Introduction
Emergency Radiology as an organized subspecialty is relatively new. While the surgery community felt the need to organize around the concept of trauma treatment in the early 20th century, it was not until 1988 that the radiology community acted on a similar need to form the American Society of Emergency Radiology.1, 2, 3, 4, 5 In the ensuing decades, focused attention to the needs of the emergency department, emergency providers and trauma surgeons has improved the efficiency and effectiveness of the management of the increasing number of patients seeking service in the emergency department.
Today, the emergency radiologist must not only be familiar with the breadth of imaging findings that may be seen in the Emergency Department (ED) but should also manage imaging in the ED.6 Particular facets of imaging that differ from other radiology settings include maintaining the relationship with the Emergency Medicine physicians, staffing considerations, designing ED-specific imaging protocols, active management of acquisition and interpretation of a wide range of imaging studies, managing outside imaging, and planning and practice for mass casualty incidents (MCI).
One of the challenges in any discussion of emergency radiology is clearly defining what is meant in that context. One definition may apply strictly to imaging performed in the emergency department. Others use “emergency radiology” to refer to all after-hours imaging, performed after the regularly scheduled radiologists have left for the day. Another definition may include urgent (ie, not routine) imaging performed after-hours.
This article will address only imaging performed in the ED and give examples from a level 1 trauma center with a dedicated emergency radiology section. Many of these practices can be adapted to any practice pattern or hospital setting. It is the goal of this article to generate ideas for improvement in the readers’ own environment.
Emergency Radiologist as a Bridge to Emergency Providers
The needs of the emergency department are unique. In the same way that chest radiologists are best suited to address the needs of pulmonologists, and neurologists and neurosurgeons prefer to consult with neuroradiologists, a subspecialized radiologist who focuses on the needs of the emergency department provides added value.7 After diagnostic accuracy, the primary need for the ED provider is speed. Emergency radiology must be done in a real-time mode, as patient length of stay (LOS) is a critical metric for the ED.8 Without a dedicated emergency radiologist, ED exams may languish in the general or subspecialist's queue or result in irregular interruptions to their workflow. By centralizing the acute care imaging, both ED and radiologist efficiency is improved. Finally, emergency providers often value brevity over comprehensiveness in their reports, in contrast to much of the referral base of a radiology department, so the additional time taken to craft a well-researched report may in fact be counter to the needs of the ED provider.
Emergency radiology can be provided on site or remotely. As many health care enterprises grow and have multiple sites of care, teleradiology can effectively be used to provide real-time image interpretation over a broad geographic area. Contract teleradiology services have become an integral part of many practices to provide emergency coverage but may have limitations. The personal relationships that smooth interactions between providers are harder to maintain when there is a widely varying teleradiologist pool. Additionally, most contract teleradiology practices do not have Electronic Medical Record (EMR) or full Picture Archiving and Communications System (PACS) integration, so historical information may be available only on request.
In our level 1 trauma center, emergency radiologists are sited in the emergency department. Our practice has been to provide in-person “wet reads” for all trauma series radiographs (portable chest and pelvis) in the resuscitation suite as soon as the exams are available in PACS. Newer portable radiography units have embedded low-resolution monitors, so for full trauma activation patients, we now stand behind the techs and provide a “super wet-read,” as the images are being acquired, even before they are QA'ed or sent to PACS (Fig. 1 ).
Figure 1.
Current generation portable x-ray units have an integrated low resolution screen interfaced with wireless DR cassettes, allowing immediate preliminary interpretation even between exposures.
Staffing
While trauma centers may benefit from fellowship-trained emergency radiologists, most practices will need to create an emergency radiology service from a larger pool. Whether staffed by general radiologists or subspecialists broadening their area of practice, a dedicated focus on trauma and other emergencies is beneficial, both in terms of clinical exposure and continuing education. A recent study has shown a substantial discordance between community radiologists and trauma center emergency radiologists when interpreting CT scans of transfer patients.7 Another study examining radiology malpractice claims found that a disproportionate number of claims arose from emergency department examinations.9
The location of the emergency radiologist can also affect the impact of the service. In our practice, the emergency radiology reading room is centrally located in the Emergency Department ( Fig. 2). Our radiologists are immediately physically available to the providers, techs and even patients. We are able to monitor exams at the CT console to ensure completeness and eliminate recalling patients for additional exams (such as delayed imaging), avoiding routine overscanning. This kind of space may not be available in most emergency departments without extensive remodeling, but even smaller hospitals can fit a reading station into a quiet part of the ED10 (Fig. 3 ). The physical location in the ED provides the opportunity to develop personal relationships with the ED providers during quiet moments, recreating the more social environment of medical practice in years gone by.
Figure 2.
Radiology is located in the center of the Harborview Medical Center trauma ED. Treatment rooms (red) and clinician work areas (blue) surround the radiology technical (purple) and interpretive (yellow) areas. Ambulance entrance is to the left, and nontrauma (medicine) ED rooms extend beyond the top of the image.
Figure 3.
Radiologist sited in a community hospital Emergency Department (Image courtesy of Richard Levey, MD).
The precise scope of the emergency radiologist may vary from practice to practice but should be internally consistent. Some practices may segregate neuro exams to neuroradiology, while others may defer nonacute ED imaging (metastatic workups, eg) to the relevant subspecialist services. In our current practice, coronary Computed Tomography Angiogram (CTA) for acute chest pain is covered by the emergency radiology section while most of the head and neck imaging is handled by the neuroradiologists. To be credible, if a group commits to provide a service, it is important that all members of the section be able to provide the service on a predictable basis. The Emergency Department cannot integrate an exam into their algorithms if they have to see who is on service before ordering the test.11
Given the dynamic and unpredictable nature of emergency imaging, all (or at least most) of the personnel involved need to be flexible, and willing and able to modify their focus and attention to the tasks at hand, and deal with the sometimes chaotic, noisy, and stressful environment that can result.
CT technologists managing a critically ill or injured patient, not only have to perform a high quality study on a patient who might be unable to cooperate, or who needs frequent checks or updates by the clinical team, but also need to work around a potentially large group of clinicians loudly discussing the patient's care and next steps, and anxiously looking over the tech's shoulder. They need to be able to firmly but politely manage all these people, to allow rapid imaging to take place with the appropriate focus and attention, in order to obtain a high-quality diagnostic exam.
X-ray technologists may also need to image patients in distress, with multiple or severe injuries, including patients with open thoracotomies or extensive extremity injuries including amputations. Experience and patient status help to determine the extent to which optimal positioning and imaging is attempted, vs a “good enough” exam to allow expedient management of the patient given their current status and situation. More optimal imaging may need to be delayed until the patient is more stable and/or additional resources are available.
