Abstract
BACKGROUND:
Hospitals in developed countries allocate itself about 40% of health-care costs and in developing countries up to 80%. In this study, researchers reviewed the related article in the field of the hospitals' performance evaluation due to the identification of common indicators used in different models with the aim of providing simple list for evaluating hospitals' performance to the researchers who are interested to these issues.
METHODS:
The databases for the search included Medline, Google Scholar, and Scopus. A search strategy leads to the extraction of 403 related articles that after the removal of inappropriate and duplicate articles, 42 studies were selected for the scoping review.
RESULTS:
This scoping review showed that 9 of 42 selected articles use data envelopment analysis model, 6 of them Pabon Lasso model, 3 of them balanced scorecard, 3 of them organizational excellence model, and the remaining articles used key performance indicators to evaluate hospital performance. A process approach was used to categorize the common indicators because the literature review indicated that common indicators mainly evaluate data, process, output, or impact of performance. The findings included 36 input, 39 process, 27 output, and 8 impact common indicators for evaluating performance.
DISCUSSION:
This scoping review of related literature indicated that despite differentiation in the time and place of past studies in the field of performance evaluation models, there are some indicators that are common in most popular performance evaluation models. These simple lists can apply for evaluation of hospitals' performance instead of complicated models.
Keywords: Evaluation, hospital, performance
Introduction
In developed countries, hospitals allocate about 40% and in developing countries up to 80% of health-care costs. Therefore, the results of hospitals' performance in the health-care system are a great priority.[1]
On the other hand, based on the literature review, more than half of national health resources are wasted in different countries, especially in underdeveloped countries, which means limited resources are inefficiently consumed or national income is spent on services that are not proportionate and effective. Therefore, ensuring the quality of health-care services requires evaluating the performance of health-care organizations to alleviate some of the government's financial problems by minimizing waste.[2] Therefore, many health-care providers have stepped to path of performance evaluation in order to achieve their goals and missions.[3]
In fact, these organizations consider performance evaluation models as a way to move toward continuous improvement and valid tool for measuring of the organization's current performance.[4]
On the other hand, an appropriate and applicable evaluation model for hospital performance potentially would lead to more accountability, service quality, and satisfied customer. When a hospital's performance is not evaluated, any claims about its service quality will be unproven, and there is no evidence to improve performance. Therefore, the evaluation and improvement of performance are two sides of the same coin that will lead to continued improvement, and the lack of an efficient performance evaluation will lead to serious problems for hospitals from the aspect of responsibility and performance improvement. Until two decades ago, designing a performance evaluation system was just a mere innovation, but today, it has become an indispensable necessity for any organization. With all these interpretations, the evaluation of performance is very complex and difficult to done, which requires pay attention to all various dimensions of performance that would affect the job results.[5]
The WHO's definition of performance is achieving the desired goals. The excellent hospital performance should be based on professional competence in benefit from the latest knowledge, advanced technology and of course regarding available resources, efficiency of resource, minimum risk for patient, and patient satisfaction. In other words, according to literature review, the performance evaluation is not worthwhile alone and will be valuable if the results of that used to continually improvement of performance.[6]
Today, several models to evaluate the performance of an organization have been introduced such as models of organizational excellence (European Foundation for Quality Management) that evaluates the performance of organizations for establishing total quality management[7] or the balanced scorecard (BSC) approach that transforms the organization's strategic goals into measurable indicators and establishes a balanced distribution across the organization's critical areas. This approach, as a measurement system while operationalizing the organization's vision and strategies, can provide a comprehensive picture of the organization's performance. In other words, a balanced scorecard can play an effective role in realizing the vision and strategy of an organization using a set of financial and nonfinancial indicators.[8]
Other ways to evaluate hospitals' performance are the use of key performance indicators (KPIs). In some studies, the performance of hospitals was evaluated by identifying and measuring KPIs.[9]
Organizations that apply any evaluation's models to measure its performance at first should identify some of the effective indicators. Improving hospital indicators means efficiency and effectiveness in hospital activities, in other words, best use of resources.[10] So far, many studies have been conducted to evaluate the performance of hospitals in different countries. In this study, we have attempted a scoping review of studies carried out over the past 10 years (2018–2008) on the performance evaluation of hospitals using different methods in Iran and other countries to reach common evaluation indicators.
