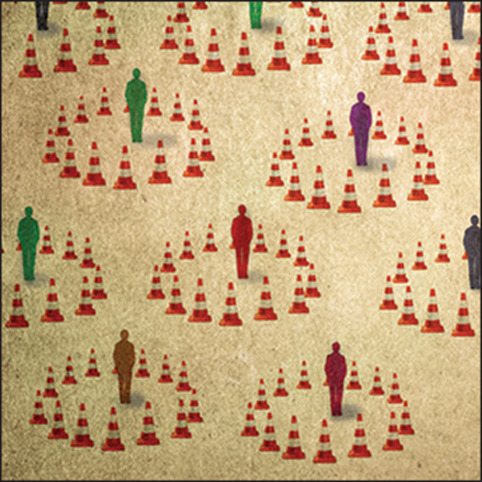
To date, over 4 million people globally have been infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), resulting in more than 250 000 deaths.1 Populations at particular risk include many of the most vulnerable sectors of society: incarcerated people, those residing in long-term care, minorities, and people with substance use disorders. Considering the high mortality rates attributable to the ongoing opioid overdose crisis, those who use illicit substances are now caught up in two simultaneous public health emergencies.2 This group might be additionally disadvantaged by barriers to the implementation of public health measures aimed at reducing virus transmission (eg, physical distancing) due to a myriad of social and structural issues including poverty, unstable employment, marginalisation, and homelessness, while having higher rates of comorbidities that portend worse outcomes if they become infected.
In response to these dual crises, health authorities have implemented policy changes to provide new tools to practitioners who treat patients with substance use disorders, circumventing previous barriers to treatment, such as inadequate access and prohibitively regimented medication management. For instance, in various North American jurisdictions buprenorphine plus naloxone can now be initiated by telehealth, pharmacists have been granted flexibility in adjusting doses for opioid agonist therapy, restrictions have been loosened on eligibility for take-home opioid agonist therapy, and delivery programmes have been established to bring methadone directly to homeless patients housed in isolation hotels.3, 4, 5 In the UK, the Advisory Council on the Misuse of Drugs has recommended that pharmacists be granted the authority to temporarily provide controlled medications without prescriptions, and adjust dispensing frequencies as needed.5 All of these measures are intended to help patients self-isolate and flatten the curve, but for many with especially severe substance use disorders they are insufficient.
In British Columbia, an epicentre of the overdose epidemic in Canada, unique steps are being taken to mitigate risk for people who use drugs in the context of SARS-CoV-2. The provision of regulated pharmaceutical-grade opioids has been discussed by public health officials and drug user advocates for years as a potential response to an overdose crisis driven by the infiltration of fentanyl into the illicit drug supply. These conversations have accelerated in the face of the additional threat posed by SARS-CoV-2. Clinical guidance published by the British Columbia Centre on Substance Use in collaboration with the provincial Ministry of Health has, for the first time, proposed an approach to prescribing these medications to patients with active substance use disorders who are thought to be at high risk for SARS-CoV-2.6 This harm-reduction measure includes providing unwitnessed doses of morphine, hydromorphone, dexamfetamine, methylphenidate, or a combination of these, to people whose current treatments (ie, methadone, buprenorphine plus naloxone) have not led to a sustained remission from drug use. These medications can be dispensed at varying frequencies, with patients having the discretion to use them however they find helpful to support them in their goal of physical distancing, alone or in combination with opioid agonist therapy.
At baseline, such an approach has been suggested to help curb the increasing rate of overdose deaths that have occurred since the arrival of fentanyl in the illicit drug supply. In the setting of current pandemic, these measures also help to promote physical distancing among people who use drugs by obviating the need to engage in high-risk behaviours to procure these substances. They are complemented by the ongoing provision of evidence-based harm-reduction strategies, including distribution of naloxone, sterile injection equipment, and access to safe injection sites (with capacity modified to promote physical distancing).7 Early anecdotal evidence (Sutherland C, Brar R, unpublished)suggests those receiving prescription alternatives to illicit drugs are able to avoid more routine contacts with drug dealers, and can reduce activities that might put them at risk of acquiring or transmitting SARS-CoV-2 (eg, sex work). An evaluation of the effect on other health outcomes, including rates of overdose deaths, is underway. The benefits of this approach on facilitating physical distancing and reducing use of illicit drugs will need to be assessed alongside the possible risks of drug diversion and other unanticipated harms.
People with substance use disorders face compounded risk in the context of SARS-CoV-2, and implementing physical distancing measures among this population presents unique challenges. Although evidence to address these issues remains limited, innovative strategies must be trialled and rapidly evaluated. Here, sensible public policy and clinical experience can be leveraged to develop an evolving solution to help protect some of the most susceptible populations. Ultimately, a prescription cannot solve the unprecedented morbidity and mortality that is a result of prohibition—this fact remains a social justice issue that will require fundamental regulatory and ideological changes to achieve sustainable improvement. In the meantime, health systems must bravely explore potential solutions to a complex problem that imminently threatens thousands of lives.
© 2020 Fanatic Studio/Gary Waters/Science Photo Library
This online publication has been corrected. The corrected version first appeared at thelancet.com/psychiatry on July 13, 2020
Acknowledgments
We thank Evan Wood for his mentorship and guidance in the preparation of this manuscript. All authors were involved in drafting and reviewing the Risk Mitigation in the Context of Dual Public Health Emergencies interim clinical guidance document published by the British Columbia Centre on Substance Use. PB is supported by a research grant from the Michael Smith Foundation for Health Research. PB, SR, CS, and RB all have financial support from the British Columbia Centre on Substance Use. CS previously held stock in the company Adamis Pharmaceuticals. All other authors declare no competing interests.
References
- 1.WHO . World Health Organization; Geneva: May 12, 2020. Coronavirus disease 2019 (COVID-19) situation report – 113.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200512-covid-19-sitrep-113.pdf?sfvrsn=feac3b6d_2 [Google Scholar]
- 2.Alho H, Dematteis M, Lembo D, Maremmani I, Roncero C, Somaini L. Opioid-related deaths in Europe: Strategies for a comprehensive approach to address a major public health concern. Int J Drug Policy. 2020;76 doi: 10.1016/j.drugpo.2019.102616. [DOI] [PubMed] [Google Scholar]
- 3.Knopf A. NYC begins home methadone deliveries. Will it have lasting impact on the rules? Filter. April 30, 2020. https://filtermag.org/new-york-home-methadone-delivery/
- 4.Substance Abuse and Mental Health Services; Rockyville: March 19, 2020. FAQs: provision of methadone and buprenorphine for the treatment of opioid use disorder in the COVID-19 emergency.https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf [Google Scholar]
- 5.Advisory Council on the Misuse of Drugs; London: April 7, 2020. COVID-19: ACMD advice on proposed legislative changes to enable supply of controlled drugs during a pandemic.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/878524/COVID-19_ACMD_advice_on_proposed_legislative_changes_to_enable_supply_of_controlled_drugs_during_a_pandemic1.pdf [Google Scholar]
- 6.Ahamad K, Bach P, Brar R. British Columbia Centre on Substance Use; Vancouver, Canada: 2020. Risk mitigation in the context of dual public health emergencies.https://www.bccsu.ca/wp-content/uploads/2020/04/Risk-Mitigation-in-the-Context-of-Dual-Public-Health-Emergencies-v1.5.pdf [Google Scholar]
- 7.Taha S, Maloney-Hall B, Buxton J. Lessons learned from the opioid crisis across the pillars of the Canadian drugs and substances strategy. Subst Abuse Treat Prev Policy. 2019;14:32. doi: 10.1186/s13011-019-0220-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


