Abstract
The Covid 19 epidemic has modified the way that plastic surgeons can treat their patients. At our hospital all elective surgery was canceled and only the more severe cases were admitted. The outpatient department activity has been reduced also. We present the number and diagnoses of patients, treated as in- and out-patients, during seven weeks from the onset of the epidemic, comparing our activity from the lockdown of elective surgery with the numbers and diagnoses observed during the same weeks of last year.
Finally we underline the importance of using telemedicine and web-based tools to transmit images of lesions that need the surgeon's evaluation, and can be used by the patient to keep in touch with a doctor during the distressing time of delay of the expected procedure.
Keywords: Covid-19, Plastic Surgery, Telemedicine, Corona virus pandemic
Introduction
On February, 21st 2020, the first case of Coronavirus Disease 2019 (COVID-19) was reported in Italy. Since then the disease rapidly expanded and on March 11, 2020, the World Health Organization (WHO) declared it to be a pandemic.1
As of April 6, 2020, Italy, with a number of deaths exceeding 16.500,2 10,000 physician infected and 94 doctors and 26 nurses dead, has the highest mortality and is the second most affected country worldwide after the United States, although other countries are rapidly increasing their number of patients. After the first case was diagnosed, hospitals were soon overcrowded by COVID-19 patients and many physicians, including plastic surgeons, were reassigned to the newly created COVID wards to manage the emergency.
This attempt of a rational use of medical resources, staff, devices and structures, has completely subverted the clinical practice, especially in hospitals.
Social distancing was implemented in Italy in successive phases (February 23, March 4 and 8) until, on March 9 and 11, the Government imposed a complete lockdown nationwide, aimed to contain the epidemic. From March 3, the Sant'Orsola University Hospital in Bologna, located in Emilia-Romagna, the second most affected Italian Region, started to admit to the Infectious Disease wards and in the Intensive Care Units, also patients from other areas of Northern Italy that were unable to cope with the rapidly increasing numbers of critically ill patients. However, the wards soon became insufficient and gradually other wards were transformed in COVID-19 Units, to admit the skyrocketing numbers of infected patients. To allow the appropriate use of all the hospital resources, surgical elective activity and in-site private practice were reduced on March 9 (together with the nationwide lockdown) and stopped altogether on Friday 13.
On March 13 the U.S. Surgeon General and a few days later the Centers for Medicare & Medicaid Services (CMS) recommended canceling all elective procedures.3 Similar recommendations were issued by the American College of Surgeons,4 the American Society of Plastic Surgeons and by many national scientific societies,5 including the Italian Society of Plastic Reconstructive and Aesthetic Surgery (SICPRE).6
However, the definition of elective surgery is not clear-cut. Elective procedures are often not optional and the patients' condition may worsen in the absence of timely surgical care.
The limitations imposed on transportation and people's movement, the increased risk of contagion for patients coming to waiting rooms and outpatient clinics, in addition to the fact that asymptomatic patients, unknowingly, could shed the virus exposing other inpatients, outpatients, and health care providers to the risk of contracting COVID-19, all called for alternative ways to manage the patients’ needs, both for a first Plastic Surgery consultation and for follow-up of a previous procedure.
We report here how our Department of Plastic Surgery faced the emergency situation brought about by the COVID 19 epidemic. We also measured the effects of the limitations imposed by the COVID-19 pandemic on the usual Plastic Surgery activity both on the number of procedures and their indications, and on the number of outpatient accesses. With the help of telemedicine and web-based tools we selected and followed patients during this time of lockdown.
Patients and methods
We established that patients with melanoma, Merkel carcinoma, infiltrative large squamous cell, and basal cell carcinoma, mainly of the face, had to be considered as surgical emergencies and their treatment was guaranteed. In addition, our team of plastic surgeons continued to be involved in multidisciplinary groups to provide reconstruction in other urgent cases, such as head & neck cancers, breast cancer, pelvic-perineal cancers, sarcomas or soft tissue infections such as necrotizing fasciitis.
All the patients already booked on an outpatient clinic at the time the switch from elective to urgent activity was implemented were contacted, on a daily basis, to evaluate the urgency of their case and to decide whether to cancel, postpone or maintain their appointment. In most cases this was done by a doctor, specific expertise being needed to judge the urgency and to assume the responsibility for the postponement.
