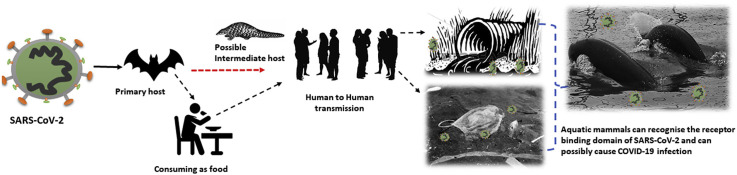
Graphical abstract
Highlights
-
•
The SARS-CoV-2 can enter the oceans, rivers, and lakes in several ways.
-
•
Aquatic mammals can recognise the receptor binding domain of SARS-CoV-2.
-
•
Cetacean species should be screened and monitored for the virus during a pandemic.
The ongoing newly emerged and highly infectious coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) started from the Huanan seafood market located in Wuhan, China at the end of December 2019 (Khan et al., 2020a). The primary source for the SARS-CoV-2 is reported as a bat because it constitutes approximately, 31% of their virome as coronaviruses (CoVs), however, the intermediate host is not clear, still, some studies reported pangolin, snake, and turtles as possible intermediate hosts (Allocati et al., 2016; Nabi et al., 2020; Wong et al., 2020; Ji et al., 2020; Liu et al., 2020). As of April 20, 2020, the pandemic has infected more than 2.4 million individuals and killed more than 165, 150 individuals globally (Walker, 2020). The pandemic has created health emergency, fear, and anxiety among global communities, and fighting against the COVID-19 aggressively (Khan et al., 2020b). The question what if the SARS-CoV-2 jump from human to wild animal species which then become reservoirs, affect the wildlife, and visit us in the near future has started a hot debate in the scientific community. As a result, several terrestrial animals were screened. A study by Shi et al. (2020) found that SARS-CoV-2 transmitted via droplet efficiently replicate in cats and ferrets, but poorly in ducks, chickens, pigs, and dogs. Recently, SARS-CoV-2 was detected in a tiger at the Bronx Zoo (Calma, 2020). What if other mammals, especially aquatic mammals can host SARS-CoV-2 need experimental verification. However, the Angiotensin-converting enzyme 2 (ACE2), a receptor for SARS-CoV-2 binding found in aquatic mammals can increase the vulnerability to SARS-CoV-2 infection (Luan et al., 2020).
The coronavirus subfamily; Coronavirinae is divided into four genera, alpha-, beta-, gamma-, and delta (α, β, γ, and δ) coronavirus. The α and β coronaviruses infect multiple species of mammals including humans, γ coronaviruses are found in birds and aquatic mammals including bottlenose dolphin and beluga whale, while δ coronaviruses are found both in birds and mammals including pigs (Durães-Carvalho et al., 2015; Miłek and Blicharz-Domańska, 2018). There are reports that α coronaviruses could also infect harbor seals (Schütze, 2016). The β coronavirus (SARS-CoV-2) bind to the host ACE2 through its receptor-binding domain (RBD) and regulate both human-to-human and cross-species transmissions of SARS-CoV-2 (Wan et al., 2020). Comparing the key amino acids in ACE2 for the binding ability to RBD in different species, ACE2 proteins from Cetacea, Primates, Cricetidae, and Bovidae were found capable to recognise RBD of SARS-CoV-2 by sustaining most of the key residues in ACE2 to connect with the SARS-CoV-2 RBD (Luan et al., 2020). This analysis indicates the vulnerability of aquatic mammals to COVID-19 infection.
The SARS-CoV-2 can survive on surgical masks and other plastic materials for several days (Chin et al., 2020). The ongoing COVID-19 pandemic has increased the demands for masks and gloves, which have been found floating in the open waters after disposal (Boyle, 2020). Globally, these protective covering as marine debris can introduce the SARS-CoV-2 from human to aquatic mammals. Furthermore, SARS-CoV-2 via stools can enter into the sewage system and survive for several days (Wu et al., 2020). The sewage especially in developing countries directly go to the ocean without treatment and can transmit the virus to the ocean. Cetaceans establish herd and migrate to long-distance beyond the political and geographical boundaries (Van Bressem et al., 2014). These characteristics can increase the chances of an outbreak if the highly infectious SARS-CoV-2 is introduced in their communities.