Staff who are trained and experienced in both x-ray and CT imaging are extremely valuable and can adjust where they work based on the immediate needs of the ED, improving throughput. For example, if CT imaging is backed up while x-ray imaging is proceeding normally, a cross-trained x-ray tech can assist with CT imaging, either as extra personnel to assist in expediting imaging of patients, or to provide coverage during breaks taken by the other CT techs.
Similarly, staff (schedulers, techs, transporters, nurses, etc.) who can rapidly switch between tasks and patients without getting flustered, confused, or upset, allow optimized care in dynamic situations. Examples include re-triaging of patients and having to stop loading a patient onto the CT scanner, so that a more critical patient can be imaged instead.
Imaging Management
As effective ED imaging requires balancing between rapid access, diagnostic specificity, time to arrive at a completed study (including interpretation) and time to get the diagnostic information back to the ordering ED physician,12 cooperation of all of the involved stakeholders is required to develop appropriate protocols. Three ED imaging scenarios: whole body CT (WBCT) for polytrauma patients, stroke imaging and ED MRI can serve as examples of how to improve imaging availability and efficiency for the ED. WBCT protocol development requires attention to scanning and reconstruction management. Acute stroke imaging exemplifies how to improve the efficiency of the ED workup. Integration of MR imaging into ED routines requires specialized imaging protocols to be practical.
Whole Body CT
Physical examination to determine what portions of a trauma patient to image can be challenging. Several studies13 , 14 have demonstrated that nearly one-fifth of patients with normal abdominal exams were found to have an abdominal injury on CT.
Even if the correct body portions are imaged, use of a combination of individual CT scans, such as cervical spine CT followed by Chest CT, often resulted in overlap of regions scanned, and delays in patient imaging, as each study was set up and the patient repositioned. These delays matter, as in trauma activation patients, delays have been reported to increase the probability of death by approximately 1% for every additional 3 minutes spent in the ED.15
Trying to piece together imaging for a polytrauma patient could result in delays, as different combinations of CTs are considered and ordered by the clinical teams, which may not be compatible with each other. For example, the contrast amount, timing, technical factors and positioning of the arms for a dedicated neck CTA would usually not be compatible with the requirements for a chest CTA or abdominal CT.
These factors led to the development of whole-body CT, also known as pan-scan protocols for patients with polytrauma, which image the entire torso and cervical spine, and include or are performed along with a noncontrast head CT. Use of pan-scans have been reported to be an independent predictor for survival16 and have been widely implemented over the last decade.
A variety of pan-scan protocols have been implemented by different institutions which have evolved over time with experience and improvements in scanner technology.17, 18, 19, 20 The current version of our protocol consists of a noncontrast head CT, followed by arterial phase imaging from the skull vertex to approximately 5 cm above the iliac crest, followed by portal venous phase imaging of the abdomen and pelvis. ( Fig. 4). The arms are placed above the abdomen on a bolster to minimize beam hardening artifact. Delayed images are obtained if indicated, following review of the scan while the patient is still in the scanner. If a pelvic ring injury is identified and patient has 3+ or greater microhematuria or gross hematuria, or if patient has gross hematuria and free intraperitoneal fluid, a CT cystogram is performed to evaluate for bladder injury. Dedicated spine CTs, with smaller field of views and bone algorithm images are generated for improved evaluation of the spine. Dedicated pelvic CT with bone algorithm images and 3D reformations are generated if pelvic fractures are detected.
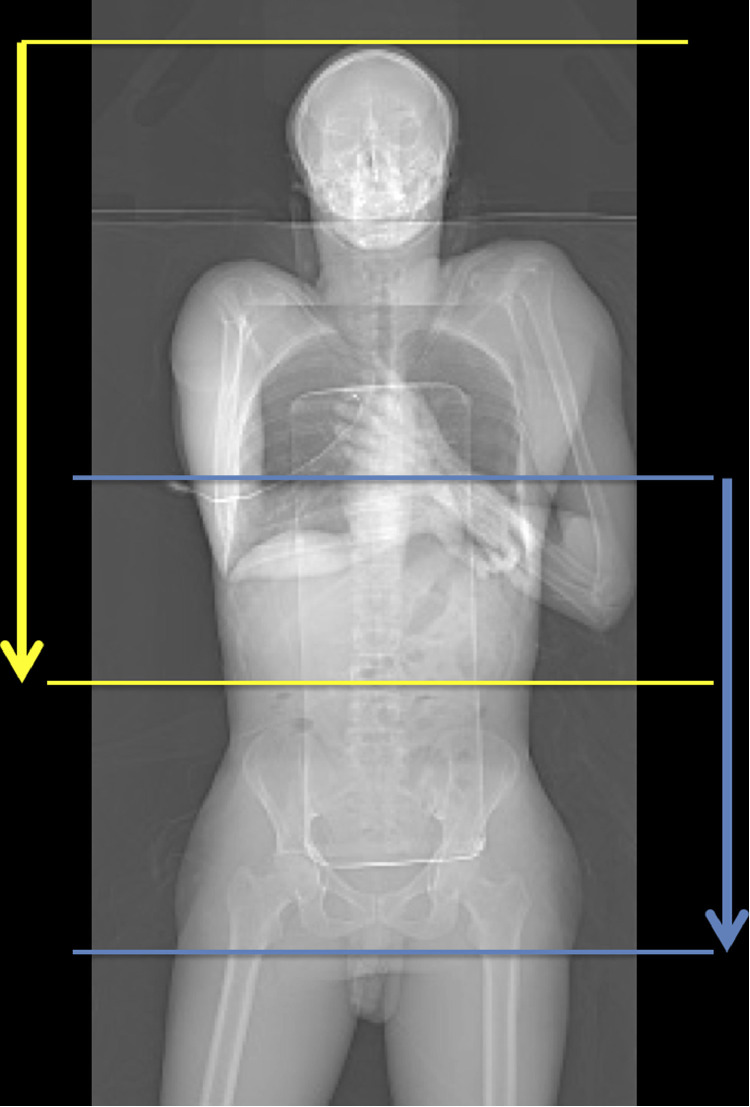
Figure 4.
Topogram illustrating the scan range of the midarterial (upper range) and venous (lower range) phases of the whole-body CT scan. Note the patient's arms are elevated above the abdomen by a bolster to minimize beam hardening artifact. (Color version of figure is available online.)