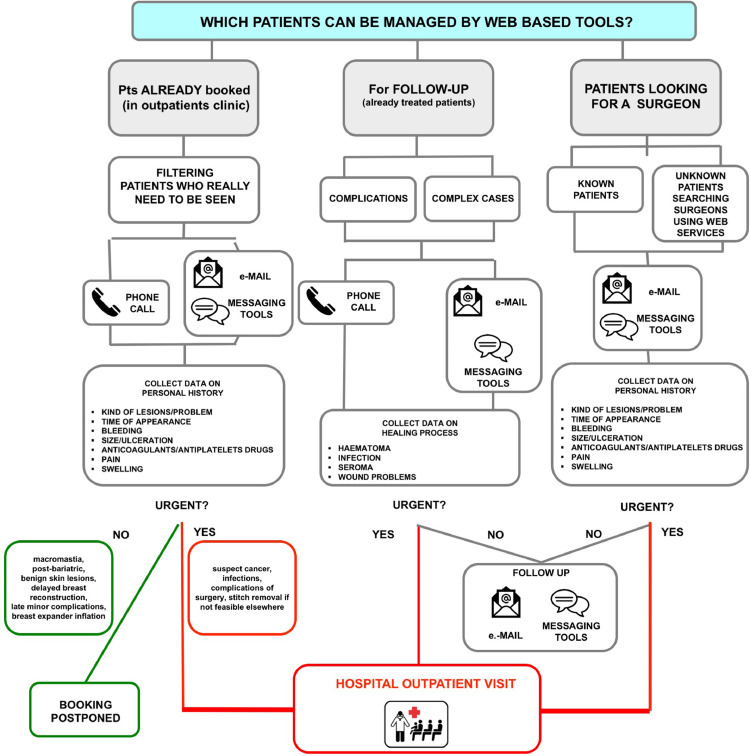
As explained in detail in Figure 1 , all the first appointments booked for non urgent problems (macromastia, post-bariatric reconstruction, benign skin lesions, delayed breast reconstruction, non-urgent breast reconstruction-related complications, breast expander inflation) were postponed and a new appointment was scheduled after 3–6 months (patients were advised to contact us if needed). The appointments of patients requiring urgent treatment (suspect cancer, infections, complications of surgery) were maintained as booked. For squamous or basal cell carcinomas and for various surgical complications the decision whether to keep or postpone the appointment depended on the severity of the case (Figure 2 ).
Figure 1.
The flowchart explains which patients can be managed by telemedicine: patients already booked in outpatients clinic; patients needing follow up for previous surgeries (either complicated or complex to manage at home); patients looking for a surgeon (and not booked yet).
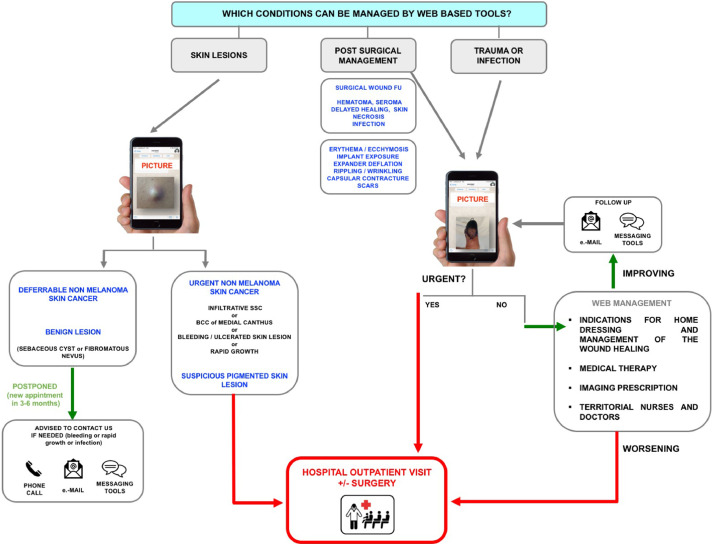
Figure 2.
The flowchart exemplifies some of the conditions that can be managed by telemedicine: Skin lesions, wounds management after surgery (including complications), urgent conditions such as trauma and infection.
The decision whether to keep or postpone the appointment was related to the severity of the case.
The appointments for large, bleeding, rapidly growing, or dangerously located squamous and basal cell carcinomas were kept as booked. In all other cases, prescriptions or suggestions for conservative treatment were given and the appointment postponed to 3–6 months. For the patients of this “uncertain group” the use of telemedicine and web-based tools was particularly useful to decide whether a visit was necessary, and also to follow the evolution of the problem (Figure 2).
All the patients booked at the outpatient clinic for the following day, for whom the need to be seen at the hospital was uncertain, were contacted by telephone. To gain more visual information of the clinical condition, after clarifying the privacy matters and obtaining consent, the patients were invited to send pictures of the lesion that should be evaluated. The patients chose the web -based tool, email or messaging apps (e.g. Whatsapp, Telegram, Messenger), they were more familiar with. On the basis of the image, further decisions were taken.