Although investigations are required, however, SARS-CoV-2 can possibly cause infection in marine mammals. Based on the literature, ample evidence is provided in several marine mammals which shows the devastating effects of pneumonia. Viral pneumonia and respiratory infection have been reported to cause deaths in a number of marine mammals including; mass mortalities of the seal at Orkney in 1813, 1836, and 1869–70 (McConnell, 1985), deaths of at least 1000 common seals during 1918 in Iceland (Dietz et al., 1989), death of 445 harbor seals along the New England seaboard in the United States during 1979–1980 (Geraci et al., 1982, 1984), and the death of 28 harbor porpoises died between 1990 and 1995 on the coasts of England and Wales (Kirkwood et al., 1997). Moreover, morbillivirus had also been linked with deaths of several mammals, for instance, the death of approximately, 18000 harbor seals (Phocavitulina L) in the North Sea and Baltic Sea in 1988 (Heide-Jorgensen et al., 1992), death of thousands of Baikal seals (Phocasibirica) in the Soviet Union in 1987 (Grachev et al., 1989; Osterhaus et al., 1989), and mass deaths of striped dolphins (Stenellacoeruleoalba) in the Mediterranean Sea (Lipscomb et al., 1996) and Spanish Mediterranean in 1990 (Duignan et al., 1992). Furthermore, in 2007, there was a recurrence of the virus which affected over 100 striped dolphins (Raga et al., 2008) and 60 long-finned pilot whales (Globicephala melas) (Fernandez et al., 2008). Nonetheless, pneumonia which can be caused by viruses or bacteria is the leading cause of death in dolphins throughout the world (Rubio-Guerri et al., 2013).
In summary, there is a need to increase surveillance on cetaceans and screen the individuals for COVID-19 infection if there is mass stranding or unusual behaviour. Special attention is required to the critically endangered, endangered, and other vulnerable populations. Further studies are needed in cetaceans to provide deeper insight into host specificity, as they are exposed continuously to escalating anthropogenic stressors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Ghulam Nabi, Email: ghulamnabiqau@gmail.com.
Suliman Khan, Email: Suliman.khan18@mails.ucas.ac.cn.
References
- Allocati N., Petrucci A.G., Giovanni P.D. Bat-man disease transmission: zoonotic pathogens from wildlife reservoirs to human populations. Cell Death Dis. 2016;2:16048. doi: 10.1038/cddiscovery.2016.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle L. Discarded coronavirus face masks and gloves rising threat to ocean life, conservationists warn. 2020. https://www.independent.co.uk/news/coronavirus-masks-gloves-oceans-pollution-waste-a9469471.html Independent.
- Calma J. Tigers (and other cats) can catch the coronavirus. The Verge. 2020. https://www.theverge.com/2020/4/6/21211217/pets-cats-tigers-bronx-zoo-covid-19-coronavirus
- Chin A.W.H., Chu J.T.S., Perera M.R.A. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microb. 2020 doi: 10.1016/s2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz R., Heide-Iargensen M.P., Harkonen T. Mass deaths of harbor seals (Phoca vitulina) in Europe. Ambio18. 1989:258–264. [Google Scholar]
- Duignan P.J., Geraci J.R., Raga J.A. Pathology of morbillivirus infection in striped dolphins (Stenella coeruleoalba) from Valencia and Murcia. Spain. Can. J. Vet. Res. 1992;56:242–248. [PMC free article] [PubMed] [Google Scholar]
- Durães-Carvalho R., Caserta L.C., Barnabé A.C. Coronaviruses detected in Brazilian wild birds reveal close evolutionary relationships with beta- and deltacoronaviruses isolated from mammals. J. Mol. Evol. 2015;81:21–23. doi: 10.1007/s00239-015-9693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez A., Esperon F., Herraez P. Morbillivirus and pilot whale deaths, Mediterranean Sea. Emerg. Infect. Dis. 2008;14:792–794. doi: 10.3201/eid1405.070948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraci J.R., St Aubin D.J., Barker I.K. Mass mortality of harbor seals: pneumonia associated with influenza A virus. Science. 1982;215:1129–1131. doi: 10.1126/science.7063847. [DOI] [PubMed] [Google Scholar]