The timing for the arterial phase is a compromise between optimal timing and technique for a neck CTA and that of the chest and abdominal CTA but is believed to be adequate to detect most injuries. If a carotid or vertebral artery injury is identified or suspected, a dedicated neck CTA is retrospectively reconstructed with all the standard reformations and is usually adequate for diagnosis. If not, a repeat dedicated neck CTA can be performed, but this is rarely required.
Acute Stroke Imaging
Acute stroke care depends on speedy and accurate diagnosis of the cause of the immediate symptoms. Acute strokes are divided primarily between ischemic infarcts (87%) and intracranial hemorrhage (15%). Treatment of acute ischemic infarct is exquisitely time dependent. Intravenous tissue Plasminogen Activator (tPA) must be given within 4.5 hours of ictus. Intra-arterial clot retrieval needs to occur within 6 hours of ictus. Hemorrhage is an absolute contraindication to both Intravenous (iv) tPA and to intra-arterial clot retrieval.21 , 22 Current recommendations require immediate imaging with noncontrast head CT for patients who arrive within the treatment windows.
In our institution achieving the access goals required the emergency department, neurology, and radiology to evaluate the workflow from initial arrival in the ED, to transfer and imaging at the scanner, and of the processes that occur after the scan is completed. When an acute stroke patient is known to be arriving, the stroke team co-ordinates with ED personnel to ensure rapid transfer to CT. The ED physicians and nurses do an assessment of cardiovascular stability when the patient arrives. Electrocardiogram is deferred until a decision regarding acute stroke treatment is made.22 The CT techs are notified as early as possible that an acute stroke patient is either in the ED or is enroute. They identify which of the 3 potential scanners will be available when the patient arrives in the emergency department. Once basic cardiovascular stability is assured, the patient is transferred to the CT scanner for a noncontrast head CT. The patient remains in the scanner after the noncontrast head CT for the next steps, which occur in parallel: further clinical evaluation including determination of the National Institutes of Health stroke scale score, placement of an iv for the CTA, and set-up of the CTA. The radiologist is in the scanner control booth to look at the scan as the images are reconstructed and provides an immediate verbal interpretation. Through this clinical cooperation, we have achieved an average door-to-CT time (that is, the time from arrival to the time that CT scanning has begun) of 10 minutes for acute stroke patients in our institution.
Magnetic Resonance Imaging
MRI continues to be a limited resource, with very few scanners sited in the ED.23 , 24 There are well defined neurological emergency diagnoses that are best triaged with MR, such as neurologic deficits in the spine (cord compression, cauda equina syndrome, epidural abscess, and epidural hematoma).25 , 26 Other diagnoses in the ED setting, such as Transient Ischemic Attack vs small infarct, posterior fossa infarcts, multiple sclerosis exacerbation, encephalitis, and hypoxic brain injury may be inferred from the CT but are more easily made with MR. Regarding the effect of MRI utilization on LOS, recent publications have been mixed. While 1 study showed that increased use of MR in the ED increases ED LOS, downstream benefits included decreased admission rates, and shorter hospital LOS for those admitted after ED MRI.27 A more recent publication demonstrated decreased LOS with MRI readily available in the ED.28
Most MR imaging protocols have been designed for completeness, but these are often time-prohibitive in the ED environment, where patients cannot be scheduled, and have a higher than usual likelihood of being in pain and unable to remain still for a 30-minute exam. Abbreviated MR protocols specifically designed to answer a focused ED question can address both of these problems. Implementing such protocols requires collaboration between the emergency radiologists who will be using the exams and the subspecialists who may have more MR expertise in protocol design and be more comfortable with complete exams.29, 30, 31
Several studies have demonstrated that limited MRI to rule out a hip fracture, avascular necrosis, and muscle injury can be reliably performed32, 33, 34, 35 reducing scanning time by at least 20 minutes compared with the complete protocol, while maintaining high sensitivity and specificity.
Faster MRI protocols for abdominal imaging have also been proposed36 and are continuing to be developed. An abbreviated MR protocol for suspected appendicitis has been described which nearly halved the scanning time and markedly reduced the interpretation time.37 Adoption of these faster protocols would allow more MR imaging to take place in the ED, which we would expect to improve patient outcomes, management and workflow.
Completion or Convenience Imaging
Completion or convenience imaging poses another challenge for emergency imaging. This refers to imaging of the patient in the ED for nonurgent reasons, that would normally be performed as an outpatient.
For example, a patient who is due (in the near future) to have a multiphasic CT for follow up of cirrhosis and indeterminate lesions, or a cancer requiring multiphasic imaging, may present to the ED with suspected diverticulitis. The ED may request that the more extensive multiphasic imaging study (possibly including the chest, as well as the abdomen and pelvis) be performed to complete patient's imaging during this 1 visit and to make it more convenient, rather than having the patient return for further imaging. While this is a reasonable action to take to minimize radiation, contrast, and patient effort (especially if patient requires the assistance of others), interpretation of the larger and more complex study can delay interpretation of other emergent cases, negatively affecting patient care and ED throughput.
Other examples of convenience imaging include patients needing abdomen and pelvis CTs for acute findings, who also need an elective chest CT for follow up of pulmonary nodules or other nonacute pulmonary findings and patients undergoing CT of the chest (eg, for suspected pulmonary embolism) who require further evaluation of previously seen indeterminate renal or adrenal lesions.
Interpretation of the nonemergent portion of the study (eg, oncologic evaluation and staging) may be better performed by specialists in those fields, with more knowledge and experience with these types of studies, and perhaps less time pressures than might be present in the ED.
A system that allows the imaging to be performed in the ED and interpretation of the additional imaging by the appropriate specialist at a later date and/or time could enhance ED throughput and patient care. However, details of how to manage the studies, and concerns regarding later interpretation of portions of those studies, pose implementation challenges.
Disaster and Mass Casualty Preparedness
“By failing to prepare, you are preparing to fail.” ∼ Benjamin Franklin
Disasters and MCI are rare events which require work flows that are very different from every day radiology operations. When a disaster strikes, these alternate strategies already need to be in place in order to allow rational and efficient mitigation of the consequences of a disaster. It is very difficult if not impossible to adjust the “usual” radiology work flow on the fly during an ongoing disaster.38 “By failing to prepare, you are preparing to fail.”