Methods
In recent years, many studies have been conducted to evaluate the performance of health-care organizations in different countries. Therefore, because of the large number of studies in this field, the search strategy limited to the 10-year period (2008–2018). Furthermore, with regard to the purpose of the study, which was a scoping review of studies conducted in the field of hospital performance, the researchers excluded studies that done in other health-care organizations. Therefore, the keywords used to search the related articles were as follows: Performance Evaluation, Hospital, Performance Evaluation Models, and Performance Evaluation Methods [Table 1].
Table 1.
Search strategy
| SPIDER tool[1] | Search term |
|---|---|
| S | Hospital* OR clinic* OR hospice* OR (health AND organization OR center) |
| PI | Assessment*OR evaluation* OR appraisal* AND (performance*OR function AND operation) AND efficiency* |
| D/E/R | “Qualitative” OR “quantitative” OR “mixed method*” OR “case study” OR “cohort study” OR “quality assurance” |
*=When some words are incomplete
The databases used for the search included Medline, Google Scholar, Scopus, EBSCO Discovery Service, and Web of Science [Table 2]. A search of these databases leads to the extraction of 403 articles that, after the removal of duplicate and non-English articles, 123 articles with screening criteria (keywords in the title or abstract of the articles) were selected. Furthermore, in order to focus on the main purpose of the study, literature that evaluated the results of performance evaluation without using a specific model were excluded. After rescreening, studies that were repeated in the EndNote X7 for windows because of the use of the snowball method in references also were excluded. Finally, 42 studies were extracted for the scoping review [Figure 1].
Table 2.
Inclusion and exclusion criteria
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Time period | January 2007 and February 2017 | Any study outside these dates |
| language | English and Persian | Non-English |
| Kind of organization | Hospitals and health centers and health-care organization | No reference to l health care organization |
| Tool | DEA, BSC, EFQM, Pabon Lasso, lean, JCAH, accreditation standard | Any study without this method |
| Population and sample | All kind of health-care organization (clinical and nonclinical) | Nonhealth-care organization |
DEA=Data envelopment analysis, BSC=Balanced scorecard, EFQM=European Foundation for Quality Management, JCAH=Joint Commission on Accreditation of Healthcare
Figure 1.
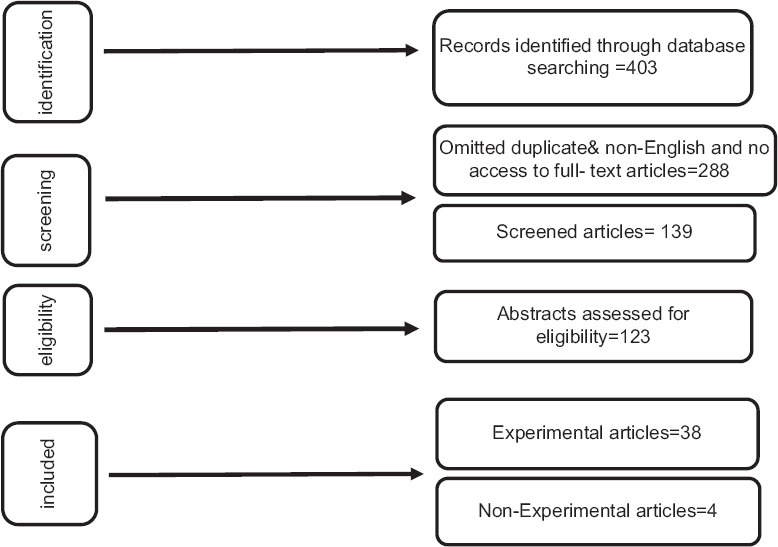
Screening process of articles
After the final review of extracted articles, the selected articles were reviewed using the matrix method – a system for organizing, critically evaluating, and synthesizing research articles for scientific review of articles. Inclusion criteria were also used for reviewing and evaluating relevance articles. A scoping review is done to attain to deep perspective of a selected topic, not to evaluate or criticize the best study that have been counducted. Therefore, the studies were reviewed by a researcher, away from any critical review and weighting of the studies.