- Geraci J.R., StAubin J., Barker I.K. Susceptibility of grey (Halichoerus grypus) and harp (Phoca groenlandica) seals to the influenza virus and Mycoplasma of epizootic pneumonia of harbor seals (Phoca vitulina) Can. J. Fish. Aquat. Sci. 1984;41:151–156. [Google Scholar]
- Grachev M.A., Kumarev V.P., Mamaev L.V. Distemper in baikal seals. Nature. 1989;338:209–210. doi: 10.1038/338209a0. [DOI] [PubMed] [Google Scholar]
- Heide-Jorgensen M.P., Harkonen T., Dietz R. Retrospective of the 1988 European seal epizootic. Dis. Aquat. Org. 1992;13:37–62. [Google Scholar]
- Ji W., Wang W., Zhao X. Cross‐species transmission of the newly identified coronavirus 2019‐nCoV. J. Med. Virol. 2020;92:433‐440. doi: 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S., Siddique R., Shereen M.A. The emergence of a novel coronavirus (SARS-CoV-2), their biology and therapeutic options. J. Clin. Microbiol. 2020 doi: 10.1128/JCM.00187-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S., Siddique R., Ali A. The spread of novel coronavirus has created an alarming situation worldwide. J. Infect. Public Health. 2020;13:469–471. doi: 10.1016/j.jiph.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkwood J.K., Bennett P.M., Jepson P.D. Entanglement in fishing gear and other causes of death in cetaceans stranded on the coasts of England and Wales. Vet. Rec. 1997;141:94–98. doi: 10.1136/vr.141.4.94. [DOI] [PubMed] [Google Scholar]
- Lipscomb T.P., Kennedy S., Moffett D. Morbilliviral epizootic in bottlenose dolphins of the Gulf of Mexico. J. Vet. Diagn. Invest. 1996;8:283–290. doi: 10.1177/104063879600800302. [DOI] [PubMed] [Google Scholar]
- Liu Z., Xiao X., Wei X. Composition and divergence of coronavirus spike proteins and host ACE2 receptors predict potential intermediate hosts of SARS-CoV-2. J. Med. Virol. 2020 doi: 10.1002/jmv.25726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luan J., Jin X., Lu Y. SARS-CoV-2 spike protein favors ACE2 from Bovidae and Cricetidae. J. Med. Virol. 2020 doi: 10.1002/jmv.25817. 10.1002/jmv.25817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell B.J. Seals in Orkney. Proc. R. Soc. Edinburgh Sect. 1985;87B:95. l 04. [Google Scholar]
- Miłek J., Blicharz-Domańska K. Coronaviruses in avian species - review with focus on epidemiology and diagnosis in wild birds. J. Vet. Res. 2018;62:249–255. doi: 10.2478/jvetres-2018-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi G., Siddique R., Ali A. Preventing bat-born viral outbreaks in future using ecological interventions. Environ. Res. 2020;185:109460. doi: 10.1016/j.envres.2020.109460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterhaus A.D.M.E., Groen J., UytdeHaag F.G.C.M. Distemper virus in Baikal seals. Nature. 1989;338:209–210. doi: 10.1038/338209a0. [DOI] [PubMed] [Google Scholar]
- Raga J.A., Banyard A., Domingo M. Dolphin morbillivirus epizootic resurgence, Mediterranean Sea. Emerg. Infect. Dis. 2008;14:471–473. doi: 10.3201/eid1403.071230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Guerri C., Melero M., Esperón F. Unusual striped dolphin mass mortality episode related to cetacean morbillivirus in the Spanish Mediterranean Sea. BMC Vet. Res. 2013;9:106. doi: 10.1186/1746-6148-9-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schütze H. Coronaviruses in aquatic organisms. Aquacult. Virol. 2016:327–335. [Google Scholar]
- Shi J., Wen Z., Zhong G. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020 doi: 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Bressem M.F., Duignan P.J., Banyard A. Cetacean morbillivirus: current knowledge and future directions. Viruses. 2014;6:5145–5181. doi: 10.3390/v6125145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker M. Track the coronavirus outbreak on Johns Hopkins live dashboard. Medpage Today. 2020. https://www.medpagetoday.com/infectiousdisease/publichealth/84698
- Wan Y., Shang J., Graham R. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 2020;94 doi: 10.1128/JVI.00127-20. e00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M.C., Cregeen S.J.J., Ajami N.J. Evidence of recombination in coronaviruses implicating pangolin origins of nCoV‐2019. bioRxiv. 2020. [DOI]
- Wu Y., Guo C., Tang L. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]