Changes in the number and type of surgical procedures
The overall “COVID-19” period examined was from Monday, February 17 (a few days before the first COVID-19 case diagnosed in Italy) to Friday, April 3 2020, for a total of 7 weeks.
The “pre-COVID-19” period used as a control went from Monday, February 18 to Friday, April 5 2019, for the same number of weeks.
Consulting the Hospital database, we collected the number of all surgical procedures performed by plastic surgeons on patients admitted to the University Hospital or in the satellite hospitals during the two periods.
Also, we collected the number of patients accessing the Plastic Surgery outpatient clinic and the reason for access (Figures 3 and 4 ).
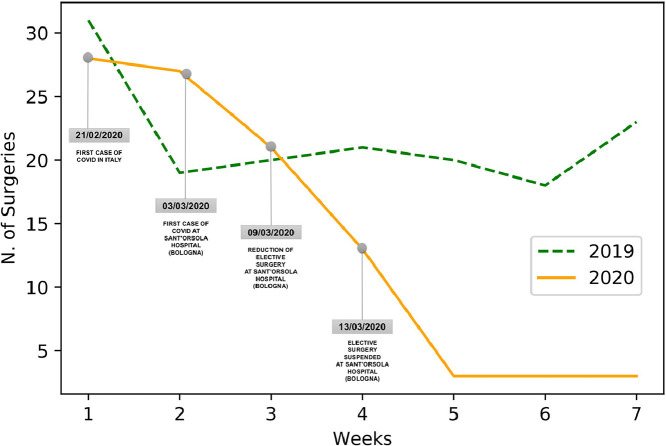
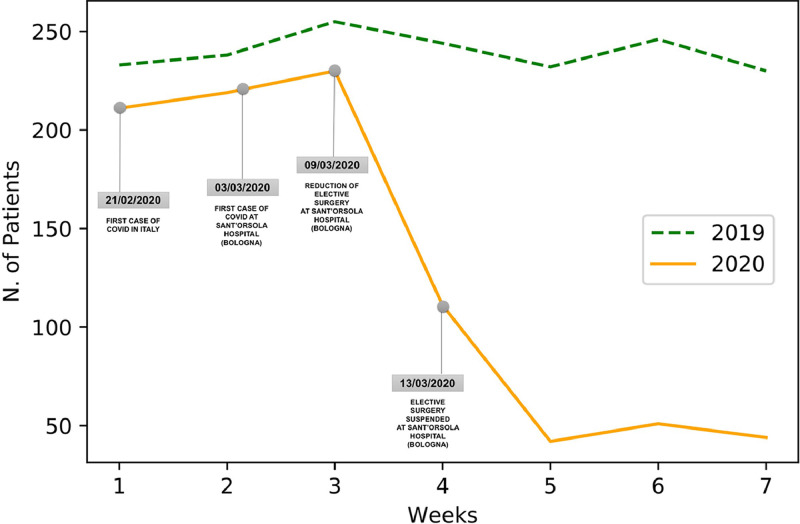
Figure 3.
The surgical activity during the overall “COVID-19” period (7 weeks 2020) and during the corresponding period of 2019 are shown.
Important dates are shown February 21: first COVID-19 in Italy. March 3: first COVID-19 patients at the Sant'Orsola University Hospital. March 9: limitation of elective surgery. March 13: STOP of elective surgery.
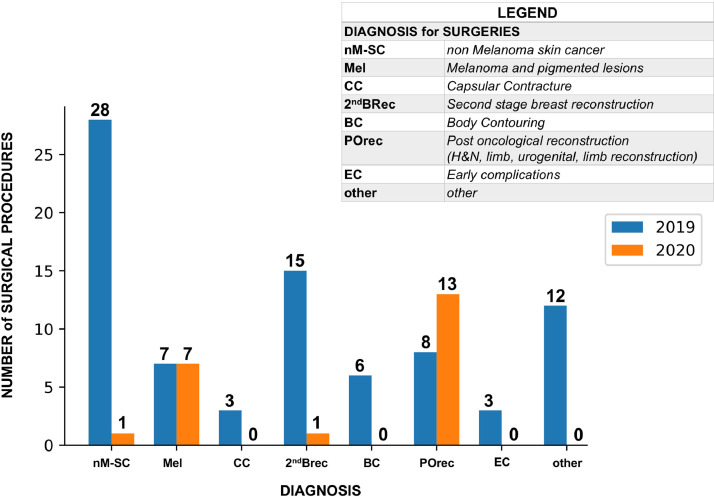
Figure 4.
The chart shows, only for the 4 weeks after lockdown, the different diagnosis for surgery, and their numbers, in comparison with the same 4 weeks of 2019.
Statistics
Data analysis and data manipulation have been developed using Python's library Pandas while all the images have been produced using Matplotlib library.