Results
After screening the studies, 42 studies that met the inclusion criteria were carefully reviewed. The characteristics of these studies are summarized in Table 3 by target population, study location, research method, and time of study.
Table 3.
Descriptive of reviewed articles
| Descriptive variable | n (%) |
|---|---|
| Place | |
| Hospital | 39 (93) |
| Other health-care organizations | 3 (7) |
| Country | |
| USA | 10 (24) |
| Asia | 26 (62) |
| Africa | 1 (2) |
| Europe | 5 (12) |
| Method | |
| Qualitative | 4 (10) |
| Quantitative | 38 (90) |
| Time | |
| Before 2010 | 6 (14) |
| After 2010 | 36 (86) |
Out of 42 selected articles, 18 were published in other countries [Table 4] and 24 in Iran [Table 5], 9 of them use data envelopment analysis,[2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17]6 of them Pabon Lasso model,[8,18,19,20,21,22]3 of them BSC,[23,24,25]3 of them organizational excellence model,[4,7,26]3 of them used accreditation standards,[27,28,29] and other articles used KPIs to evaluate hospital performance.[1,30,31,32,33,34,35,36,37,38,39,40,41,42] The Pabon Lasso model was used for the evaluation of hospital performance only in Iran in determined time period. In two studies, combined models were used for performance evaluation, and in some studies, performance evaluation indicators have been used; these indicators were hospital mortality rates and readmission rates as performance evaluation indicators.
Table 4.
Descriptive of English reviewed articles
| Authors | Country | Years | Performance assessment method |
|---|---|---|---|
| Dong et al. | China | 2017 | DEA: Systematic review |
| Karsak et al. | Istanbul | 2017 | DEA |
| Glover et al. | USA | 2015 | Social media |
| Lacko et al. | Slovakia | 2014 | DEA |
| Ash et al. | USA | 2012 | Statistical issues |
| Baradach et al. | USA | 2012 | Commercial website |
| Stephan et al. | USA | 2012 | Readmission rate |
| Renzi et al. | Italia | 2012 | Quality indicators |
| Grigorodis et al. | Greece | 2011 | BSC |
| Stephen et al. | USA | 2011 | JCAH |
| Chung et al. | Taiwan | 2010 | DEA |
| Yawe et al. | Uganda | 2010 | DEA |
| Abujudeh et al. | USA | 2010 | KPI |
| Weng et al. | USA | 2009 | DEA |
| Kneenan et al. | USA | 2008 | Readmission rate |
| Derrigo et al. | Italia | 2008 | Empirically derived model and euroscore system |
| Werner et al. | USA | 2007 | Mortality rate |
| Jha et al. | USA | 2007 | Mortality rate |
DEA=Data envelopment analysis, BSC=Balanced scorecard, JCAH=Joint Commission on Accreditation of Healthcare, KPI=Key performance indicator
Table 5.