Disaster clinical care differs fundamentally from standard clinical care because irrespective of the nature of the disaster, needs during a disaster will exceed resources available. During MCI disasters, the number of patients who need immediate imaging will be larger than the number of available standard imaging slots. Any attempt to process imaging requests during a disaster in a standard fashion will lead to bottlenecks that are likely to delay care downstream from imaging, which in turn may result in higher in-hospital disaster mortality.39 To avoid overwhelming system failure, the paradigm of care has to change during disasters from “the greatest good for each individual to the greatest good for the greatest number of victims.”38 Processes and workflows during disasters need to be adjusted accordingly.
The Process Map
Although disaster imaging workflows are different, they include the same elements as standard radiology workflows. These building blocks of the radiology work flow can be plotted as a process map ( Fig. 5) to include the multiple steps that occur from when imaging is requested to how imaging results are communicated.
Figure 5.
Process map of the MCI radiology workflow. Each step requires optimization to allow expedited patient throughput during disasters. Courtesy Eric Roberge, MD (personal communication, used with permission).
Each individual radiology MCI disaster plan will differ by institution taking into account available local resources and site-specific characteristics and circumstances. In addition, each radiology MCI disaster plan will necessarily need to be embedded in the hospital-wide disaster management plan, which in turn ties in with the regional disaster management plan. Therefore, each radiology MCI disaster plan should be developed, vetted and practiced in coordination with other subspecialties (eg, emergency medicine, trauma surgery) and specific local administrative units (hospital administration, regional disaster management authorities).38 Historically, radiology departments have often been underrepresented or excluded from disaster management plans.
Ordering of Studies, Transport
First responders in the field usually perform field triage according to well established triage criteria. Unfortunately, field triage is only moderately accurate. Disaster victims who are put in a falsely low category (under-triage) may be more severely injured than initially thought, resulting in poor individual outcomes. Disaster victims who are assigned to a falsely higher category (over-triage) put the health care system as a whole at risk because these patients are healthier than initially thought. Over-triaged patients may block critical limited resources (such as ICU beds or operating rooms), which could potentially save the life of sicker patients. Frykberg39 showed that over-triage during disasters is linearly related to higher in-hospital mortality during MCI disasters. It is through imaging that triage accuracy is improved (to avoid over-triage), thus permitting limited hospital resources to be used most efficiently. Although approaches may differ regionally, providers at a specific hospital must agree which patients should get imaging studies during MCI disasters to avoid bottle necks. Equally important is reliable patient tracking through the radiology department once the decision is made to perform imaging on a patient, keeping in mind that electronic medical records may not be operational or sufficient during MCI disasters. Many patients are likely to arrive by private vehicle or walk into the emergency department during MCI disasters and plans for rapid registration and in-hospital triage of these patients at the front door needs to be in place.40 , 41
Imaging during MCI disasters usually includes point-of-care ultrasound, radiography and CT scanning. Selected patients may receive angiographic procedures. During MCI disasters it may be necessary to make additional capacity available for ED patients. The amount by which capacity can be increased will depend on the specific hospital environment (numbers of scanners installed). It is helpful to take inventory of available resources (scanners) and the minimal personnel necessary to run it (staffing grid) well before disaster hits. Arrangements about how to make additional capacity available (bring scanners online for MCI) need to be specified and practiced (eg, postpone inpatient scans, clear outpatient scanners). Additional staff (technologists, radiologists, clerical, transportation, runners) may need to be called in, which requires robust, multimodality methods of communication to reach employees who are off shift (phone lists, email, social media, paging).38 , 42 , 43
In our experience, WBCT scanning is the most common imaging during MCIs,38 , 42 but more restrictive approaches have been reported.44
Protocol, Schedule, Imaging, Processing
CT imaging during MCI disasters should be optimized for robust imaging quality and high throughput (Table ). Standardized comprehensive MCI protocols should be utilized for all patients who are imaged during the surge phase of MCIs in order to eliminate the need for individual study protocolling and additional communication.45 These standardized CT protocols should be preprogrammed into all scanners to be readily available when MCI disasters occur. Thin collimation images and multiple reconstructions are to be avoided as network overload may result when too many images need to be transferred to PACS.46
Table.
MCI CT Protocols, Optimized for Fast Throughput and Robust Image Quality
| Harborview MCI Protocol | Koerner et al 200942 | |
|---|---|---|
| Head | NC head CT, 5 mm, brain | NC head CT, 5 mm, brain |
| Torso | Arterial neck/chest, 1.5 mm, ST | PV chest abdomen pelvis, 5 mm, ST |
| PV Abdomen pelvis, 3 mm, ST | ||
| Reformations | Sagittal and coronal, 3 mm, ST | None |
Arterial, arterial phase; NC, noncontrast; PV, portal venous phase; ST, soft tissue algorithm.
Reformations include the whole spine with bone algorithm images.
PACS, Interpretation, Communication
Preliminary image interpretation during MCIs often occurs directly at the CT scanner console to increase interpretation speed and facilitate ease of communication while the patient is still physically in the imaging suite. These preliminary imaging interpretations can be documented on standardized paper preliminary report forms with carbon copies.42 A priori identification of a single point person for communication of critical results can be helpful.
MCI Conclusion
The elements of the radiology work flow process require adaptation for MCI disasters. Such radiology disaster plans (see Appendix) need to be developed in an iterative process in advance, because MCI disasters are rare and it is impossible to adapt standard work flows on the fly.
Summary
Emergency Radiology has developed as a distinct subspecialty in Radiology. While the clinical subject matter spans most other subspecialties, the manner in which it is practiced has its own requirements and obligations. Every practice should have at least 1 member whose responsibility is to manage this important segment of a complete radiology service.
Addendum
Following completion of this manuscript, the outbreak of the coronavirus pandemic brought another dimension of Emergency Radiology to the fore. While the role of imaging in the diagnosis and management of COVID-19 is not as central as in many other conditions, the strictures of appropriate infection control make routine procedures as difficult for radiology technologists as it is for other clinical providers. We would like to share an innovation that may be used to improve operational efficiency without sacrificing patient care or operator safety.
We have implemented a protocol to image patients through the glass window of an isolation room that allows us to reduce the risk of transmission, increase speed of acquisition, and conserve resources. The technologist operates the portable radiographic unit from the hallway without having to don personal protective equipment. The digital image receptor is double bagged and passed through the isolation room door to a care provider (typically nursing staff) inside the room, who assists in the positioning of the exam. Guidance from the technologist is provided by telephone. If possible, the patient stands upright and holds the receptor against their own chest and faces away from the window for a PA chest view, otherwise the receptor is placed behind the patient in a bed or wheelchair as typical for a portable exam. The x-ray tube is positioned as close as possible to the window and the image is taken through the glass. An increase in exposure technique is necessary to account for the glass material as well as an increase in the source-to-image distance (SID). Portable lead shields and increasing distance are used to protect staff from scattered radiation from the patient and glass window. After confirming the image is satisfactory on the integrated portable monitor, the receptor's outer bag is disinfected and opened by staff inside the isolation room, and carefully peeled back. The technologist outside the room receives the receptor while only touching the inner bag, and the outer bag remains in the room. The inner bag is then wiped down and the receptor can be removed. The images acquired using this technique are of good quality, and generally difficult to distinguish from conventional portable radiographs.