Results
Changes in case load and types of procedures
Surgical procedures
In the entire “COVID-19” period (7 weeks 2020) 98 surgical procedures were performed (78 at the University hospital, 20 at the satellite hospitals).
The activity had a gradual reduction in the first 5 weeks and reached a nadir at week 5, after closure of the elective activity (Friday, March 13, week 4).
In the “pre-COVID-19” 7 weeks period (2019) 152 surgical procedures were performed (109 at the University hospital, 43 at the satellite hospitals).
To obtain a more precise comparison between the activity after elective lockdown and previous activity, the 4-week period from March 9 (reduction and then stop of elective surgery) to April 4 2020, and the corresponding 2019 period were compared.
As expected, the reduction of surgical activities was evident when comparing the two 4 weeks periods.
Outpatient clinic
In the “COVID-19” period (7 weeks 2020), patients accessed 908 times the Plastic Surgery outpatient clinic compared to 1678 times on the “pre-COVID-19” period (Figure 5 and Table 1 ).
Figure 5.
The Plastic Surgery outpatient clinic activity during the overall “COVID-19” period (7 weeks 2020) and during the corresponding period of 2019 are shown.
Important dates are shown February 21: first COVID-19 in Italy. March 3: first COVID-19 patients at the Sant'Orsola University Hospital. March 9: limitation of elective surgery. March 13: STOP of elective surgery.
Table 1.
The numbers of outpatient clinic access, outpatient minor surgery procedures and surgical procedures are shown during the 7 weeks period and the 4 weeks of lockdown, in comparison to the same periods of 2019.
| 2020 |
2019 |
||||
|---|---|---|---|---|---|
|
7 weeks activity 17 February 2020–3 April 2020 |
4 weeks activity 9 March 2020–3 April 2020 |
7 weeks activity 18 February 2019–5 April 2019 |
4 weeks activity 11 March 2019–5 April 2019 |
||
| Outpatient clinic access | 908 | 248 | 1678 | 952 | |
| Outpatient minor surgeries | 108 | 29 | 200 | 121 | |
| Surgical procedures | Sant'Orsola hospital (Bologna) | 78 | 21 | 109 | 58 |
| Satellite hospitals | 20 | 1 | 43 | 24 | |
| Total | 98 | 22 | 152 | 82 | |
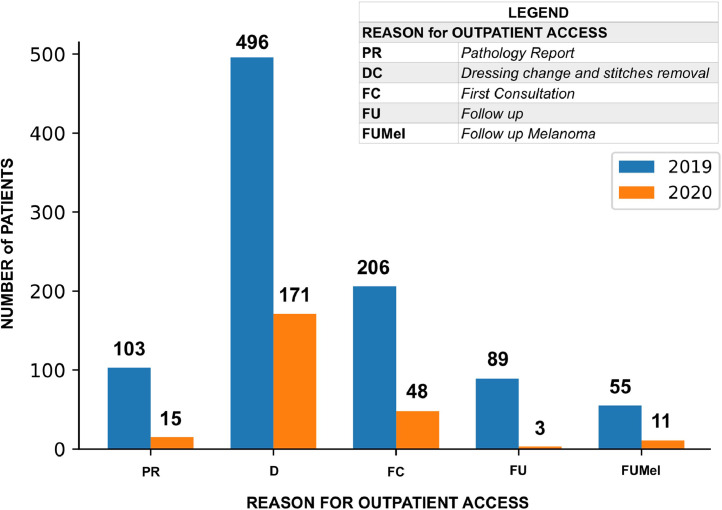
The reasons for access during the 4 weeks 2020 from March 9 (reduction and then stop to elective surgery) to April 4 2020, after stop of elective procedures and the correspondent ones of 2019 are shown in Figure 6 .
Figure 6.
Comparison of the reasons for access to the Outpatient clinic during the 4 last weeks 2020, after stop of elective activity, and the correspondent ones of 2019.
Outpatient minor surgeries
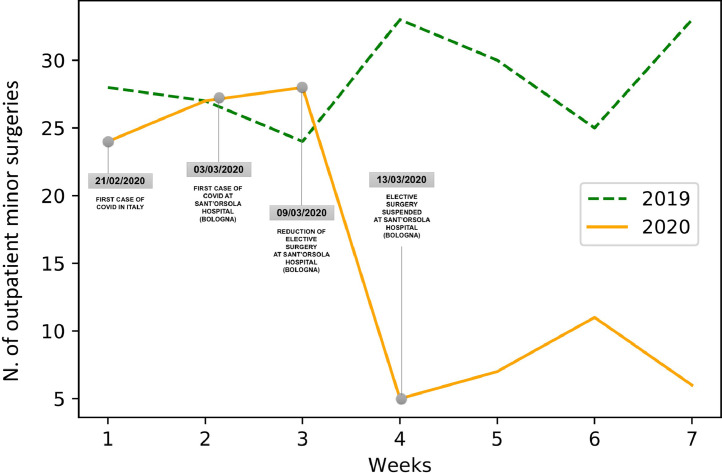
In the “COVID-19” period (7 weeks 2020), 108 surgical procedures were performed at the Plastic Surgery outpatient Minor Surgeries under local anaesthetic compared to 200 procedures on the “pre-COVID-19” period (Figure 7 and Table 1).