Descriptive of Persian reviewed articles
| Authors | Years | Performance assessment method |
|---|---|---|
| Saeedi et al. | 2018 | Lean |
| Barati et al. | 2017 | Pabon Lasso |
| Jahangiri et al. | 2017 | MADM |
| Rajouee et al. | 2017 | AHP + BSC |
| Alinezhad et al. | 2017 | BSC + VFB-DEA |
| Omidvari et al. | 2016 | FANP + BSC |
| Dargahi et al. | 2016 | Pabon Lasso |
| Bastani et al. | 2016 | Pabon Lasso |
| Khanzadeh et al. | 2015 | EFQM |
| Arzemani et al. | 2014 | Accreditation standards |
| Tabatabaee et al. | 2013 | EFQM |
| Raeesi et al. | 2013 | Standard of ministry |
| Rahbar et al. | 2013 | Pabon Lasso |
| Azar et al. | 2013 | LINMAP + SAW + HBSC |
| Azar et al. | 2013 | DEA |
| Parham et al. | 2013 | EFQM |
| Bahadori et al. | 2012 | Systematic review |
| Khani et al. | 2012 | DEA |
| Samadi et al. | 2012 | BSC |
| Janati et al. | 2012 | Expert consensus |
| Bahadori et al. | 2011 | Pabon Lasso model |
| Sheikhzadeh et al. | 2010 | Delphi |
| Asadi et al. | 2010 | DEA + BSC + SERVQUAL |
| Sajadi | 2009 | Pabon Lasso |
BSC=Balanced scorecard, DEA=Data envelopment analysis, EFQM=European Foundation for Quality Management, SAW=Simple additive weighting, HBSC=Hierarchical Balanced Scorecard AHP=Analytical Hierarchy process, MADM=Multi Attribute Decision Making, VFB=Virtual Frontier Benevolent, FANP=Fuzzy Analytic Network Process, LINMAP=Linear Programming for Multidimensional Analysis of Preferences, SERVQUAL=Scale for measuring service quality
After reviewing the indicators used in hospitals' performance evaluation-related literature review, a process approach was used to categorize the common indicators in most applied performance evaluation models because the literature review indicated that common indicators are main kind of indicators to evaluate data, process, output, and impact of performance. This category is summarized in Table 5.
Discussion
Much has been echoed in the literature about the importance of understanding performance. According to industrial models of production, where the efficiency of production is paramount, some researchers have proposed that health care could be viewed under the same magnifying glass as the production of other goods.
Nevertheless, in many countries, the hospital environment has completely changed in the past 20 years compared to industrial zone, so health-care organizations have been forced to apply continued performance improvement approaches to survive in competitive environment. Therefore, seeking to comprehensive, reliable, strategic, and flexible model to evaluate performance has become an important priority and an undeniable responsibility for them. As mentioned above, health-care management and health-care industry have been one of the popular and complex topics that many researchers and professionals have focused on. In this study, researchers reviewed studies conducted over 10 years (2007–2017) with the aim of extracted common indicators of evaluating hospital performance.
For as much as in hospitals such as other organizations, services are delivered through determined processes and the researchers decided to summarize and categorize the common indicators in the format of process components (data, process, output, and impact) [Table 6]. In the articles reviewed, different indicators were used in varied model applied for hospitals' evaluation, but a scoping review confirms this point that despite difference among performance evaluation models, common indicators are the main body of all reviewed models.
Table 6.
Effective indicators on hospital performance evaluation in a process format
| Input | Process | Output | Impact |
|---|---|---|---|
| Number of inpatient beds | Number of hospitalization days | Number of deaths after admission | Patient satisfaction |
| Number of outpatient beds | Number of emergency visits to outpatient visits | Incidence of nosocomial infections | Relocation of staff |
| Number of physicians | Proportion of patients who have to use expensive medical equipment to total patients | Percentage of agreement between diagnosis at the time of admission and at discharge | Absence of staff |
| Number of nurses | Hospital survival rate | Number of outpatient deaths | Employee sick leave rates |
| Number of other clinical team staff | Combined index of hospitalization adjusted days | Number of deaths after surgery | Hospital success in obtaining credentials in quality management |
| Total number of employees equivalent to full time | Total number of nonemergency outpatient visits | Percentage of readmission for the same diagnosis | Legal complaint rate from the hospital during the year |
