Introduction
New York City (NYC) evolved rapidly into the epicenter of the coronavirus disease 2019 (COVID-19) pandemic in the United States. Throughout the month of March, cases of COVID-19 infection in NYC increased rapidly with 41,771 positive patients and 1,096 mortalities as of March 31.1 Infection among health care workers strained hospital systems by limiting the number providers available for patient care as institutions become overwhelmed with COVID-19 patients. To preserve personal protective equipment (PPE), expand hospital bed capacity, and protect the safety of staff and patients, the Centers for Disease Control and Prevention and American College of Surgeons released guidelines recommending that all nonurgent surgical procedures be halted.2 , 3
A recent report described restructuring of a general surgery program in a prepandemic setting.4 Within the setting of rapidly evolving hospital policies and the COVID-19 case load, the General Surgery program at Mount Sinai Hospital in NYC underwent many emergent restructurings of the clinical services while trying to maintain fundamental educational experiences. Clinical restructuring occurred in 2 phases: (1) the surge—when COVID-19 cases were beginning to increase in the system; and (2) the pandemic—when the hospital system quickly became saturated and overwhelmed, and preservation of semi-normal hospital operations quickly changed. In this report, we describe the restructuring of our general surgery program across these phases as the objectives of staffing shifted from minimizing exposure and protection of staff to deployment for help covering COVID-19 units as the system resources became overwhelmed with cases.
Clinical staffing
Phase 1: The surge and general surgery staffing
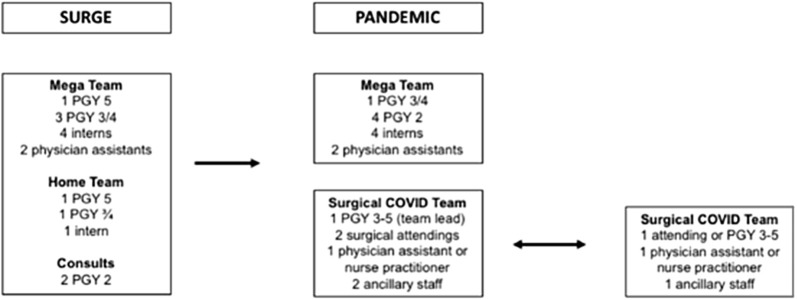
The prior team structure at Mount Sinai main campus consisted of 4 general surgery teams with 1 chief resident (PGY-5s), 2 senior residents (PGY-3 or -4s), and 4 interns (PGY-1s), in addition to a consult resident (PGY-2; Fig 1 ). As cases of COVID-19 increased in NYC, the Mount Sinai health system began to prepare for an inordinate incoming surge of patients due to the location and access points of the Mount Sinai Health Systems in NYC. As of March 18, 2020, all elective cases were cancelled. Attending surgeons worked with the house staff to cover all emergent cases from the inpatient services and the emergency department.
Fig 1.
Team structures of general surgery residents at Mount Sinai Hospital before and during the coronavirus disease surge and pandemic.
In the setting of a markedly decreased volume of elective cases and an anticipated lower inpatient census, we elected to reorganize the surgical teams to preserve and use resources in a thoughtful manner. A single “mega-team” was rolled out on March 23. Before this, all efforts were made to discharge patients from the hospital as the elective cases ceased and the volume of COVID-19 increased within the hospital.
Two inpatient teams were made that each consisted of 1 chief resident, 3 senior residents, and 4 interns. In addition, there were 2 daytime residents (PGY-2s) who handled all the consults initially. The 2 teams were on service on a 48-hour-on, 48-hour-off schedule. There were also 2 physician assistants (PAs) per 12-hour shift. The on-call patient team was responsible for all inpatient duties, including morning rounds, admissions and discharges, new consults, and the staffing of the operating room. To limit exposure to COVID-19, nonessential team members were sent home after morning rounds were completed. One of the 3 senior residents served as the in-house consult resident and stayed for a 24-hour shift daily. The consult resident evaluated all new consults; however, all efforts were made to limit exposure to off-service patients as more consults were increasingly involving COVID-19 patients. As such, only essential consults were seen.
An inpatient, surgical back-up team was on standby daily to be activated for morning rounds when the inpatient census was ≥15 patients. The remaining residents were on standby to allow for cross-coverage and creation of special teams to assist directly in treatment of COVID-19 patients. Initially, this consisted of PGY1s rotating in the intensive care unit (ICU) in 2- to 12-hour day blocks, followed by 2 days off to assist the critical care teams in patient management (documentation, consults, and organizing transfers) but with no direct patient care.
Phase 2: Pandemic team structure
Approximately 1.5 weeks after the surge model was implemented, the crisis began to further develop in severity and the hospital system became saturated and soon overwhelmed with COVID-19 patients. Bed shortages necessitated having both COVID-19 positive and negative patients on the same floor. Furthermore, most of the senior residents and chief residents were deployed as leaders of surgical COVID-19 teams to help meet the needs of the health system. As such, the inpatient surgical “mega-team” was then changed to be composed of 1 senior resident acting as chief resident, 4 PGY-2s, 4 interns, and 2 PAs. The PGY-2 residents took turns every other day on 24-hour call for consults. After rounds, 1 to 2 interns stayed inhouse to work with the PA on documentation and discharges, and the rest of the team, if possible, went home.