Acknowledgement
Acknowledgement: Thanks to Jeff Moirano for preparation of this addendum.
Appendix
Radiology Disaster Activation Plan
Background:
-
•
In case of disasters and mass casualty incidents, emergency radiology surge capacity needs to be utilized.
-
•
Disaster activation on the hospital side will include activation and use of the incident command center for central coordination if disaster or MCI are big enough. Radiology personnel in the command center include the administrative director of radiology. Imaging supervisors and Chief of Service will be informed in the second tier by the administrative director.
-
•
The operational disaster activation plan (Version May 2017) will be replaced by this document.
-
•
In case of disaster, the emergency radiologist in house will assume the role of Radiology Control Officer (RCO), (attending 0700 to 2159 hours, on call radiology resident 2200 to 0659) will be notified by lead technologist, Medical Control Officer (MCO) or ED charge nurse. Coordination between Radiology and Emergency Medicine (EM) will rely on the Imaging Control Officer (ICO), who is an Emergency Medicine Physician (new role) coordinating imaging.
Activation of Surge Plan:
-
1.
Additional radiology personnel may be required if the expected number of victims exceeds 5 severely injured patients (major trauma). Need for additional personnel will be decided on case-by-case basis by the RCO in coordination with ICO.
-
2.
2200 to 0659 hours: On-call radiology resident pages back-up resident and attending emergency radiologist to come to the hospital (physical presence required).
-
3.
0700-2159 hours: Attending Emergency Radiologist on shift activates plan.
-
4.Activation of additional radiologists (if necessary):
-
a.Call ERad Faculty from list (cell phone group text, cell phone call, See appendix 1): First person to respond to call is delegated responsibility of further activation. If first responder is unable to co-ordinate, then second responder.
-
a.
-
5.Radiology team structure for mass casualty response:
-
a.Depending on size, time and nature of mass casualty teams will be assembled according to the staffing grid as outlined in appendix 2.
-
a.
Radiologist Roles:
-
1.
On-call radiology resident assumes the role of lead radiologist in Emergency Radiology (RCO) until the attending arrives.
-
2.
The emergency radiologist on call is by default the lead radiologist (RCO) who delegates radiologist responsibilities.
-
3.Interventional radiology and neuroradiology operate under a separate plan:
-
a.IR and NeuroRad fellow will be paged and asked to come to the hospital (ERad schedulers; See separate document for schedulers).
-
a.
-
4.
Use job action cards (deck of cards in MCI box for radiologists and technologists, see Appendix 3).
Radiologist Elements:
-
1.Communication:
-
a.Nature of disaster (blunt, penetrating, blast, chemical, natural disaster).
-
b.Anticipated number of patients expected at HMC.
-
c.Anticipated time of first MCI patient arrival.
-
d.Anticipated mode of registration (paper-based vs EMR).
-
e.Anticipated duration of event: Will it be necessary to organize a relief team?
-
fImaging control officer (ICO) and emergency radiology lead radiologist (RCO) determine patient queue for CT scanning (priority).
-
a.
-
2.Personnel resources:
-
a.The predesignated meeting area for available Emergency Radiologists (attendings, fellows, residents assigned to ED) is the Emergency Radiology Reading Area (room number 1WH416, across from ED fish bowl).
-
b.Current team designation (minimum): lead radiologist (RCO), on-shift fellow, on-shift resident, backup-resident.
-
c.Relief team designation: attending who is scheduled to be on the next shift will lead relief team (relief team RCO) and will organize providers to come in for new shift.
-
d.Radiology residents: volunteer radiology residents will be alerted by HMC telecommunications as part of group 2. Radiology Residents will be assigned to their roles by RCO and relief RCO.
-
e.Radiology IT: HMC radiology IT site manager will be alerted by HMC telecommunications as part of group 2. Radiology IT site manager will come to HMC in case of mass casualty activation or delegate to one of her team members.
-
f.Neuroradiology fellow on call will be paged by HMC ED radiology scheduler and asked to come to the hospital for disaster activation/MCI. Neuroradiology fellow will talk to ICO in person and then coordinate with Neuroradiology attending and rest of the Neuroradiology team.
-
g.IR fellow on call will be paged by HMC ED radiology scheduler and asked to come to the hospital for disaster activation/MCI. IR fellow will talk to ICO in person and then coordinate with IR attending and rest of the IR team.
-
a.
-
3.Responsibilities:
-
a.Clear scanners (techs, RCO).
-
b.Activate MCI CT scanning protocol (see online CT protocols): noncon head, MCI pan-scan with sagittal and coronal reformations (no arm bolstering, no delays, no spine reformats, no extra recons) as fast as possible. During MCI surge, all CT scans will be performed in this fashion without protocolling. We return to tailored scanning with protocolling in the recovery phase. MCI CT protocol is programmed into all scanners. If there is any problem with contrast injection (bad IV, injector problem, history of severe contrast allergy), perform scan as noncontrast study (backup MCI scanning protocol).
-
c.Open radiologist MCI box, which is located in the cabinet next to the PA/fellow workstation in room 1WH416.
-
i.Paper based reporting (CT and x-ray):
-
a.White copy: Stays with scheduler: filed in radiology area for viewing by providers who want to (alphabetic box).
-
b.Yellow copy: Stays with radiologists: reference and reconciliation during recovery.
-
c.Pink copy: Goes with patient: becomes part of paper package.
-
d.Copies of the paper-based MCI radiology CT and x-ray requisitions are also be available in the Disaster Registration packages.
-
a.
-
ii.Hand out “Job Action Cards” to available team members (Appendix 3 & 4). Adjust number of cards based on available personnel and number of expected patients. (Each staff person may have more than 1 role).
-
a.RCO lead radiologist: scan coordination and communication.
-
b.Patient flow co-ordinator.
-
c.Trauma series radiologist.
-
d.CT2 scanner radiologist.
-
e.CT3 scanner radiologist.