| Cost of human resources | Number of outpatient visits | Percentage of repeat surgical procedures | Staff satisfaction percentage |
| Cost of other resources | Number of emergency patients | The number of falling patients | Complaint patient percentage |
| Ratio of the number of administrative staff to total staff | Number of correct diagnoses to total diagnoses to each specialist | Percentage of medical errors | |
| The ratio of physician to nurse | Number of patients refer to hospital to admitted patients | Percentage of postoperative hematomas and hemorrhages | |
| Ratio of physicians to bed | Number of patients admitted per day | Mortality rate in intensive care unit | |
| Ratio of nurses to bed | Number of minor surgeries | Needlestick | |
| Ratio of other members of clinical team to bed | Number of major surgeries | Unplanned readmissions to the intensive care unit within 48 h after discharge | |
| The ratio of the number of employees to the number of active beds | Patient admitted ratio | Prevalence of smoking among staff | |
| Day-case rates | The ratio of perfect nursing documentation | Readmission rate per active bed | |
| The ratio of staff to existing standards | Number of hours of nursing courses | Percentage of costs due to medical neglect | |
| The ratio of managers’ salaries to the total cost of human resources | Ratio of appropriate prescriptions to total prescriptions | Error percentage in estimating bills correctly | |
| Gross margin | Rate of clinical chemistry, hematology, immunology, and bacteriology tests | Number of readmissions based on different diagnoses | |
| Clothing and appearance of staff | Average cost of outpatient | Hospital medical expenses relative to total hospital costs | |
| Parking for patients’ relatives and acquaintances | Average cost of inpatient | Ratio of private income to total hospital costs | |
| Prescription rate of diagnostic procedures | Average costs per bed per day | Sentinel event rate | |
| Staff salary and benefits | Hand hygiene practices (measurement of alcohol) | Total rejected (total number of bills rejected by insurance) | |
| Debtors | Percentage of patients with long stay | The rate of false-positive and false-negative tests | |
| Quality of medical equipment | Average waiting time for outpatient admission | The rate of canceled surgeries | |
| Hospital safety | Operating expense per bed | Total number of radiologic tests per number of beds | |
| The reputation of the hospital | Duration of unused equipment | Medical error rates per 10,000 outpatients | |
| Wellness facilities for patient families and visitors | Number of articles published in peer-reviewed scientific journals by staff per year | Compensation rate as a percentage of total revenue | |
| On-call physicians | Occupied day per bed | ||
| Patient safety culture | Inpatient bed days per physician | ||
| Costs of staff training per capita | BOR | ||
| Percentage of staff with postgraduate degrees | BTR | ||
| Percentage of physicians’ referrals to other specialists | Waiting time for admitted in the emergency department | ||
| Ratio of total staff costs (salaries and benefits of staff) to total hospital revenue | ALS | ||
| Average overtime per employee | Waiting time for admitted in the emergency department | ||
| Ratio of assets to debt | ALS | ||
| Food quality | Time and circulation of visits | ||
| The relevance of the tests prescribed to the diagnosed disease | |||
| Physicians’ tolerance to hear details of patients’ problems | |||
| Respectfully treat of all staff | |||
| Number of discharge with personal consent |
BOR=Bed occupancy rate, BTR=Bed turnover ratio, ALS=Average length of stay
Therefore, the researchers in this study tried to gather indicators that were mainly used in previous related literature to evaluate the performance of hospitals to guide the practice of those interested in this kind of topics.
Study novelty
In this study researchers tried to obtaining a simple but comprehensive list of indicators that commonly used for hospital performance evaluation instead of complex performance evaluation models.
Study limitation
Researchers in this study tried to extracted related articles but some of them were not available because of publisher or journal rules so, researchers for overcoming this limitation replaced the most similar ones.
Financial support and sponsorship
This article is the part of the first author thesis that financial by grant number IUMS/SHMIS-1395/9221532202
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
this research was part of Ph.D. thesis of the first author that was financially supported by grant number IUMS/SHMIS-1395.9221532202.