Figure 7.
The chart shows the outpatient Minor Surgery (local anaesthetic) activity during the overall “COVID-19” period (7 weeks 2020) and during the corresponding period of 2019.
Important dates are shown February 21: first COVID-19 in Italy. March 3: first COVID-19 patients at the Sant'Orsola University Hospital. March 9: limitation of elective surgery. March 13: STOP of elective surgery.
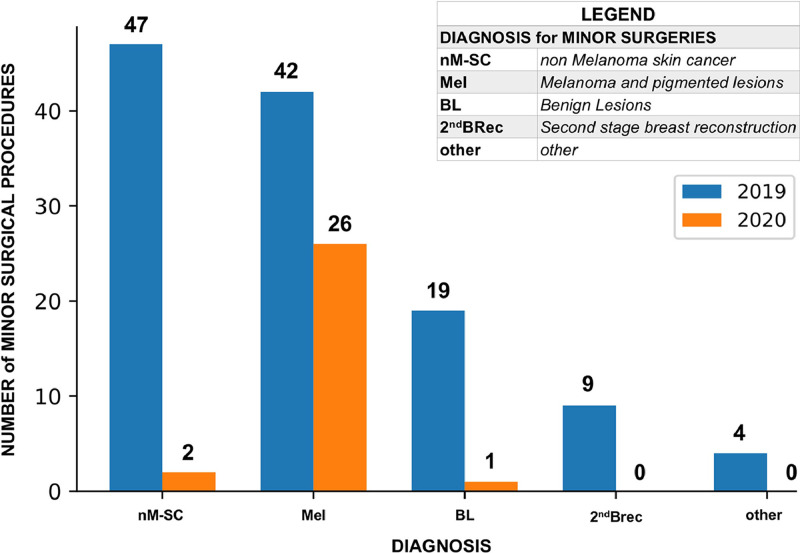
A comparison between the diagnosis for minor surgery in the 4 last weeks 2020 after stop of electives and the correspondent ones of 2019 is shown in Figure 8 .
Figure 8.
Comparison of the diagnosis for Minor Surgery in the 4 last weeks 2020, after stop of elective activity, to the correspondent ones of 2019.
Number of patients operated, accessing outpatient clinic and treated in the outpatient minor surgeries unit are shown in Table 2 . Their gender, age, and geographical origin are detailed.
Table 2.
Patients’ demographics for all the patients treated in the in the 4 weeks of 2020 (after stop of elective activity) in comparison to the correspondent weeks of 2019 are shown.
Number of patients, their gender, age and geographical origin.
| Demographic data for the 4 weeks activity 2020: 9 March–3 April 2019: 11 March–5 April | ||||||
|---|---|---|---|---|---|---|
| Surgical procedures |
Outpatient clinic access |
Outpatient minor surgeries |
||||
| 2020 | 2019 | 2020 | 2019 | 2020 | 2019 | |
| Numbers | 22 | 82 | 248 | 952 | 29 | 121 |
| Gender | ||||||
| Male | 6 | 32 | 88 | 342 | 12 | 55 |
| Female | 16 | 50 | 160 | 610 | 17 | 66 |
| Age (years) | ||||||
| Range | 43–88 | 2–97 | 21–95 | 1–99 | 23–90 | 16–89 |
| Average | 59 | 62 | 59 | 58 | 53 | 58 |
| Origin | ||||||
| Bologna | 215 | 768 | 27 | 103 | ||
| Extra | 33 | 184 | 2 | 18 | ||
Alternative methods of patients’ evaluation and follow up
The decisional flow chart that we applied for the screening of outpatients and follow-up of operated patients is shown in detail in Figure 1.
Figure 2 shows which Plastic Surgery conditions were managed by web based tools during the pandemic and how.
All patients expressed their satisfaction for the web-based modality of evaluation and follow-up that simplified the procedure, avoided logistic problems especially in the lockdown situation and reduced chances of contagion.
Discussion
Changes in case load and types of procedures
As expected, a significant reduction of the total number of surgical procedures was seen in the “COVID-19” period compared to the usual activity. The reasons for surgery also changed significantly. As required by the reorganization of the hospital activity, only patients with a diagnosis of malignancy were operated on during the COVID-19 period.
