To the Editor:
The coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China, has caused considerable infection in health-care workers (HCWs). More than 3,000 cases in 422 involved medical facilities have been reported by the Chinese Center for Disease Control and Prevention (China CDC) as of February 22, 2020; 64% occurred in Wuhan.1 However, the incidence and patterns of infection in medical staff have not yet been described.
Patients and Methods
COVID-19 infection rates, models of infection, and clinical characteristics and outcomes among HCWs were examined in Renmin Hospital of Wuhan University, a general hospital with 5,200 beds, 118 clinical departments, 33 administrative divisions, and 6,507 staff members. This study enrolled 166 medical staff members diagnosed with COVID-19 from January 10, 2020, to February 11, 2020. The data cutoff date was February 19, 2020. Nucleic acid testing for COVID-19 is mandatory for all symptomatic staff members, suspected case subjects, and close contacts of COVID-19 patients, and optional for any other staff members. Diagnostic criteria for COVID-19 were based on the Diagnosis and Treatment Scheme of Novel Coronavirus-Infected Pneumonia, Version 6, by the China CDC.2 This retrospective study was approved by the institutional ethics board of Renmin Hospital of Wuhan University (No. 2020020).
Clinical characteristics and distribution of the study subjects were recorded. Red area was defined as where those diagnosed or suspected cases were isolated or treated. The study subjects were divided into three groups: a mild group, with asymptomatic or mild symptoms but no radiographic evidence of pneumonia; a moderate group, with moderate symptoms such as a fever or respiratory symptoms, or with radiographic evidence of pneumonia; and a severe group, with respiratory distress (respiratory rate ≥ 30 times per minute), hypoxemia (blood oxygen saturation ≤ 93% at rest), or Pao 2/Fio 2 ≤ 300 mm Hg. All patients were managed with standard treatment protocols of antivirotics and antiinflammatory drugs,3, 4, 5 symptomatic and respiratory support, and assessment of demographic, clinical, radiologic, and laboratory characteristics. The total CT score was the sum of lung involvement (5 lobes, score 1-5 for each lobe, range, 0 none, 25 maximum). The CT score was recorded according to previously reported methods.6 , 7
Results
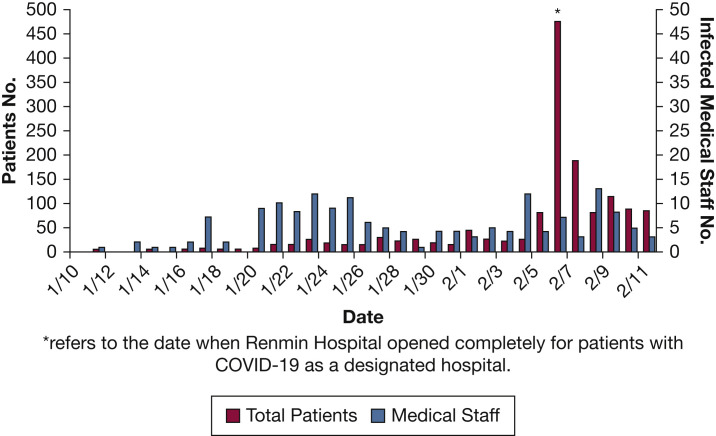
The incidence curve of COVID-19 patients and infected HCWs is shown in Figure 1 . Among 6,507 HCWs (median age, 33.0 years [interquartile range, 28.0-42.0 years]; 1,920 male subjects, 4,587 female subjects), the infection rate was 2.55% (n = 166; median age, 34.0 years [interquartile range, 21.0-57.0 years]; 50 male subjects, 116 female subjects). Staff members with both clinical (140 cases [46 in the red area, 94 outside the red area]; 84.3%) and nonclinical (26 cases; 15.7%) cases were involved. No epidemic chain of transmission of COVID-19 originated from one super spreader.
Figure 1.
The number of patients with COVID-19 and number of infected hospital staff members in Renmin Hospital. ∗Date when Renmin Hospital opened completely for patients with COVID-19 as a designated hospital. COVID-19 = coronavirus disease 2019.
Table 1 includes the clinical characteristics for patients. Most cases were classified into the mild (9.64%) or moderate (80.12%) group. As of the study cutoff date, 69 patients (including eight mild, 54 moderate, and seven severe cases) were discharged (median length of stay, 16.7 days). The 97 remaining hospitalized cases recovered significantly. As of March 25, 2020, all moderate or mild cases and two severe cases had been discharged. The other eight with severe disease were discharged on April 17, 2020, and no one died (data not shown).
Table 1.