References
- 1.Adel A, Mohammadi Y. Designing a math model for hospital performance evaluation with the FHNBSC, SAW, and LINMAP integrated approach. [Last accessed on 2019 Nov 20];Health Syst Res. 2012 10:509–24. Available from: http://magirancom/2322-5564 . [Google Scholar]
- 2.Adel A, Valipour M, Moghbel A, Hassas Y. Efficiency evaluation of Tehran university of medical sciences hospitals using data envelopment analysis (2011-2010) [Last accessed on 2019 Nov 20];Health Manage J. 2013 16:36–46. Available from:http://jha.iums.ac.ir/article-1-1305-fa.htm. [Google Scholar]
- 3.Asadi M, Mirghafouri H, Sadeghi Z, Kosravsniyan H. Evaluation of performance of Yazd public hospitals using a combination of balanced scorecard models, data envelopment analysis and servqual. [Last accessed on 2019 Nov 20];J Shahid Sadoughi Univ Med Sci Health Serv Yazd. 2010 18:559–69. Available from: http://jssussuacir/article-1-1335-fahtml . [Google Scholar]
- 4.Parham M, Fotouhi M, Jandaghi M, AlipourKh Evaluation of performance of Shahid Beheshti hospital in Qom based on organizational excellence model. [Last accessed on 2019 Nov 20];J Qom Univ Med Sci. 2014 7:79–85. Available from: http://journalmuqacir/article-1-598-fahtml . [Google Scholar]
- 5.Taslimi M, Zayandeh M. Challenges for creating a system for evaluating the performance of the hospital: A review of the literature and scientific work. [Last accessed on 2019 Nov 20];Hakim. 2014 16:35–41. Available from: http://hakimhbiir/article-1-1132-fahtml . [Google Scholar]
- 6.Khalilnezhad R, Barati O. Hspital performance evalouatio. [Last accessed on 2019 Nov 20];Health Manage. 2009 3:27–36. Available from: http://jhaiumsacir/article-1-166-fahtml . [Google Scholar]
- 7.Khanzadeh A, Motlagh M, Mirshakak A, Akbari N, Niyakan M, Pour shirvaniD. Evaluation of the performance of hospitals affiliated to Abadan faculty of medical sciences based on the Iranian national excellence award model. [Last accessed on 2019 Nov 20];Health Inf Manage. 2016 13:138–44. Available from: http://magirancom/p1563440 . [Google Scholar]
- 8.Dargahi H, Tolouee SH, Sadeghifar J. Evaluation of performance of hospitals affiliated with Tehran university of medical sciences using the Pabon Lasso model. [Last accessed on 2019 Nov 20];Payavard Health. 2017 10:290–8. Available from: http://payavardtumsacir/article-1-6068-fahtml . [Google Scholar]
- 9.Ghandehari N, Esmaeeliyan M, Teimouri H, Ghalamkari Sh. Evaluation of performance of Nour and Hazrat Ali Asghar hospitals in Isfahan using a balanced scorecard combination method and a technique for measuring attractiveness through a series of evaluations. [Last accessed on 2019 Nov 20];Health Inf Manage. 2017 14:58–64. Available from: http://magirancom/p1718495 . [Google Scholar]
- 10.Tripathi CB, Kumar R, Sharma RC, Agarwal R. Assessment of performance of services in a tertiary care neuropsychiatric institute using Pabon Lasso model. Asian J Med Sci. 2016;7:69–74. [Google Scholar]
- 11.Dong S, Zuo Y, Guo S, Li M, Liu X, Li H. Data envelopment analysis for relative efficiency measurements of Chinese hospitals: A systematic review. Res Health Sci. 2017;2:79–103. [Google Scholar]
- 12.Karsak EE, Karadayi MA. Imprecise DEA framework for evaluating health-care performance of districts. Kybernetes. 2017;46:706–27. [Google Scholar]
- 13.Hajduová RL. Using the data envelopment analysis in evaluating the technical efficiency in hospitals: General and new approaches. Acta Oecon Cassoviensia. 2014;19:144–58. [Google Scholar]
- 14.Chuang CL, Chang PC, Lin RH. An efficiency data envelopment analysis model reinforced by classification and regression tree for hospital performance evaluation. J Med Syst. 2011;35:1075–83. doi: 10.1007/s10916-010-9598-5. [DOI] [PubMed] [Google Scholar]
- 15.Yawe B. Hospital performance evaluation in Uganda: A super-efficiency data envelope analysis model. [Last accessed on 2019 Nov 20];Zambia Soc Sci J. 2010 1:6. Available from: http://scholarshiplawcornelledu/zssj/vol1/iss1/6 . [Google Scholar]
- 16.Weng SJ, Wu T, Blackhurst J, Mackulak G. An extended DEA model for hospital performance evaluation and improvement. Health Serv Outcomes Res Methodol. 2009;9:39. [Google Scholar]
