Abstract
As the world witnessed the rapid spread of SARS-CoV-2, the World Health Organization has called for governing bodies worldwide to intensify case findings, contact tracing, monitoring, and quarantine or isolation of contacts with COVID-19. Drive-through (DT) screening is a form of case detection which has recently gain preference globally. Proper implementation of this system can help remediate the outbreak.
Keywords: COVID-19, Drive-through screening, Pandemic
Introduction
In December 2019, the world received reports of unusual cases of pneumonia emerging from Wuhan, China. The causative pathogen was identified as a novel coronavirus (2019-nCoV), which was then named severe acute respiratory syndrome-related coronavirus-2 (SARS-CoV-2).1 Global transmission and exponential increase in the number of cases led to the declaration of a pandemic by the WHO on 11 March 2020. The WHO called for governing bodies worldwide to intensify case findings, contact tracing, monitoring, and quarantine or isolation of contacts with COVID-19.2 The WHO also emphasized the three golden rules of epidemic control, namely test, test, and test again. Considering that four-fifths of individuals who harbor the virus can be asymptomatic,3 infected individuals potentially spreading the disease 2–4 days before exhibiting symptoms is a major concern. To date, screening and laboratory testing strategies are based on defined transmission scenarios,4 and these must be tailored to the testing capacity of the country.
During an outbreak, passive and active case detection form the fundamentals of disease control programs. Passive case detection (PCD) is instigated when patients self-present to a medical facility. A lesser-known method of PCD is drive-through (DT) screening. Eric Weiss and Gregory Gilbert first described drive-through screening as a safer option for PCD during the 2009 H1N1 influenza outbreak.5 The concept of drive-through screening was welcomed. It was based on the idea of cars treated as self-contained units to reduce the spread of infection. Following this approach, South Korea was the first country to initiate drive-through screening for the COVID-19 pandemic.6
Methods
Location
A designated DT screening area (ground floor, open-air, and covered area of the hospital) has been chosen to reduce congestion. A workstation has been set up for the screening staff 10 m from the DT area. The site is only accessible by car through a single entrance. It should accommodate only a single vehicle at any time, and the flow of traffic should be in a single direction. Two wardens have been deployed for overall traffic control and identity verification. The DT screening team consists of two nurses and a doctor. They take charge of the screening session planned for the day. The morning session is from 9:00 to 14:00 and the afternoon session lasts from 15:00 to 18:00. Members of the DT screening team are required to wear full personal protective equipment (PPE) as per WHO recommendations.7
Stages of DT screening
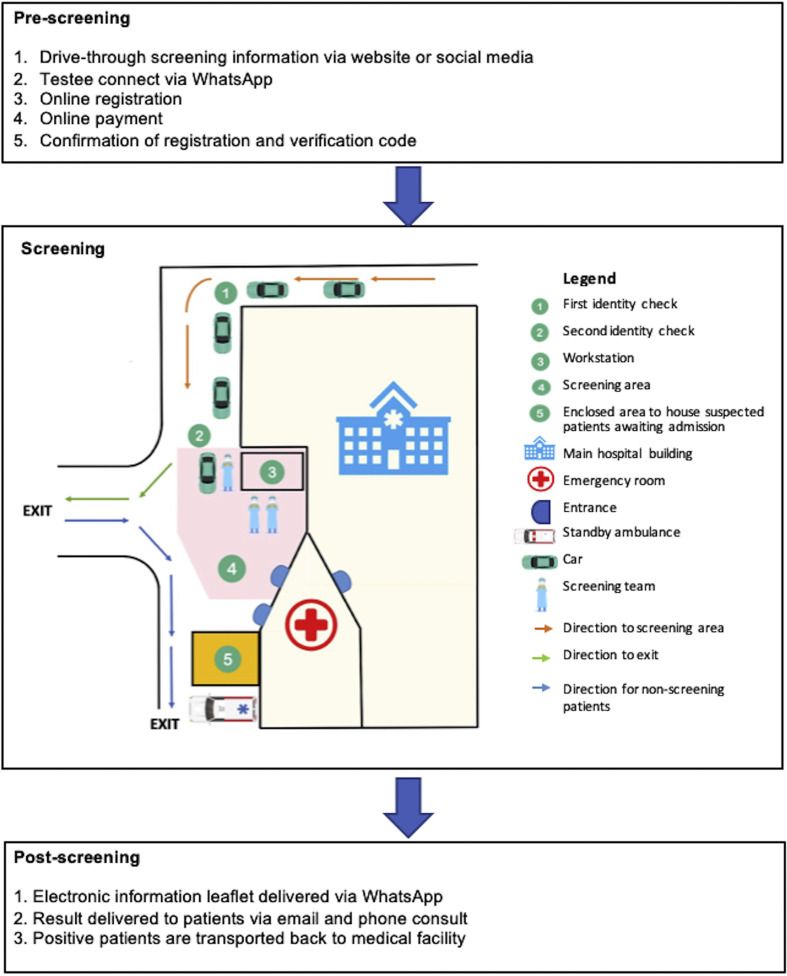
The DT screening is a paperless process consisting of three stages. It can be divided into prescreening, screening, and post-screening. During prescreening, relevant information is distributed through various platforms. These can be an official website or social media. Individuals interested in screening can dial and connect to the hospital through an instant messaging application (IMA) WhatsApp (owned by Facebook). Instructions for the DT screening are provided before the online registration. A link will be provided to connect individuals to a secure site for registration. The registration requires essential data such as name, age, gender, nationality, identification number, and residential address. Upon completion, the testee will be directed to make a secure online payment. Once the process has been finalized, the testee will receive details of the appointment (date and time) and a verification code will be sent to their cellphone and email address. The hospital uses the registration information to make necessary arrangements before the testee's arrival.