Baseline Characteristics of Hospital Staff Infected With COVID-19
| Variable | Total (N = 166) | Mild Cases (n = 16) | Moderate Cases (n = 133) | Severe Cases (n = 17) | P |
|---|---|---|---|---|---|
| Characteristic | |||||
| Age, median (range), y | 34 (21-57) | 29 (24-42) | 35 (21-58) | 42 (27-57) | .009 |
| Sex | .001 | ||||
| Male | 50 (30.12) | 1 (6.25) | 38 (28.57) | 11 (64.71) | |
| Female | 116 (69.88) | 15 (93.75) | 95 (71.43) | 6 (35.29) | |
| Comorbidities | 19 (11.45) | 1 (2.17) | 7 (6.80) | 11 (64.71) | < .001 |
| Signs and symptoms | |||||
| Fever | 103 (62.05) | 0 | 86 (64.66) | 17 (100) | < .001 |
| Cough | 81 (48.80) | 3 (18.75) | 63 (47.37) | 15 (88.24) | < .001 |
| Fatigue | 51 (30.72) | 2 (12.50) | 41 (30.83) | 8 (47.06) | .099 |
| Dyspnea | 33 (19.88) | 0 | 19 (14.29) | 14 (82.35) | < .001 |
| Sore throat | 31 (18.67) | 5 (31.25) | 25 (18.80) | 1 (5.88) | .190 |
| Myalgia | 29 (17.47) | 1 (6.25) | 16 (12.03) | 12 (70.50) | < .001 |
| Headache | 18 (10.84) | 1 (6.25) | 14 (10.53) | 3 (17.65) | .555 |
| Nausea | 11 (6.63) | 0 | 9 (6.77) | 2 (11.76) | .351 |
| Diarrhea | 9 (5.42) | 0 | 7 (5.26) | 2 (11.76) | .406 |
| Laboratory | |||||
| Leukocyte < 3.5 × 109/L | 27 (16.27) | 1 (6.25) | 22 (16.54) | 4 (23.53) | .691 |
| Neutrophils < 1.8 × 109/L | 30 (18.07) | 3 (18.75) | 26 (19.55) | 1 (5.88) | .563 |
| Lymphocyte < 1.1 × 109/L | 48 (28.92) | 0 | 37 (27.82) | 11 (64.71) | < .001 |
| Monocyte < 0.1 × 109/L | 2 (1.20) | 0 | 2 (1.50) | 0 | .914 |
| Eosinophils < 0.02 × 109/L | 63 (37.95) | 1 (6.25) | 49 (36.84) | 13 (76.47) | < .001 |
| CRP > 10 mg/L | 34 (20.48) | 0 | 20 (15.04) | 14 (82.35) | < .001 |
| SAA ≥ 10 mg/L | 89 (53.61) | 4 (25.00) | 68 (51.13) | 17 (100) | < .001 |
| Abnormalities on CT imaging | |||||
| Ground-glass opacity | 133 (88.67) | 0 | 118 (88.72) | 15 (88.24) | .998 |
| Patchy shadowing | 119 (79.33) | 0 | 102 (76.69) | 17 (100) | .024 |
| Interstitial abnormalities | 67 (44.67) | 0 | 52 (39.10) | 15 (88.24) | < .001 |
| Crazy-paving pattern | 48 (32.00) | 0 | 32 (24.06) | 16 (94.12) | < .001 |
| Consolidation | 51 (34.00) | 0 | 37 (27.82) | 14 (82.35) | < .001 |
| Linear densities | 71 (47.33) | 0 | 56 (42.11) | 15 (88.24) | < .001 |
| CT score, mean ± SD (range) | 3.0 ± 2.4 (1-14) | 0 | 2.3 ± 1.2 (1-7) | 8.3 ± 2.9 (5-14) | < .001 |
| Outcomes | |||||
| Hospitalization | 97 (58.43) | 8 (50.00) | 79 (59.40) | 10 (58.82) | .771 |
| Discharge | 69 (41.57) | 8 (50.00) | 54 (40.60) | 7 (41.18) | ... |
| Length of stay, mean ± SD, d | 16.7 ± 5.7 | 12.2 ± 4.6 | 18.0 ± 4.7 | 23.8 ± 5.0 | < 0.001 |
Data are presented as No. (%) unless otherwise indicated. CRP = C-reactive protein; SAA = serum amyloid A.
Representative characteristics in this population included a higher proportion of young, prime-aged subjects, a majority of mild or moderate cases, feasibility of treatment within the “golden first week” of disease, and lower mortality compared with the general population.
Discussion
We describe here the COVID-19 infection pattern in medical staff in Wuhan for the first time, which featured various types of medical personnel involved even outside the red area. Here, red area was defined as where those diagnosed or suspected cases were isolated or treated.
On the incidence curve, two peaks were observed (Fig 1), which coincided with the COVID-19 epidemic peaks in China.8 We attribute the first peak (January 20-26, 2020), at least partly, to the lack of knowledge regarding the disease, enforcement of procedures, and specialized COVID-19 wards, as well as inadequate personal protective equipment (PPE), especially for those outside the red area at the early stages of the COVID-19 outbreak. On January 20, 2020, the China CDC annouced that COVID-19 is categorized as B type infectious disease but with A type infectious disease management.9 Prior to the announcement, workers in the red area were equipped with level 1 protection (disposable work cap, medical surgical mask, work clothes, disposable impermeable isolation clothing, and disposable latex gloves), whereas those outside the red area had no protection when dealing with patients on the front-line without effective COVID-19 screening. During this period, some nonclinical staff members were infected due to cross-infection in the hospital.