No urgent surgery for infection, haematomas, necrosis, delayed wound healing or other complications was performed in the study period. If, on one hand, this might be justified by the reduced number of technically demanding procedures, such as elective free flaps, or extensive surgeries like abdominoplasty or breast reduction, this may also be due to a general reduction in access to the emergency room. Overall, the non-COVID-19 use of the emergency room was greatly reduced, both because of the limitations in movement imposed to the population (with consequent less accidents and crime) and by the fear of getting infected inside the hospital's premises. In fact, the cardiology association has issued a warning on the increased numbers of heart-related deaths because of the reluctance of the patients to go to the hospital.7, 8, 9, 10
The consequences of canceling elective surgery are difficult to foresee. As stated in a recent Editorial,11 many elective non-urgent surgeries will become urgent at some point in time, and therefore we will probably face a consistent back-log of procedures that we'll need to perform when the COVID-19 epidemic will end (nobody still knows when).12
The delayed surgeries that we will certainly need to perform in the future are the squamous and basal cell carcinomas that, at the moment, are only treated when severe and progressive.
It is possible that these skin cancers will grow in the next months, requiring a more complex surgical approach.4
How will the hospital organization change after Covid-19? As many opinion makers say, this epidemic will force all of us to reconsider, and possibly change, many aspects of our living style. This is true also for the health system. As an example, the consistent reduction in number of patients accessing the outpatient clinic demonstrates that a considerable amount of work could benefit from reorganization. The follow-up visits after minor surgeries performed under local anaesthesia could be avoided by using only subcutaneous reabsorbable sutures and providing adequate training for stitch removal and dressing to the personnel already working in the territorial ambulatory services.
Another example concerns the pathology reports that, before COVID-19, were given to the patient in the outpatient clinic, in order to explain the diagnosis and the plan for subsequent surgical or medical interventions. During the epidemic, all the patients who had undergone a biopsy were contacted by telephone, the report was explained, sent by email and only a subset of the patients were invited to return to the hospital.
Alternative methods of patients evaluation and follow up
In what may be the first pandemic of the social-media age, plastic surgeons are trying to manage patients remotely, in real time, by using online services. Telemedicine has been in use for a long time in some countries Including, among others, the United Kingdom, Scandinavia, North America, Bolivia, Brazil, and Australia, especially where big distances and a low population density made it necessary.13, 14, 15 With the evolution of modern technology and of the internet web applications, the interest for telemedicine has expanded to more countries and medical specialities, including Plastic Surgery.16 Due to the “visual nature” of their field, plastic surgeons have pioneered the professional use of social networks. Often, the commercial nature of cosmetic surgery has played a role in the use of the internet.17, 18, 19, 20, 21 However the use of internet tools for monitoring reconstructive surgery patients has been largely described.22, 23, 24 Instant sharing of images or video calls allow plastic surgeons to make an easy consultation, filtering only clinical cases that really need to be evaluated in person for an adequate treatment.
These tools provide different and complementary functions allowing different levels of communication possibly with different levels of privacy.20 , 25, 26, 27, 28
Gardiner and Hartzell,29 in this journal, have highlighted applications, limitations and pitfalls of Telemedicine.
Copyrighted material is shared through personal messages according to each own social media copyright policy.30, 31, 32, 33
To avoid legal action for malpractice in telemedicine, it is mandatory for the surgeons to establish appropriate boundaries in online communication with patients, keeping highest ethical and deontological standards in physician-patient relationship.28 , 29 , 34
The importance of these legal and privacy limitations was recognized (February 2020) by the United States Department of Health and Human Services that recently liberalized the Health Insurance Portability and Accountability Act (HIPAA) compliance guidelines for the COVID-19 pandemic, allowing the use of video communication tools.35, 36, 37
Unfortunately, while the Web can be ideal for some conditions, it may represent an insufficient and inappropriate means to approach critically ill patients.
Telemedicine and the Web tools during the COVID-19 emergency have allowed a reduction in hospital access for the patients and have promoted a stricter interactive communication between hospital surgeons, general practitioners and territorial nurses, hopefully creating the basis for an interesting new working way for the post COVID 19 era that may include a regular, dedicated telemedicine/telehealth working shift for a plastic surgeon to deal remotely with non urgent conditions.
Conclusions
The destructive effect of COVID 19 in our lives has changed also the working way of hospitals. In our Department of Plastic Surgery, in the second most affected Region in Italy, the number of patients admitted to hospital for elective procedures greatly decreased, surgery being limited to malignancies.
