflammatory responses. J Immunol. 2004;173(3):1503–1510. doi: 10.4049/jimmunol.173.3.1503. [DOI] [PubMed] [Google Scholar]
- 18.Peters-Golden M., Gleason M.M., Togias A. Cysteinyl leukotrienes: multi-functional mediators in allergic rhinitis. Clin Exp Allergy. 2006;36(6):689–703. doi: 10.1111/j.1365-2222.2006.02498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laitinen L.A., Laitinen A., Haahtela T., Vilkka V., Spur B.W., Lee T.H. Leukotriene E4 and granulocytic infiltration into asthmatic airways. Lancet. 1993;341(8851):989–990. doi: 10.1016/0140-6736(93)91073-u. [DOI] [PubMed] [Google Scholar]
- 20.Singulair (montelukast sodium) US FDA Label 2019 https://www.merck.com/product/usa/pi_circulars/s/singulair/singulair_pi.pdf.
- 21.British National Formulary (BNF) https://bnf.nice.org.uk/drug/montelukast.html. Accessed 29th Apr 2020.
- 22.Zumla A., Chan J.F., Azhar E.I., Hui D.S., Yuen K.Y. Coronaviruses – drug discovery and therapeutic options. Nat Rev Drug Discov. 2016;15(5):327–347. doi: 10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tortorici M.A., Veesler D. Structural insights into coronavirus entry. Adv Virus Res. 2019;105:93–116. doi: 10.1016/bs.aivir.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou P., Yang X.L., Wang X.G. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walls A.C., Park Y.J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(2):281–292.e286. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Irwin J.J., Sterling T., Mysinger M.M., Bolstad E.S., Coleman R.G. ZINC: a free tool to discover chemistry for biology. J Chem Inf Model. 2012;52(7):1757–1768. doi: 10.1021/ci3001277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorlund K, Dron L, Park J, Hsu G, Forrest J, Mills E. A real-time dashboard of clinical trials for COVID-19. Lancet. April 24, 2020 doi: 10.1016/ S2589-7500(20)30086-8. [DOI] [PMC free article] [PubMed]
- 28.Russell C.D., Millar J.E., Baillie J.K. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395(10223):473–475. doi: 10.1016/S0140-6736(20)30317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ritchie A.I., Singanayagam A. Immunosuppression for hyperinflammation in COVID-19: a double-edged sword? Lancet. 2020;395(10230):1111. doi: 10.1016/S0140-6736(20)30691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu B, Li M, Zhou Z, Guan X, Xiang Y. Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)? J Autoimmun 2020:102452. [DOI] [PMC free article] [PubMed]
- 31.Fu B., Xu X., Wei H. Why tocilizumab could be an effective treatment for severe COVID-19? J Transl Med. 2020;18(1):164. doi: 10.1186/s12967-020-02339-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