- 17.Khani F, Naderi H, Zangeneh M, Fazeli E. Measuring the relative efficiency of Ilam hospitals using data envelopment analysis. Manage Sci Lett. 2012;2:1189–94. [Google Scholar]
- 18.Sajadi H, Sajadi Z, Hadi M. Is there a method for comparing key indicators of hospital performance. [Last accessed on 2019 Nov 20];Health Inf Manage. 2010 8:71–81. Available from: http://ensaniir/fa/article/262230 . [Google Scholar]
- 19.Rahbar A, Hadi P, Khosravi M. Evaluation of the performance of teaching hospitals in Qom and Kashan university of medical sciences and health services and their comparative comparison using the Pabonacci model. [Last accessed on 2019 Nov 20];Health Inf Manage. 2015 11:362–70. Available from: http://ensaniir/fa/article/353851 . [Google Scholar]
- 20.Bastani P, Lotfi F, Moradi M, Ahmadzadeh M. Performance analysis of educational hospitals of Shiraz university of medical sciences before and after delivery of the health system using the Pabon Lasso model. [Last accessed on 2019 Nov 20];J Rafsanjan Univ Med Sci. 2016 15:781–92. Available from: http://journalrumsacir/article-1-3165-fahtml . [Google Scholar]
- 21.Barati B, Farziyanpour F, Arab M, Rahimi A. Evaluation of the performance of Ninth and Deh Razi hospitals in Torbat Heydarieh city based on the Pabon Lasso model and its comparative comparison with the national standards in 1393-2014. [Last accessed on 2019 Nov 20];J Torbat E Heydarieh Univ Med Sci. 2017 5:48–55. Available from: http://jms.thums.ac.ir/article-1-430-fa.html . [Google Scholar]
- 22.Mohammadkarim B, Jamil S, Pejman H, Seyyed MH, Mostafa N. Combining multiple indicators to assess hospital performance in Iran using the Pabon Lasso model. Australas Med J. 2011;4:175–9. doi: 10.4066/AMJ.2011.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grigoroudis E, Orfanoudaki E, Zopounidis C. Strategic performance measurement in a healthcare organisation: A multiple criteria approach based on balanced scorecard. Omega. 2012;40:104–19. [Google Scholar]
- 24.Samadi S, Gholmohammadi A, Mohammadi A, Rezapour T. Designing an organizational performance evaluation model for NAJA hospitals. Entezami Med. 2011;1:38–45. [Google Scholar]
- 25.Rajoui M, Ramezan M, Hesari M, Bour bour M. Designing performance evaluation indicators by using AHP and BSC approaches (case of study: Social security organization of Mashhad) [Last accessed on 2019 Nov 20];Soc Welf Q. 2017 17:131–58. Available from: http://refahjuswracir/article-1-2867-fahtml . [Google Scholar]
- 26.Tabatabaee SS, Kalhor R, Yousefi S, Taghadum-Kangi S, Ghamari MR. Performance evaluation of mehr hospital in Mashhad, Iran, based on European foundation for quality management (EFQM) organizational excellence model. [Last accessed on 2019 Nov 20];Journal of Kerman School of Management and Medical Information. 2013 1:89–1. Available from: http://jmskmuacir/article-1-35-fahtml . [Google Scholar]
- 27.Stefan MS, Pekow PS, Nsa W, Priya A, Miller LE, Bratzler DW, et al. Hospital performance measures and 30-day readmission rates. J Gen Intern Med. 2013;28:377–85. doi: 10.1007/s11606-012-2229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arzemani M, Akaberi A, Pournaghi S. Performance evaluation of medical records department of hospitals related to North Khorasan university of medical sciences in 2013. [Last accessed on 2019 Nov 20];J North Khorasan Univ Med Sci. 2014 6:235–44. Available from: http://journalnkumsacir/article-1-338-fahtml . [Google Scholar]
- 29.Schmaltz SP, Williams SC, Chassin MR, Loeb JM, Wachter RM. Hospital performance trends on national quality measures and the association with joint commission accreditation. J Hosp Med. 2011;6:454–61. doi: 10.1002/jhm.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glover M, Khalilzadeh O, Choy G, Prabhakar AM, Pandharipande PV, Gazelle GS. Hospital evaluations by social media: A comparative analysis of facebook ratings among performance outliers. J Gen Intern Med. 2015;30:1440–6. doi: 10.1007/s11606-015-3236-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ash AS, Fienberg SF, Louis TA, Normand SL, Stukel TA, Utts J. Statistical issues in assessing hospital performance Committee of Presidents of Statistical Societies. 2012. [Last accessed on 2019 Nov 20]. Available from: https://escholarshipumassmededu/qhs_pp/1114 2012 .