In the outpatient department, where also the number of patients have been reduced to 26% of the previous load, a great help to surgeons was given by the internet. In fact it was possible for the surgeons to make an approximate diagnosis on the basis of the images provided by the patients and for the patients to feel connected with the surgeons, despite the lockdown.
These web based tools, allow patients to communicate with their treating surgeons, not only to discuss medical problems but also to express psychological frailties due to the delaying of treatment.
The internet resources, however, cannot completely replace the direct diagnostic opinion nor the human relationship.
Declaration of Competing Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Acknowledgments
Funding
The authors received no financial support for the research, authorship, and publication of this article.
References
- 1.Zoia C., Bongetta D., Veiceschi P. Neurosurgery during the COVID-19 pandemic: update from Lombardy, Northern Italy. Acta Neurochir. 2020;162:1221–1222. doi: 10.1007/s00701-020-04305-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Italian Ministry of Health. 2020. http://www.salute.gov.it. [Accessibility verified April 6, 2020].
- 3.Centers for Medicare & Medicaid Services, CMS, part of the Department of Health and Human Services (HHS). https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental. [Accessibility verified April 6, 2020]
- 4.American College of Surgeons. https://www.facs.org/covid-19/clinical-guidance/triage. [Accessibility verified April 6, 2020]
- 5.American Society of Plastic Surgeons. http://email.plasticsurgery.org/q/12EC50dbrptNnCCaBimf8m0W/wv. [Accessibility verified April 6, 2020]
- 6.Italian Society of Plastic Reconstructive and Aesthetic Surgery. https://www.sicpre.it/emergenza-coronavirus-le-raccomandazioni-della-sicpre/. [Accessibility verified April 6, 2020]
- 7.PanoramaSanità. Italian Health Magazine. http://www.panoramasanita.it/2020/04/01/covid-19-allarme-cardiologi-internisti-si-continua-a-morire-di-infarto-ma-sui-ricoveri-vince-la-paura-del-contagio/. [Accessibility verified April 6, 2020]
- 8.Italian Society of Interventional Cardiology (GISE). 2020. https://gise.it [Accessibility verified April 6, 2020].
- 9.Tarantini G., Fraccaro C., Chieffo A. Italian Society of Interventional Cardiology (GISE) position paper for Cath lab-specific preparedness recommendations for healthcare providers in case of suspected, probable or confirmed cases of COVID-19. Catheter Cardiovasc Interv. 2020:1–5. doi: 10.1002/ccd.28888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Covid-19 protocol. Italian Society of Interventional Cardiology (GISE). 2020. https://gise.it/Uploads/EasyCms/Protocollo%20Covid%2019_54321.pdf. [Accessibility verified April 6, 2020].
- 11.Stahel P.F. How to risk-stratify elective surgery during the COVID-19 pandemic? Patient Saf Surg. 2020;14:8. doi: 10.1186/s13037-020-00235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.What It Really Means to Cancel Elective Surgeries. The Atlantic. 2020. https://www.theatlantic.com/science/archive/2020/03/patients-whose-surgeries-are-canceled-because-coronavirus/608176/. [Accessibility verified April 6, 2020].
- 13.Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth 2009. WHO Global Observatory for eHealth. 2010. https://www.who.int/goe/publications/goe_telemedicine_2010.pdf. [Accessibility verified April 6, 2020].
- 14.Zanaboni P., Wootton R. Adoption of routine telemedicine in Norwegian hospitals: progress over 5 years. BMC Health Serv Res. 2016;16:496. doi: 10.1186/s12913-016-1743-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Currell R., Urquhart C., Wainwright P., Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2000;(2) doi: 10.1002/14651858.CD002098. [DOI] [PubMed] [Google Scholar]
- 16.Wallace D.L., Jones S.M., Milroy C., Pickford M.A. Telemedicine for acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg. 2008;61(1):31–36. doi: 10.1016/j.bjps.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 17.Wheeler C.K., Said H., Prucz R. Social media in plastic surgery practices: emerging trends in North America. Aesthetic Surg J. 2011;31:435–441. doi: 10.1177/1090820X11407483. [DOI] [PubMed] [Google Scholar]
- 18.Italian Society of Plastic Reconstructive and Aesthetic Surgery. Facebook page. 2020. https://www.facebook.com/sicpre/. [Accessibility verified April 6, 2020].
- 19.Italian Society of Plastic Reconstructive and Aesthetic Surgery. 2020. https://www.sicpre.it/. [Accessibility verified April 6, 2020].