-
f.CT1 scanner radiologist.
-
g.Plain film radiologist.
-
h.Runners (between ICO, RCO, and scanners).
-
a.
-
i.
-
d.Coordination: The MCO is in charge of the ED and has a white board at the back-triage desk of the ED. Imaging is coordinated by the ICO in coordination with MCO and RCO. CT scanner queue will be created and updated by ICO in coordination with RCO. ICO will circulate between Room Captains (EM or Surgery doc coordinating a geographic ED area) and Trauma Surgery Captain (who decides priority for OR). If a patient needs more expedited CT scanning, Imaging Control Officer (ICO) has to be informed (chain of command). If hyper-acute inpatient requests for scanning are submitted (Stroke, PE), the ICO needs to be consulted and floor patient gets added to the MCI CT queue.
-
i.Studies will be requested on paper forms that are in the patient packages and will be available at the scanners.
-
ii.Results are communicated as prelims on PINK paper copies, which are to stay and travel with patient (different form for CT and x-ray).
-
i.
-
a.
-
4.Recovery:
-
a.Patient administration returns to electronic format (ORCA, RIS, PS360).
-
b.CT scanning returns to protocolled tailored approach.
-
c.Paper MCI radiology reports get reviewed and dictated in RIS/PS360:
-
i.Use macro “ERAD MCI CT recovery” for final CT reports.
-
ii.Use macro “ERAD MCI X-RAY recovery” for final X-RAY reports.
-
iii.Reconciliation with Canary copy of paper-based MCI reports.
-
iv.All CT images will be in the same exam folder. Head CTs will get a white pointer sheet like OSH reports.
-
v.All x-ray images acquired during MCI will be under a single accession number in 1 exam folder.
-
i.
-
d.Complete after action report.
-
a.
Imaging Supervisor Roles:
-
1.
If occurring during off hours, on-call supervisor will contact Director of Radiology to establish communication and determine the severity of the event.
-
2.Make contact with lead techs to ensure staffing is adequate to staff trauma x-ray portables, suites, and CT scanners according to the MCI staffing matrix (see Appendix 2) when expected number of patients exceeds 5 severely injured patients.
-
a.Determine current radiology staffing levels in Trauma x-ray, Main x-ray, CT, NJB and the OR. By default, OR techs will remain in OR.
-
b.Determine how many HAs and students are available for support roles.
-
a.
-
3.If staffing is not adequate, on-call supervisor will attempt to make contact with Associate Director or an additional supervisor. If contact is made, the on-call supervisor will inform the Associate Director/Supervisor about staffing needs and direct him/her to begin calling staff to attain proper staffing levels.
-
a.Associate Director/Supervisor will utilize the emergency contact lists to call technologists to determine if they are available to come to HMC.
-
a.
-
4.
When additional staffing is needed, on-call supervisor will travel to HMC.
-
5.
Ensure technologist MCI box is located in the radiology core (room 1WH416 scheduler file cabinet) and open it.
-
6.
Coordinate with leads to assign roles/role cards from MCI box (If on-site.)
-
7.
Supervisors will monitor staffing and anticipate staffing changes associated with shift change. Call additional technologists as necessary.
-
8.Pre-assigned meeting point for additional called-in technologist staff is the lead office (1WH314). The on-call supervisor will assign roles to them there.
-
a.Communicate names of additional staff called in on the whiteboard in the lead office including their assignment upon arrival.
-
b.Provide role cards to called-in staff.
-
a.
-
9.Announce when recovery phase has begun and assign technologists to recovery tasks.
-
a.Reassess staffing levels and formulate a plan for a return to normal staffing.
-
b.Officially announce when recovery has commenced.
-
a.
Trauma x-ray Lead Roles:
-
1.
Inform on-call supervisor of any gaps in coverage. At baseline for an MCI event, 1 x-ray suite and 3 portables should be fully staffed. Two portable teams would work in Resus 2 and 3, an additional team will be assigned to blue and/or green.
-
2.
If not fully staffed, call in the call tech.
-
3.
Inform scheduler of MCI plan activation.
-
4.
Coordinate with supervisor and assign role cards for each technologist for each x-ray suite/portable.
-
5.
Provide paper copy of MCI x-ray form to each portable and x-ray suite
-
6.
After portable x-rays obtained, paper order/report (the Mass Casualty Emergency Radiology Preliminary Report) needs to travel to x-ray radiologist (ERAD 3).
-
7.
The x-ray Lead will facilitate communication between each x-ray suite and inform the runner when an x-ray suite is ready for the next patient.
-
8.
Coordinate recovery processes as assigned.
CT Lead Roles:
-
1.
Inform on-call supervisor of any gaps in coverage. At baseline for an MCI event, all scanners should be fully staffed.
-
2.
If not fully staffed, call in the call tech.
-
3.
Inform scheduler of MCI plan activation.
-
4.
Coordinate with supervisor and assign role cards for each scanner.
-
5.
Provide paper copy of MCI CT form to each scanner.
-
6.
The CT Lead will facilitate communication between each scanner and communicate to the runner when a scanner is ready for the next patient.
-
7.
Coordinate recovery processes as assigned.
-
8.
We will not screen for renal function or contrast allergy during MCI.
x-ray Technologist Roles (10 technologists):
-
1.
Portable team 1 (Resus 2, 2 technologists).
-
2.
Portable team 2 (Resus 3, 2 technologists).
-
3.
Portable team 3 (Blue/Green, 2 technologists).
-
4.
Trauma x-ray 1 (2 technologists).
-
5.
Trauma x-ray 2 (2 technologists).
Trauma series will not be paged overhead during MCI events. Trauma series will be verbally called in the RESUS rooms (ED Room Captain). For these verbal orders, technologists must fill out a paper order so the radiologist has something on which to report preliminary findings.
During MCI events, we will only obtain 2 view chest, abdomen, and spine x-rays. AP views will be obtained for long bones which include both joints on 1 exposure. Lateral views will be obtained when technologist identifies any fracture or abnormality. If additional imaging/views are requested, inform the physician that those exams should be ordered after the MCI event has moved into the recovery phase.
CT Technologist Roles (6 technologists):
-
1.
Scanner Tech CT 3/Room Tech CT 3 (AS+).
-
2.
Scanner Tech CT 2/Room Tech CT 2 (FORCE).
-
3.
Scanner Tech CT 1/Room Tech CT 1 (EDGE).
We will not screen for renal function or contrast allergy during MCI.
HA/Student Roles:
-
1.
Runners.
-
2.
CT room support (at least 1 per room).