- 32.Bardach NS, Asteria-Peñaloza R, Boscardin WJ, Dudley RA. The relationship between commercial website ratings and traditional hospital performance measures in the USA. BMJ Qual Saf. 2013;22:194–202. doi: 10.1136/bmjqs-2012-001360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keenan PS, Normand SL, Lin Z, Drye EE, Bhat KR, Ross JS, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 34.D'Errigo P, Seccareccia F, Rosato S, Manno V, Badoni G, Fusco D, et al. Comparison between an empirically derived model and the euroSCORE system in the evaluation of hospital performance: The example of the italian CABG outcome project. Eur J Cardiothorac Surg. 2008;33:325–33. doi: 10.1016/j.ejcts.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 35.Werner RM, Bradlow ET, Asch DA. Does hospital performance on process measures directly measure high quality care or is it a marker of unmeasured care? Health Serv Res. 2008;43:1464–84. doi: 10.1111/j.1475-6773.2007.00817.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jha AK, Orav EJ, Li Z, Epstein AM. The inverse relationship between mortality rates and performance in the hospital quality alliance measures. Health Aff (Millwood) 2007;26:1104–10. doi: 10.1377/hlthaff.26.4.1104. [DOI] [PubMed] [Google Scholar]
- 37.Shiekhzadeh R. Designing a model for evaluation and management of the health system of the country. [Last accessed on 2019 Nov 20];Management Research. 2010 3(10):83–108. Available from: http://ensaniir/fa/article/301140 . [Google Scholar]
- 38.Janati A, Dadgar E, Sadegh Tabrizi J, Asghari Jafarabadi M, GHolamzade Nikjoo R. Health system professionals, attitude towards necessary criteria for hospitals managers, performance assessment. [Last accessed on 2019 Nov 20];Sci Mag Yafte. 2012 14:91–101. Available from: http://yaftelumsacir/article-1-809-fahtml . [Google Scholar]
- 39.Bahadori M, Izadi AR, Ghardashi F, Ravangard R, Hosseini SM. The evaluation of hospital performance in Iran: A systematic review article. Iran J Public Health. 2016;45:855–66. [PMC free article] [PubMed] [Google Scholar]
- 40.Reisi-Nafchy M, Drees F, Mirzaeian RR. Assessment of performance indicators in hospitals university of medical sciences based on the standards of the ministry of health. [Last accessed on 2019 Nov 20];J Shahrekord Univ Med Sci. 2014 15:60–7. Available from: http://journalskumsacir/article-1-1931-fahtml . [Google Scholar]
- 41.Jahangiri A, Jahangiri M. Evaluation of hospital performance using multi-indicative decision making: A case study at Imam Khomeini social security hospital. [Last accessed on 2019 Nov 20];Arak Q J Health Manage. 2017 8:91–102. Available from: http://jhmsrbiauacir/article_10679html . [Google Scholar]
- 42.Saeedi Mehr M, Ghosi R, Emami G. Evaluating the urgency of emergency hospital based on lean principles. [Last accessed on 2019 Nov 20];Health Inf Manage. 2018 15:162–7. Available from: http://dxdoiorg/1022122/himv15i43554http://dxdoiorg/1022122/himv15i43554 . [Google Scholar]