- 20.Branford O.A., Kamali P., Rohrich R.J. #PlasticSurgery. Plast Reconstr Surg. 2016;138(6):1354–1365. doi: 10.1097/PRS.0000000000002814. [DOI] [PubMed] [Google Scholar]
- 21.Varkey P., Tan N.C., Girotto R., Tang W.R., Liu Y.T., Chen H.C. A picture speaks a thousand words: the use of digital photography and the Internet as a cost-effective tool in monitoring free flaps. Ann Plast Surg. 2008;60(1):45–48. doi: 10.1097/SAP.0b013e31805003df. [DOI] [PubMed] [Google Scholar]
- 22.Engel H., Huang J.J., Tsao C.K. Remote real-time monitoring of free flaps via smartphonephotography and 3G wireless Internet: a prospective study evidencing diagnostic accuracy. Microsurgery. 2011;31(8):589–595. doi: 10.1002/micr.20921. [DOI] [PubMed] [Google Scholar]
- 23.Hwang J.H., Mun G.H. An evolution of communication in postoperative free flap monitoring: using a smartphone and mobile messenger application. Plast Reconstr Surg. 2012;130(1):125–129. doi: 10.1097/PRS.0b013e318254b202. [DOI] [PubMed] [Google Scholar]
- 24.Rao R., Shukla B.M., Saint-Cyr M., Rao M., Teotia S.S. Take two and text me in the morning: optimizing clinical time with a short messaging system. Plast Reconstr Surg. 2012;130(1):44–49. doi: 10.1097/PRS.0b013e3182547d63. [DOI] [PubMed] [Google Scholar]
- 25.Ben Naftali Y., Duek O.S., Rafaeli S., Ullmann Y. Plastic surgery faces the web: analysis of the popular social media for plastic surgeons. Plast Reconstr Surg Glob Open. 2018;6(12) doi: 10.1097/GOX.0000000000001958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mabvuure N.T., Rodrigues J., Klimach S., Nduka C. A cross-sectional study of the presence of United Kingdom (UK) plastic surgeons on social media. J Plast Reconstr Aesthet Surg. 2014;67(3):362–367. doi: 10.1016/j.bjps.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 27.Cho M.J., Furnas H.J., Rohrich R.J. A primer on social media use by young plastic surgeons. Plast Reconstr Surg. 2019;143(5):1533–1539. doi: 10.1097/PRS.0000000000005533. [DOI] [PubMed] [Google Scholar]
- 28.Eberlin K.R., Perdikis G., Damitz L. Electronic communication in plastic surgery: guiding principles from the American society of plastic surgeons health policy committee. Plast Reconstr Surg. 2018;141(2):500–505. doi: 10.1097/PRS.0000000000004022. [DOI] [PubMed] [Google Scholar]
- 29.Gardiner S., Hartzell T.L. Telemedicine and plastic surgery: a review of its applications, limitations and legal pitfalls. J Plast Reconstr Aesthet Surg. 2012;65(3):e47–e53. doi: 10.1016/j.bjps.2011.11.048. [DOI] [PubMed] [Google Scholar]
- 30.Camp S.M., MD, Mills D.C., II, MD The marriage of plastic surgery and social media: a relationship to last a lifetime. Aesthet Surg J. 2012;32(3):349–351. doi: 10.1177/1090820X12439862. [DOI] [PubMed] [Google Scholar]
- 31.Patel A., Pfaff M., Tuggle C.T. The plastic and reconstructive surgery Facebook page: newfound treasure. Plast Reconstr Surg. 2013;132:189e. doi: 10.1097/PRS.0b013e3182910e8d. [DOI] [PubMed] [Google Scholar]
- 32.Dauwe P., Heller J.B., Unger J.G. Social networks uncovered: 10 tips every plastic surgeon should know. Aesthet Surg J. 2012;32:1010–1015. doi: 10.1177/1090820X12462027. [DOI] [PubMed] [Google Scholar]
- 33.Facebook: statement of rights and responsibilities. 2014. https://www.facebook.com/legal/terms. [Accessibility verified April 6, 2020]
- 34.Aicher R.H. Internet liability. Aesthet Surg J. 2000;20:433. doi: 10.1016/s1090-820x(98)70048-2. [DOI] [PubMed] [Google Scholar]
- 35.Department of Health and Human Services, USA. 2020. https://www.hhs.gov/sites/default/files/covid-19-hipaa-and-first-responders-508.pdf [Accessibility verified April 6, 2020].
- 36.Department of Health and Human Services, USA. BULLETIN: HIPAA Privacy and Novel Coronavirus. 2020. https://www.hhs.gov/sites/default/files/february-2020-hipaa-and-novel-coronavirus.pdf [Accessibility verified April 6, 2020].
- 37.Calton B., Abedini N., Fratkin M. Telemedicine in the time of coronavirus. J Pain Symp Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.019. S0885-3924(20)30170-6 [published online ahead of print, 2020 Mar 31] [DOI] [PMC free article] [PubMed] [Google Scholar]