Highlights
-
•
The prognosis of critical cases of COVID-19 might be changed if a timely intervention of EBP was performed.
-
•
EBP may help to attenuate the progression of ARDS.
-
•
Evaluating FDPs as a sensitive marker of injury and prognosis of COVID-19 is warranted.
Keywords: COVID-19, Cytokine storm, ARDS, Extracorporeal blood purification
Abstract
COVID-19 associated cytokine storm could rapidly induce ARDS, and the patients would require mechanical ventilation. However, the prognosis was not that optimistic. The outcome might be changed if the timely intervention of EBP was performed. We present a case of severe SARS-CoV-2 infection who recovered from a cytokine storm.
Background
The novel coronavirus disease (COVID-19) has now broken out throughout the world. The total number of deaths has been over 88,900 up to now. Patients with confirmed COVID-19 progressed to acute respiratory distress syndrome (ARDS) rapidly with an incident rate as high as 41.8% (Wu et al., 2020); many of them require mechanical ventilation. In a cohort of an intensive care unit (ICU) from Italy, 1287 cases needed respiratory support, and among them, 88% of patients (1150 cases) had to be supported with mechanical ventilation (Grasselli et al., 2020). Apart from the desperate shortage of ventilators all over the world, mechanical ventilation may cause barotrauma and ventilator-associated lung injury.
Cytokine storm has been disclosed as a main pathological characteristic of COVID-19 (Huang et al., 2020), and it is also the direct pathogenic contributor to induce ARDS. Cytokines may be effectively eliminated by extracorporeal blood purification (EBP) (Honore et al., 2019a), which can interrupt the initiation and progression of an inflammation cascade in the scenario of COVID-19. Accordingly, EBP may offer a chance of avoiding intubation and mechanical ventilation. Here, we report a case of severe SARS-CoV-2 infection with cytokine storm, who wholly recovered using extracorporeal blood purification.
Case presentation
A 62-year-old male presented to the hospital with an 8-day history of fever and a 6-day history of cough and chest distress. The patient had a history of gallstones. He developed a fever on day one (February 14, 2020) and had a chill, headache, muscle soreness, fatigue, nausea, cough, chest distress, and shortness of breath on day three. Then, he was quarantined in a hotel. Having been tested positive for SARS-CoV-2 on day five, he received oseltamivir, moxifloxacin, and Lianhua Qingwen capsule (Chinese medicine) in the outpatient ward.
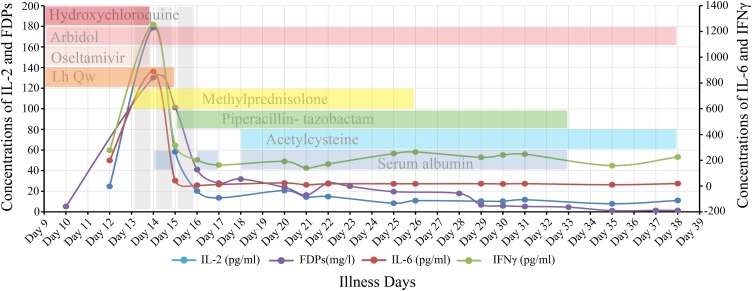
He was admitted to the hospital with fever, cough, and mild chest distress on day nine. Arbidol, hydroxychloroquine, oseltamivir, and Lianhua Qingwen capsule were administered. Supplemental oxygen was delivered by nasal cannula at 2 L/min. Alterations in hepatic function were found: levels of alanine aminotransferase (81 U/L, normal range: 9–50 U/L) and aspartate aminotransferase (94 U/L, normal range: 15–40 U/L) were elevated, and CD3 and CD4 cell counts were markedly decreased (Supplemental Table) on day ten. Chest CT indicated multiple ground-glass opacities in both lungs on day eleven (Supplemental Figure 1A–C). The highest temperature was 38.5 °C up to date. His vital signs remained clinically stable, except oxygen saturation was 97% while providing oxygen at 3 L/min. IL-6 (198.66 pg/mL) was almost 10 times the normal range (≤5.9 pg/mL), which indicated the initiation of a cytokine storm on day twelve (Figure 1 ). The EBP, including a double plasma molecular adsorption system (BS330 and HA330II, Jafron, China) and plasma exchange (2000 mL each), was applied to remove the cytokines on day 13. The BS330 and HA330II were installed in series after the plasma separator (EC-4W, Asahi) with a blood flow velocity of 80–100 mL/min and a separating speed of 20–25 mL/min; the duration of the treatments was six hours. The plasma exchange was then conducted. Intravenous methylprednisolone (40 mg daily) was used to suppress the inflammatory reaction. The patient was mostly stable until the chest distress exacerbated, and blood in phlegm developed on day 14. He then progressed to type I respiratory failure (partial pressure of oxygen 51 mmHg, partial pressure of carbon dioxide 32 mmHg) with 89% oxygen saturation while the oxygen flow was 3 L/min. High-flow oxygen (40 L/min) was initiated to keep oxygen saturation values between 96–99%. Hydroxychloroquine was discontinued due to a prolonged QT interval. The EBP therapy continued on days 14 and 15.
Figure 1.
The changes of cytokines and FDPs and the medications applied. The left vertical axis represents the levels of interleukin 2 (IL-2, blue dot) and fibrinogen degradation products (FDPs, purple dot). The right vertical axis represents the levels of interleukin 6 (IL-6, red dot) and interferon γ (INF γ, green dot). The horizontal axis shows the illness days. The gray vertical bar shows the artificial liver therapy. The horizontal bars with different colors represent the medications, and the lengths represent the corresponding duration. Lh Qw denotes the Lianhua Qingwen capsule.