Scheduler Roles:
-
•
During an MCI event ORCA/RIS electronic workflows may stop (decision to be made by MCO) and we then will move to paper workflows.
-
•
The ED schedulers will receive notification and updated information about the MCI from the Imaging Leads or Supervisor.
-
•Once notification is received, the schedulers will do these things to prepare:
-
○Page on-call IR and Neuroradiology fellows to come to hospital.
-
○Schedulers will circulate to all CT scanners and x-ray suites and gather completed preliminary reports (white forms) from designated trays. These trays will hold completed white forms for techs to place the white copy for schedulers to reference. Schedulers will collect white forms and file in Rad reading area in alphabetic order.
-
○Await instructions from Imaging Lead/Supervisor
-
○
-
•During MCI:
-
○Schedulers will be assigned a role in the MCI by the Imaging Leads or Supervisor. Roles could include runners, room support, inpatient scheduling, other communication roles.
-
○A runner facilitates communication between the ED and a radiology suite. A runner's role is to notify ED staff when a suite is available to image the next patient and minimize the idle time between patients.
-
○Schedulers may begin entering orders in RIS before the MCI has concluded.
-
○
-
•After MCI:
-
○Schedulers will schedule all exams performed during the MCI in RIS to initiate the clean-up/recovery effort.
-
○
Schedulers will play a key role in the cleanup and recovery process after the MCI is over. Schedulers will schedule all exams performed during the MCI in RIS to initiate the clean-up/recovery effort. See separate document for details.
Appendix 1: Call list Emergency Radiology (not included).
Appendix 2: Radiology Mass Casualty Staffing Grid.
Appendix 3: EmRad Job Action Cards.
Appendix 4: Radiology Technologist Job Action Cards.
References
- 1.Baker S.R. Emergency radiology in the United States—a stepchild finding its way. Br J Radiol. 2015;89 doi: 10.1259/bjr.20150867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatem S.F., Novelline R.A. Looking back, moving forward: 1988-2013. The first 25 years of the American Society of Emergency Radiology. Emerg Radiol. 2014;21:115–132. doi: 10.1007/s10140-013-1182-0. [DOI] [PubMed] [Google Scholar]
- 3.Harris J.H. Reflections: Emergency radiology. Radiology. 2001;218:309–316. doi: 10.1148/radiology.218.2.r01fe41309. [DOI] [PubMed] [Google Scholar]
- 4.Choy G., Novelline R.A. Past, present, and future of emergency radiology. Can Assoc Radiol J. 2013;64:85–89. doi: 10.1016/j.carj.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Goldman S.M. Emergency radiology as a sub-speciality has come of age. Eur J Radiol. 2004;50:3–4. doi: 10.1016/j.ejrad.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Chong S.T., Robinson J.D., Davis M.A. Emergency radiology: Current challenges and preparing for continued growth. J Am Coll Radiol. 2019;16:1447–1455. doi: 10.1016/j.jacr.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Robinson J.D., Linnau K.F., Hippe D.S. Accuracy of outside radiologists' reports of computed tomography exams of emergently transferred patients. Emerg Radiol. 2018;25:169–173. doi: 10.1007/s10140-017-1573-8. [DOI] [PubMed] [Google Scholar]
- 8.Center for Medicare and Medicaid Services . Version 5.5a ed. Washington, DC; 2018. The Joint Commission. Specifications manual for national hospital inpatient quality measures. [Google Scholar]
- 9.Robinson J.D., Hippe D.S., Deconde R.P. Emergency radiology: An underappreciated source of liability risk. J Am Coll Radiol. 2019;17:42–45. doi: 10.1016/j.jacr.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Levey R. Placing a radiologist in the ED. Personal Commu. 2019 [Google Scholar]
- 11.Stern S. Integration of coronary CTA into emergency medicine algorithms. Personal Commun. 2017 [Google Scholar]
- 12.Rigual D., Rove M., Robison Z. Emergency department CT expediency: A time reduction by redesign. J Am Coll Radiol. 2016;13:178–181. doi: 10.1016/j.jacr.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Livingston D.H., Lavery R.F., Passannante M.R. Admission or observation is not necessary after a negative abdominal computed tomographic scan in patients with suspected blunt abdominal trauma: Results of a prospective, multi-institutional trial. J Trauma. 1998;44:273–280. doi: 10.1097/00005373-199802000-00005. discussion 80-2. [DOI] [PubMed] [Google Scholar]
- 14.Tillou A., Gupta M., Baraff L.J. Is the use of pan-computed tomography for blunt trauma justified? A prospective evaluation. J Trauma. 2009;67:779–787. doi: 10.1097/TA.0b013e3181b5f2eb. [DOI] [PubMed] [Google Scholar]
- 15.Mowery N.T., Dougherty S.D., Hildreth A.N. Emergency department length of stay is an independent predictor of hospital mortality in trauma activation patients. J Trauma. 2011;70:1317–1325. doi: 10.1097/TA.0b013e3182175199. [DOI] [PubMed] [Google Scholar]
- 16.Huber-Wagner S., Lefering R., Qvick L.M. Effect of whole-body CT during trauma resuscitation on survival: A retrospective, multicentre study. Lancet. 2009;373:1455–1461. doi: 10.1016/S0140-6736(09)60232-4. [DOI] [PubMed] [Google Scholar]
- 17.Geyer L.L., Korner M., Harrieder A. Dose reduction in 64-row whole-body CT in multiple trauma: an optimized CT protocol with iterative image reconstruction on a gemstone-based scintillator. Br J Radiol. 2016;89 doi: 10.1259/bjr.20160003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ptak T., Rhea J.T., Novelline R.A. Radiation dose is reduced with a single-pass whole-body multi-detector row CT trauma protocol compared with a conventional segmented method: Initial experience. Radiology. 2003;229:902–905. doi: 10.1148/radiol.2293021651. [DOI] [PubMed] [Google Scholar]
- 19.Sedlic A., Chingkoe C.M., Tso D.K. Rapid imaging protocol in trauma: a whole-body dual-source CT scan. Emerg Radiol. 2013;20:401–408. doi: 10.1007/s10140-013-1139-3. [DOI] [PubMed] [Google Scholar]
