Abstract
Objectives
The study objective was to: (1) quantify symptom (pain) and crack changes during one year of follow-up, among teeth that had at least one visible crack at baseline but which did not receive treatment for those cracks; (2) identify any patient traits/behaviors and external tooth/crack characteristics correlated with these changes.
Methods
In this observational study, 209 National Dental Practice-Based Research Network dentists enrolled a convenience sample of 2,858 subjects, each with a single, vital posterior tooth with at least one observed external crack; 1,850 teeth remained untreated after one year of follow-up and were the cohort for analyses. Data were collected at the patient-, tooth-, and crack-level at baseline, one-year follow up (Y1), and interim visits. Associations between changes in symptoms and cracks were identified, as were changes in symptoms associated with baseline treatment recommendations.
Results
Changes in pain symptoms were observed in 32% of patients; decreases were twice as common as increases (23% vs.10%). More changes were observed in cold pain than in biting pain and spontaneous pain combined; 2% had increases in biting pain and 2% in spontaneous pain. Only 6% had an increase in the number of cracks. Changes in pain symptoms were not associated with an increase in the number of cracks, but were associated with baseline treatment recommendations. Specifically, pain symptom changes (especially decreases) were more common when the tooth was recommended for treatment at baseline.
Conclusions
Cracked teeth that have not received treatment one year after baseline do not show meaningful progression as measured by increased symptoms or number of cracks during follow-up.
Clinical Significance
Untreated cracked teeth, most of which were recommended for monitoring at baseline and some of which were recommended for treatment but did not receive treatment, remained relatively stable for one year with little progression of cracks or symptoms.
Keywords: practice-based research, cracked teeth
Introduction
The ideal course of action for teeth with cracks often presents a conundrum to dentists, ranging from monitoring to tooth extraction, depending upon the degree of pain and/or perceived severity of the crack system [1]. The issue may seem straightforward for teeth that demonstrate symptoms, since patient pain often dictates that some treatment be initiated to relieve distress. Even so, the best approach is often not obvious [1, 2].
The diagnosis of incomplete tooth fracture has been based axiomatically on tooth symptomatology: localized pain during chewing or biting, unexplained sensitivity to cold, and pain on release of pressure [3–13]. Besides the symptomatology described by the patient, the diagnosis of incomplete tooth fracture may be verified through a succession of procedures or tests performed by the clinician. Visual inspection, transillumination, staining [9,14,15], percussion, biting, thermal pulp tests (7,9,11], radiography [14,12], microscopy (14X-18X) (16], ultrasound [17], optical coherence tomography [18], quantitative light-induced fluorescence – QLF [19] and quantitative percussion diagnostics -QPD [20, 21, 22] all have been suggested as having the potential to detect cracks within tooth structure. However, incomplete tooth fracture may still be difficult to diagnose and may be a source of frustration for both the dentist and patient. To our knowledge, none of the different diagnostic procedures suggested have been tested in a controlled clinical study.
Asymptomatic teeth, which make up half or more of the population of cracked teeth, are an even greater diagnostic and treatment planning challenge [1]. The crucial yet controversial issue is to determine which teeth are more likely to “fail”, i.e., become symptomatic, fracture, have a crack extend to the pulp or down the root and require more-invasive and expensive treatment, and potentially even loss of the tooth.
There is limited evidence regarding the best way to identify risk factors for cracked teeth, as well as best practices for prevention, diagnosis, and treatment. Diverse therapies have been advocated and have shown some success, but these have mainly been based on a limited number of case reports and personal observations by clinicians [23,24]. However, due to the efforts of the Cracked Tooth Registry (CTR) study in the National Dental Practice-Based Research Network considerable research has gone into assessing correlations of patient-, tooth- and crack level characteristics to tooth symptoms, crack progression and tooth failure. The CTR represents the largest and most-comprehensive study of cracked teeth in history, and to date has provided significant insight into the associations between dentist-observable characteristics of teeth with cracks, and baseline symptoms and recommendations for treatment [25–28]. A significant strength of the CTR is that the patients will be followed for three years, providing much-needed longitudinal assessment of cracked teeth.
The study objective was to: (1) quantify symptom (pain) and crack changes during one year of follow-up, among teeth that had at least one visible crack at baseline but which did not receive any treatment for those cracks, and (2) identify any patient traits/behaviors and external tooth/crack characteristics correlated with these changes. Specifically, these objectives were achieved by determining 1) the proportion of teeth for which the number of cracks increased, 2) the proportion of teeth for which there were any changes in symptoms and the types of changes, and 3) the association of changes in symptoms with increases in cracks and with baseline treatment recommendations. The latter assesses the possible role that changes in symptoms (primarily decreases) may have had on whether treatment was performed on teeth originally recommended for treatment. The secondary objective was to identify patient-, tooth- and crack-level characteristics associated with increases in number of cracks and changes in symptoms at one year (Y1).