The patient was transferred into ICU on day 15. Given the acute inflammatory reaction, methylprednisolone was increased to 60 mg twice daily, and piperacillin–tazobactam (4.5 g administered intravenously every eight hours) was initiated to treat hospital-acquired pneumonia. Acetylcysteine was used to dilute the phlegm. Human serum albumin and other supportive care were also administered. The patient’s clinical condition improved on day 16 and was stable thereafter; his hepatic function returned to normal as well. His body temperature returned to normal on day 17. The IgM of anti- SARS-CoV-2 was identified (77.11 AU/mL, normal value <10 AU/mL) on the same day. Methylprednisolone was gradually reduced and discontinued on day 23. The lesions on chest CT were confined on day 17, further alleviated on day 21, and almost disappeared on day 33 (Supplemental Figure 1). A low flow rate of oxygen (2 L/min) was delivered instead of high-flow oxygen, on day 26, then discontinued on day 36. He was asymptomatic at rest and had no shortness of breath while doing activity training. His renal function was unaffected, and immunoglobulin levels, including IgG, IgM, IgA, and IgE, were normal throughout the clinical course. Complement C3 level was staying below the normal range (0.9–1.8 g/L) during the hospital duration (Supplemental Table 1). C4 level (<0.06 g/L, normal range: 0.1–0.4 g/L) was reduced at day 16 and was back to normal (0.15 g/L) on day 31. The nucleic acid testing of SARS-CoV-2 was negative at four different times. He was discharged on day 38.
Discussion
The management of COVID-19 in critical cases is still challenging. Respiratory and circulation support, such as mechanical ventilation and extracorporeal membrane oxygenation (ECMO), were almost the last defense for severe COVID-19 (Bartlett et al., 2020). Although specific methods to intervene in the progression of critical cases are unknown, the effects of EBP in the treatment of COVID-19 associated cytokine storm have not been emphasized. The outcome of the present case of COVID-19 with ARDS is promising. Pulmonary fibrosis was not observed to date.
EBP was suggested to interrupt the inflammation cascade and stop the progression of the cytokine storm. There were evident peak levels of cytokines after the initiation of EBP on day 13. HA330 improved oxygenation and lung mechanics by removing circulating and alveolar cytokine levels (Honore et al., 2019b); BS330 adsorbed bilirubin to attenuate liver injury (Su et al., 2016). The EBP that combined the double plasma molecular adsorption system and plasma exchange can directly reduce the cytokines. Although methylprednisolone was also administered synchronously, it has been identified that the significant time point of IL-6 reduction was the seventh day rather than the first three days in ARDS (Metwally et al., 2019). Also, there was a very short time-window to manipulate the acute inflammatory state. The patient became unstable all of a sudden without any changes in clinical symptoms or subjective discomfort until day 14. Fortunately, we noticed the elevation of cytokine levels on day 12. Therefore, the proper time for intervention, based on the levels of cytokines, needs further validation.
Similar features to this case were found in the published literature (Guan et al., 2020, Wang et al., 2020), for instance, low level of lymphocytes, high level of cytokines, and d-dimer. Of interest, we found that the changes in fibrinogen degradation products (FDPs) (Figure 1) were correlated with cytokines. It returned to normal range even earlier than the cytokines and d-dimer. Besides, an increase in the d-dimer over time was observed in non-survivors with more stable levels than in survivors (Wang et al., 2020). Taken together, employing FDPs as a sensitive marker of injury and prognosis of COVID-19 is warranted.
Although the present patient has completely recovered from severe COVID-19, other factors should also be considered:
-
(a)
There were no chronic complications, and the patient was of a relatively younger age.
-
(b)
There was no development of other organ failures.
-
(c)
The existence of antibodies to SARS-CoV-2.
Conclusion
The prognosis of critical cases of COVID-19 might be improved if a timely intervention of EBP was performed.
Conflicts of interest statement
The authors declare that they have no relevant financial interests.
Funding source
This work was supported by the Shandong UniversitySpecial Project for COVID-19 (2020XGA01).
Ethical approval
This study was approved by Qilu Hospital, Cheeloo College of Medicine, Shandong University.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2020.05.065.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Bartlett R.H., Ogino M.T., Brodie D., McMullan D.M., Lorusso R., MacLaren G. Initial ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. ASAIO J. 2020;66(5):472–474. doi: 10.1097/MAT.0000000000001173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y., Liang W.J., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honore P.M., Hoste E., Molnar Z., Jacobs R., Joannes-Boyau O., Malbrain M.L.N.G. Cytokine removal in human septic shock: where are we and where are we going? Ann Intensive Care. 2019;9(1):56. doi: 10.1186/s13613-019-0530-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honore P.M., De Bels D., Barreto Gutierrez L., Spapen H.D. Hemoadsorption therapy in the critically ill: solid base but clinical haze. Ann Intensive Care. 2019;9(1):22. doi: 10.1186/s13613-019-0491-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L.L., Zhao J.P., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metwally A.A., Fathy W.M., El-Feky E.M., Saleh M.E.S. Effect of methylprednisolone on inflammatory markers and patients’ outcomes in acute respiratory distress syndrome. Menoufia Med J. 2019;31:1193–1199. [Google Scholar]
- Su R., Rao Y., Shen X., Zhu J.N., Ji A.Q., Jin G.R. Preparation and adsorption properties of novel porous microspheres with different concentrations of bilirubin. Blood Purif. 2016;42(2):104–110. doi: 10.1159/000445933. [DOI] [PubMed] [Google Scholar]
- Wang D.W., Hu B., Hu C., Zhu F.F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C., Chen X., Cai Y., Xia J.A., Zhou X., Xu S. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.