The screening process is based on the “swab and go” approach. The testee is advised to arrive on time. They are required to go through an initial identity check at the entrance of the DT screening by displaying their verification code from their cellphone. Following this, the testee will drive to the DT area, and a second identity check will be performed. The second verification is to ensure the correct testee identification labels are applied to the samples (sample labels are pre-prepared and arranged in sequence according to appointment details). The DT screening requires drivers to turn off air conditioning before lowering their car windows. The patient's body temperature is recorded using infrared thermography. They are briefly evaluated, and all information are recorded in a computerized system. The doctor than proceeds nasopharyngeal and oral pharyngeal swabs through the car window. The entire screening process (arrival to departure) takes 5–8 min.
Post-screening, an electronic information leaflet will be delivered to the testees’ cellphone together with advice to seek medical advice should their symptoms have worsened. The results are delivered via email and through a phone call from a doctor within 24–72 h. Positive individuals are transported back to the hospital by an ambulance. (Fig. 1 ) illustrates the entire paperless DT screening.
Figure 1.
Illustration of the COVID-19 paperless DT screening. DT = Drive through, COVID-19 = Coronavirus 2019.
Discussion
Relevance
Following the H1N1 outbreak in 2009, the idea of DT screening programs did not take off until the COVID-19 pandemic. It is indisputable that emergency rooms (ERs) are seeing higher patient loads, and this may outstrip the crisis response capacity of a hospital. The emergence of DT screening was based on the concept of reducing the burden on ERs and avoiding congestion and overcrowding of patients to mitigate person-to-person transmission, especially when dealing with airborne or droplet transmittable diseases. In a pilot study, Weiss et al. demonstrated that a DT screening model resulted in a shorter median time spent at the hospital without compromises to patient care.5 During a pandemic, streamlined workflows and effective workforce management can help improve hospital efficiency. Trained medical personnel can assess stable patients based on predefined standard protocols. Thus, critically ill cases can be attended promptly by ER doctors. The appropriate disposition of outpatients is key to freeing up spaces in the ER.8
DT screening is also a suitable means for identifying asymptomatic individuals and those with mild symptoms and advising home quarantine to help reduce overall medical expense and free up hospital beds.
In terms of safety, DT screening is conducted in a designated open area with adequate ventilation. This precludes the need to pressurize rooms. Setting up mobile pressure rooms for testing will also incur unnecessary costs.
The paperless approach
In this digital age, IMAs are widely available. An IMA is a cross-platform messaging and voice mobile application that is user-friendly, highly intuitive, and available without additional cost to end-users. Some IMAs even provide a business extension to facilitate efficient communication with customers. Therefore, IMAs are a revolutionary tool to replace a conventional phone call or email. For privacy protection, registration is secured through a separate online registration platform. The paperless approach also has numerous other advantages. The system is environmentally friendly and helps reduce the risk of fomite-mediated transmission.