Surgical COVID-19 teams were assigned based on need within the health system, which included 7 other hospitals ranging from a capacity of 200 to 1,200 beds. The composition of the surgical COVID-19 teams was as follows: 1 chief/senior resident (team lead), 2 surgical attendings, 1 PA or nurse practitioner (NP), and 2 ancillary staff (a medical or administrative assistant for documentation and other lesser acuity medical needs). But because case load and hospital burden varied by location and as some team members got sick themselves or needed time to rest to ensure wellness, this structure became fluid and varied as the needs arose. Nevertheless, the team always included at least one physician per team. The team lead was responsible for: (1) organizing communication regarding deployment of the team to needed locations and functions, (2) delegating responsibilities to team members at the deployment site, and (3) distribution of designated team PPE. The most common sites of deployment were to ICUs and emergency departments. Rotations were either 8- or 1- hour shifts for 3 days followed by 3 days off.
Residents were pulled off of all off-service rotations (eg, anesthesia, plastic surgery) except for vascular surgery to increase the available workforce. Additionally, residents who were on research were recruited back in to help with staffing, and those with assigned vacation were recruited and offered compensation for working. Throughout this restructuring, every attempt was made to comply with the duty-hour regulations as mandated by the Accreditation Council for Graduate Medical Education.
Outpatient Clinics
Outpatient clinics were continued but were staffed only by attending staff surgeons. As the volume of COVID-19 cases increased, outpatient clinics were closed and staff in those clinics were redeployed elsewhere.
PPE
We carefully kept inventory of available PPE for our surgical and COVID-19 teams. As described earlier, the surgical COVID-19 team lead was responsible for ensuring that the team had appropriate PPE at the deployment site. PPE was obtained through the institutional Graduate Medical Education Office, Department of Surgery as well as from specific floors and units at deployment sites.
Communication
To facilitate communication during this time of evolving changes, 2 separate encrypted messaging conversations were used. One was for the inpatient team to communicate regarding daily staffing and sign out of patients between teams.
A second conversation encompassed the entire General Surgery residency program, NPs, and PAs and was used for coordination of major events and dissemination of general information.
Education and simulation
All residents and attendings attended mandatory simulation sessions on both proper donning and doffing of PPE and on the basics of critical care and airway management of COVID-19 patients in the ICU setting and proper management in the setting of cardiac arrest.
We continued our weekly Friday basic science didactic sessions; however, the format was modified from small groups to an Internet meeting format, and the focus was changed to topics dealing with intensive care and COVID-19. Furthermore, we converted our weekly departmental morbidity and mortality and grand rounds conferences into an Internet meeting, with presentation of various COVID-related updates and studies.
Testing for COVID-19 infection
The initial policy of our health system for management of symptomatic employees was to self-isolate at home for minimum of 7 days and to return to work after being afebrile for 72 hours. Our institution eventually began to test employees in order to preserve the workforce. During this period, we had several house staff develop symptoms with seroconversion for COVID-19. To date, they have all recovered safely and returned to work. Antibody testing was performed on all employees deployed on the COVID-19 teams; however, we did not use the antibody test result as a screening tool to determine who came back to work because of the variability in the titres and immune response.
Wellness
Given concerns regarding infection and the uncertainty surrounding the schedule, we implemented a weekly wellness Internet conference check-in to facilitate sharing of concerns and experiences. Furthermore, our institution made counseling services available and implemented regular system-wide house staff town halls. Daily mindfulness sessions were available for all employees. Finally, a $300-dollar additional stipend was added onto the salary of all house staff.
In conclusion, during this rapidly evolving situation, ensuring the safety of residents while providing critical staffing remained the ongoing challenge as the crisis evolved from a surge to pandemic. Our experiences during this period saw the cessation of nearly all normal operating procedures. In the setting of this rapidly changing environment, we had to adapt our usual spectrum of hospital operations to the occasion. Our experience demonstrated the importance of having a plan, but furthermore, the importance of having the flexibility to adapt the plan in order to maximize resources to help the system as the situation worsened while simultaneously ensuring the safety and wellbeing of the workforce. We hope that our experiences can help other programs prepare as the volume of COVID-19 patients increases in their hospitals or as a new surge occurs in the fall.
Funding/Support
None
Conflict of interest/Disclosure
The authors have no relevant disclosures.
References
- 1.City of New York Mayor de Blasio to create hospital at Billie Jean King Tennis Center to relieve need at Elmhurst Hospital. https://www1.nyc.gov/office-of-the-mayor/news/214-20/mayor-de-blasio-create-hospital-billie-jean-king-tennis-center-relieve-need-elmhurst
- 2.CDC COVID-19: Strategies for optimizing the supply of PPE. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html
- 3.COVID-19: Guidance for triage of non-emergent surgical procedures. https://www.facs.org/covid-19/clinical-guidance/triage
- 4.Nassar AH, Zern NK, McIntyre LK, et al. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: The University of Washington Experience [Epub ahead of print]. JAMA Surg. 10.1001/jamasurg.2020.1219. Accessed April 12, 2020. [DOI] [PubMed]