We attribute the second peak (February 4-8, 2020) to close and frequent contact with COVID-19 patients with insufficient supply of PPE. When level 3 protection (disposable working cap, full-mask respirator or other respirator with positive air pressure, medical N95 mask, protective clothing, disposable latex gloves, and disposable shoe covers) was enforced in the red area, the infection was significantly reduced. To reduce the impact of medical runs (all medical resources concentrated on COVID-19 patients, which leads to lack of medical resources for non-COVID-19 patients) on non-COVID-19 patients, all clinical staff members outside the red area worked on the front-line. Due to the insufficient PPE supply, most of them were equipped with level 1 protection under the premise of COVID-19 screening. However, COVID-19 screening was not yet thorough enough, which resulted in noticeable infection among HCWs outside the red area. Similarly, with incomplete level 1 protection, nonclinical staff members provided logistics and administrative support for the main campus designated for non-COVID-19 patients, the east campus appointed for severe COVID-19 cases, the Wuchang mobile cabin hospital, and several medical assistance teams from other provinces, and a few were infected.
After mid-February, PPE supply was compensated by government allocation and social donations, and protection of clinical workers outside the red area increased to level 2 (disposable working cap, goggles or protective screen, N95 mask, protective clothing and disposable latex gloves, and disposable shoe covers). Meanwhile, strict safety protocols, disinfection routines, and training programs were implemented and enforced. Few sporadic infections occurred thereafter.
We draw some experiences and lessons from prevention of COVID-19 infection in the hospital. In each work area, regardless of whether it was in the red area, we set up three zones (infected, buffering, and cleaning zones) and two channels for staff and patients, respectively. Common outpatient clinics receive patients all by online time-segment appointment. We screened patients by using a “twice screening, twice buffering” strategy. First, in the outpatient department, patients with fever were shifted into fever clinics. Second, in the emergency ward, COVID-19 patients and carriers were screened by using CT imaging and blood testing and allocated to fever clinics. Prior to hospitalization, patients were housed temporarily in a specialized buffering ward for 3 days receiving symptomatic and supportive treatment. Patients were then transferred to the buffering zone of an ordinary ward for another 3 days and received professional treatment.
This study has several limitations. In calculating infection rate, we used the total number of HCWs as the denominator, although not everyone underwent testing. Here we assumed that the staff members not tested were not infected under the principle of mandatory testing for symptomatic or suspected staff (or close contacts) and freewill testing for other staff.
However, for potential missed cases with asymptomatic or atypical initial symptoms, or false-negative results of nucleic acid testing, we probably underestimated the infection rate. Instead, we may have overestimated the infection rate as not all HCWs have the same exposure risk in different health-care settings.
In addition, the data from the medical staff infected with COVID-19 may vary dramatically in different hospitals with diverse missions in Wuhan. Even so, our study will be helpful in preventing COVID-19 in HCWs from other hospitals currently dealing with this pandemic.
Acknowledgments
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript
Footnotes
Drs Q. Song and Bu contributed equally to this work as co-corresponding authors.
FINANCIAL/NONFINANCIAL DISCLOSURES: None declared.
FUNDING/SUPPORT: This work was supported in part, by the National Natural Science Foundation of China (81871419 to L. B., 81670123 to Q. S.), and Seed project in Sino foreign joint research platform of Wuhan University (2309-413100006 to L. B.). This was not an industry supported study.
References
- 1.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [in Chinese] [DOI] [PubMed] [Google Scholar]
- 2.National Health Commission of the PRC Diagnosis and Treatment Scheme of Novel Coronavirus–Infected Pneumonia, Version 6. http://www.nhc.gov.cn/xcs/zhengcwj/202003/4856d5b0458141fa9f376853224d41d7.shtml Accessed July 1, 2020.
- 3.Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected by SARS-CoV-2 in Wuhan, China [published online ahead of print February 19, 2020]. Allergy. https://doi.org/10.1111/all.14238. [DOI] [PubMed]
- 4.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu F., Zhao S., Yu B., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [published correction appears in Nature. 2020;580(7803):E7] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan F., Ye T., Sun P., et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020;295(3):715. doi: 10.1148/radiol.2020200370. fro. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang Y.C., Yu C.J., Chang S.C., et al. Pulmonary sequelae in convalescent patients after severe acute respiratory syndrome: evaluation with thin-section CT. Radiology. 2005;236(3):1067–1075. doi: 10.1148/radiol.2363040958. [DOI] [PubMed] [Google Scholar]
- 8.National Health Commission of the PRC Coronavirus disease 2019 (COVID-19) situation reports. http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml Accessed July 1, 2020.
- 9.National Health Commission of the PRC Announcement of the National Health Commission of the People's Republic of China. http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml Accessed July 1, 2020.