Limitations and areas for improvement
The transmission of COVID-19 began slowly, almost imperceptibly. In a short time, however, the number of transmissions escalated dramatically and overwhelmed health-care services globally. Although paperless DT screening is a successful practical option to facilitate screening during a pandemic, potential limitations are identifiable. (Table 1 ) outlines these limitations with corresponding solutions.
Table 1.
Limitation and potential solution for drive-through (DT) screening.
| Limitation | Potential solution |
|---|---|
| System | |
| - Limitations in diagnostic capability (symptoms are not disease-specific) | - Using multi vital sign–based remote sensing to identify those requiring further assessment.9 |
| - Advise to return for assessment if screening is negative and the testee remains symptomatic | |
| - Non-flexible screening time (unavailable after office hours) | - Consider extending DT screening hours with the availability of workforce and resources |
| - Standardized screening protocols to streamline workflow | |
| - Breakdown in communication using IMA (language barrier with non-English users) | - Consider providing information in other commonly spoken languages (based on local population) |
| - Fatigue in healthcare staff (excessive workload in PPE) | - Increase workforce and resources |
| - Encourage taking more frequent breaks when the situation permits10 | |
| Testee/patient | |
| - Limited to individuals with a vehicle or a valid driving license | - Consider extending DT screening (with appropriate modification to the DT area) to cater for individuals on motorcycle or bicycle |
| - Increase resources | |
| - Screening not done for an underage individuals | - Walk-in screening for underage individuals (accompanied by a guardian) |
| - Limited to one person per vehicle (vehicle: self-contained compartment) | - Consider utilizing vehicles with larger capacity to ferry testees to DT screening |
| - Testees maintain social distance while in vehicle | |
| - Requiring special prearrangement with the DT screening center | |
| - Nonpunctual individuals may affect flow of screening process | - Consider sending reminders through instant messaging to testee 24 and 4 h before the appointment |
| Other | |
| - Change in weather (e.g., heavy rain or storm) | - Reschedule DT screening appointments via instant messaging |
| - Unfamiliarity with screening area | - Improve signage |
| - Increase the number of traffic wardens | |
Summary
The resilience of the global health system has been tested during the COVID-19 crises. Digital technology enhances the overall efficiency of DT screening and can assist in coping with the abrupt surge of patients during a pandemic. The framework of this system can be modified and tailored for outbreaks in other countries.
Declaration of Competing Interest
The authors declare no conflict of interests.
References
- 1.Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2020. Critical preparedness , readiness and response actions for COVID-19. (March):1–3. [Google Scholar]
- 3.Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020;369(April):m1375. doi: 10.1136/bmj.m1375. Available from: [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . 2020. Laboratory testing strategy recommendations for COVID-19. (March):6. [Google Scholar]
- 5.Weiss E.A., Ngo J., Gilbert G.H., Quinn J.V. Drive-through medicine: a novel proposal for rapid evaluation of patients during an influenza pandemic. Ann Emerg Med. 2010;55(3):268–273. doi: 10.1016/j.annemergmed.2009.11.025. Available from: [DOI] [PubMed] [Google Scholar]
- 6.Kwon K.T., Ko J.H., Shin H., Sung M., Kim J.Y. Drive-through screening center for covid-19: a safe and efficient screening system against massive community outbreak. J Kor Med Sci. 2020;35(11):2–5. doi: 10.3346/jkms.2020.35.e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO . World Health Organization; Geneva: 2020. Rational use of personal protective equipment for coronavirus disease (COVID-19): interim guidance.https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf (March):Accessed 23rd Mar 2020. Available from: [Google Scholar]
- 8.Liu S., Hobgood C., Brice J.H. Impact of critical bed status on emergency department patient flow and overcrowding. Acad Emerg Med. 2003;10(4):382–385. doi: 10.1111/j.1553-2712.2003.tb01353.x. [DOI] [PubMed] [Google Scholar]
- 9.Sun G., Nakayama Y., Dagdanpurev S., Abe S., Nishimura H., Kirimoto T. Remote sensing of multiple vital signs using a CMOS camera-equipped infrared thermography system and its clinical application in rapidly screening patients with suspected infectious diseases. Int J Infect Dis. 2017;55(January):113–117. doi: 10.1016/j.ijid.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radonovich L.J., Cheng J., Shenal B.V., Hodgson M., Bender B.S. Respirator Tolerance in health care workers. JAMA. 2009;301(1):36–38. doi: 10.1001/jama.2008.894. Available from: [DOI] [PubMed] [Google Scholar]