- 20.Yaniv G., Portnoy O., Simon D. Revised protocol for whole-body CT for multi-trauma patients applying triphasic injection followed by a single-pass scan on a 64-MDCT. Clin Radiol. 2013;68:668–675. doi: 10.1016/j.crad.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 21.Powers W.J., Rabinstein A.A., Ackerson T. 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–e110. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 22.Boulanger J.M., Lindsay M.P. Canadian stroke best practice recommendations for acute stroke management: Prehospital, emergency department, and acute inpatient stroke care, 6th edition, update 2018. Int J Stroke. 2018;13:949–984. doi: 10.1177/1747493018786616. [DOI] [PubMed] [Google Scholar]
- 23.Buller M., Karis J.P. Introduction of a dedicated emergency department MR imaging scanner at the Barrow Neurological Institute. AJNR Am J Neuroradiol. 2017;38:1480–1485. doi: 10.3174/ajnr.A5210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yousem D.M., Pakpoor J., Babiarz L. Emergency department MR imaging scanner: Supportive data. AJNR Am J Neuroradiol. 2017;38:E88. doi: 10.3174/ajnr.A5315. United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah L.M., Long D., Sanone D. Application of ACR appropriateness guidelines for spine MRI in the emergency department. J Am Coll Radiol. 2014;11:1002–1004. doi: 10.1016/j.jacr.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Rozell J.M., Li S. Recognition and appropriate use of magnetic resonance imaging for emergent neuroradiology. Semin Ultrasound CT MR. 2017;38:424–438. doi: 10.1053/j.sult.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Redd V., Levin S., Toerper M. Effects of fully accessible magnetic resonance imaging in the emergency department. Acad Emerg Med. 2015;22:741–749. doi: 10.1111/acem.12686. [DOI] [PubMed] [Google Scholar]
- 28.Gil H., Tuttle A.A., Dean L.A. Dedicated MRI in the emergency department to expedite diagnostic management of hip fracture. Emerg Radiol. 2020;27:41–44. doi: 10.1007/s10140-019-01729-5. [DOI] [PubMed] [Google Scholar]
- 29.Sanchez Y., Yun B.J., Prabhakar A.M. Magnetic resonance imaging utilization in an emergency department observation unit. West J Emerg Med. 2017;18:780–784. doi: 10.5811/westjem.2017.6.33992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glover M., Gottumukkala R.V., Sanchez Y. Appropriateness of extremity magnetic resonance imaging examinations in an academic emergency department observation unit. West J Emerg Med. 2018;19:467–473. doi: 10.5811/westjem.2018.3.35463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pakpoor J., Saylor D., Izbudak I. Emergency department MRI scanning of patients with multiple sclerosis: Worthwhile or wasteful? AJNR Am J Neuroradiol. 2017;38:12–17. doi: 10.3174/ajnr.A4953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kumaravel M., Weathers W.M. Emergency magnetic resonance imaging of musculoskeletal trauma. Magn Reson Imaging Clin N Am. 2016;24:391–402. doi: 10.1016/j.mric.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 33.Ross A.B., Chan B.Y., Yi P.H. Diagnostic accuracy of an abbreviated MRI protocol for detecting radiographically occult hip and pelvis fractures in the elderly. Skeletal Radiol. 2019;48:103–108. doi: 10.1007/s00256-018-3004-7. [DOI] [PubMed] [Google Scholar]
- 34.Khurana B., Okanobo H., Ossiani M. Abbreviated MRI for patients presenting to the emergency department with hip pain. AJR Am J Roentgenol. 2012;198:W581–W588. doi: 10.2214/AJR.11.7258. [DOI] [PubMed] [Google Scholar]
- 35.Kotecha H.M., Lo H.S., Vedantham S. Abbreviated MRI of the foot in patients with suspected osteomyelitis. Emerg Radiol. 2020;27:9–16. doi: 10.1007/s10140-019-01722-y. [DOI] [PubMed] [Google Scholar]
- 36.Canellas R., Rosenkrantz A.B., Taouli B. Abbreviated MRI protocols for the abdomen. Radiographics. 2019;39:744–758. doi: 10.1148/rg.2019180123. [DOI] [PubMed] [Google Scholar]
- 37.Mian M., Khosa F., Ali I.T. Faster magnetic resonance imaging in emergency room patients with right lower quadrant pain and suspected acute appendicitis. Pol J Radiol. 2018;83:e340–e3e7. doi: 10.5114/pjr.2018.77790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Berger F.H., Korner M., Bernstein M.P. Emergency imaging after a mass casualty incident: role of the radiology department during training for and activation of a disaster management plan. Br J Radiol. 2016;89 doi: 10.1259/bjr.20150984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frykberg E.R. Medical management of disasters and mass casualties from terrorist bombings: how can we cope? J Trauma. 2002;53:201–212. doi: 10.1097/00005373-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Landman A., Teich J.M., Pruitt P. The Boston Marathon Bombings mass casualty incident: One emergency department's information systems challenges and opportunities. Ann Emerg Med. 2015;66:51–59. doi: 10.1016/j.annemergmed.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 41.Menes K., Tintinalli J., Plaster L. 2017. How One Las Vegas ED Saved Hundreds of Lives after the Worst Mass Shooting in US History.https://epmonthly.com/article/not-heroes-wear-capes-one-las-vegas-ed-saved-hundreds-lives-worst-mass-shooting-u-s-history/ Available at: Accessed April 1, 2019. [Google Scholar]
- 42.Bolster F., Linnau K., Mitchell S. Emergency radiology and mass casualty incidents-report of a mass casualty incident at a level 1 trauma center. Emerg Radiol. 2017;24:47–53. doi: 10.1007/s10140-016-1441-y. [DOI] [PubMed] [Google Scholar]
- 43.Brunner J., Rocha T.C., Chudgar A.A. The Boston Marathon bombing: after-action review of the Brigham and Women's Hospital emergency radiology response. Radiology. 2014;273:78–87. doi: 10.1148/radiol.14140253. [DOI] [PubMed] [Google Scholar]
- 44.Young V.S., Eggesbo H.B., Gaarder C. Radiology response in the emergency department during a mass casualty incident: A retrospective study of the two terrorist attacks on 22 July 2011 in Norway. Eur Radiol. 2017;27:2828–2834. doi: 10.1007/s00330-016-4677-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Korner M., Krotz M.M., Wirth S. Evaluation of a CT triage protocol for mass casualty incidents: Results from two large-scale exercises. Eur Radiol. 2009;19:1867–1874. doi: 10.1007/s00330-009-1361-2. [DOI] [PubMed] [Google Scholar]
- 46.Amoretti N. Terrorist attack in Nice, France, in July 2016: Massive influx of patients to a radiology department. Radiology. 2018;288:2–3. doi: 10.1148/radiol.2018172915. [DOI] [PubMed] [Google Scholar]