Methods
A previous publication detailed the study procedures, including enrollment and data collection [25]. In brief, the study used a convenience sample of subjects between 19 and 85 years old, each with at least one single, vital posterior tooth in which at least one external crack was clinically observed, who were enrolled by dentists in the National Dental Practice-Based Research Network [29]. Participating dentists selected and characterized one eligible cracked tooth in each subject. Each practice enrolled up to 20 eligible subjects, or as many as they could in eight weeks, whichever came first. The Institutional Review Board (IRB) of the lead investigators (TH & JF), as well as the various IRBs that oversee the six regions of the network, reviewed and approved the study. All patients provided informed consent prior to participating in study procedures. Patients were enrolled in two phases: first a pilot phase with 183 patients from 12 practices from April-July 2014, followed by a main launch phase that occurred from October 2014-April 2015.
A training manual developed and approved by study personnel and the lead investigators was used to train participating dentists and their designated practice personnel in data collection. A key element of the study was for dentists to determine what constituted a crack. Practitioners were asked to use the following definition: An obvious break of the external contiguous structure of the tooth, but involves no loss of tooth structure (e.g., lost cusp). Therefore, a crack had to be observable to be considered for entry into the study. Each crack on an enrolled tooth was documented on the case report form (CRF) by noting each surface using check boxes. In addition, the CRF included an odontogram in which each crack was depicted graphically. This data was then available at every recall so the dentist could evaluate the tooth for changes in crack number and surfaces.
Various patient-, tooth- and crack-level characteristics were collected, including the presence and type of pain, as well as data on treatment recommendations for subject teeth. Data forms are publicly available at [http://nationaldentalpbrn.org/study-results/cracked-tooth-registry.php]. Dentists were asked to confirm vitality of enrolled teeth with cold [30] (e.g., refrigerant, ice), although other methods such as air, air/water spray, or electric pulp testing were also used. Patients were asked about the presence of spontaneous pain. Pain to cold was determined using refrigerant, ice, or air/water spray, and pain upon biting was verified by having the patient bite on a device or instrument placed on the occlusal surface of the cracked tooth. To help patients distinguish between pain (an increased response to the cold or bite assessment) and an ordinary response, dentists were asked to subject a “normal” tooth, e.g. a contralateral tooth, to the same stimuli as the test tooth.
All visits after baseline and before Y1 during which the cracked tooth was treated were recorded as an interim visit. If the treatment was the completion of treatment planned at baseline, a treatment data form was completed, which included specific information about the type of treatment performed and about any internal cracks revealed by the treatment. If an interim visit was unplanned, the same data collected at baseline were collected again, including the patient’s symptoms, external crack characteristics, and any planned treatment. If treatment was provided, a treatment data form was also completed.
The practices were notified six months ahead of time of each patient’s annual recall date by the Data Coordinating Center (DCC); the offices then sent reminders to the patients based on the patient’s preferred mode of contact. Specific tracking procedures were used by the DCC for any patients who ultimately could not be contacted by the practices. Patients and practitioners were remunerated for the baseline and Y1 visits, but not any interim visits.
Analysis
The number of practitioners and patients who withdrew or were otherwise discontinued from the study were determined and the reasons why were described. The overall one-year retention rate was then calculated. The number of patients who attended the Y1 examination was categorized based on baseline treatment recommendation (monitor or treat) and whether any treatment was performed. Analyses were conducted on teeth not treated because changes in cracks could only be observed among these teeth; and similarly for changes in symptoms that were indicative of tooth damage from the crack.
Among untreated teeth, whether there were any changes in cracks between baseline and Y1 was determined, specifically, any increase in the number of cracks, as well as whether there were any changes in symptoms. For each type of pain identified at Y1, an increase could only occur if that type of pain was not present at baseline, and decreases could only occur if that type of pain was present at baseline but not at Y1. The association of change in each type of pain with any increase in the number of cracks was determined, as well as whether there was a difference by baseline treatment recommendation, namely, whether there were any associations with teeth recommended to be treated vs. monitored.
Associations of patient-, tooth-, and crack-level characteristics with increases in cracks were ascertained, and as well as with changes in symptoms, separately for increases and decreases. Significance of associations was determined by entering the characteristic into a logistic regression model that used generalized estimating equations (GEE) adjusted for clustering of patients within the practice, implemented using PROC GENMOD with CORR=EXCH option. Where there were sufficient numbers, predictive full models were built by entering all characteristics with p<0.10 after adjusting only for clustering of patients within the practice. This was followed with backwards elimination, again using GEE to adjust for clustering, to identify independent associations, being retained if p< 0.05, in a reduced model. All odds ratios and p-values reported were adjusted for clustering of patients within practitioner with GEE. All analyses were performed using SAS software (SAS v9.4, SAS Institute Inc., Cary NC).
Results
Year 1 follow-up visit
A total of 2,531 (88.6%) patients attended their year 1 follow-up visit (Y1), and had data recorded by 201 practitioners. One practitioner retired and seven did not have any study patients return. Twenty-seven patients were discontinued by study personnel for the following reasons prior to their Y1 visit: 12 patients had study teeth recommended for extraction, 6 moved, 5 died, 3 could not be located/contacted (lost to follow-up), and 1 had payment issues; another 8 patients withdrew and were thus discontinued. While the reasons for the remaining 292 not attending the Y1 recall are not known, patients not returning were more likely to have been younger, and more likely to have had symptomatic teeth with caries at baseline. They are eligible, however, for future examination, while the discontinued are not. The mean age of the 2.531 patients examined was 54.2 years (SD=11.6); 64% (n=1,619) were female.
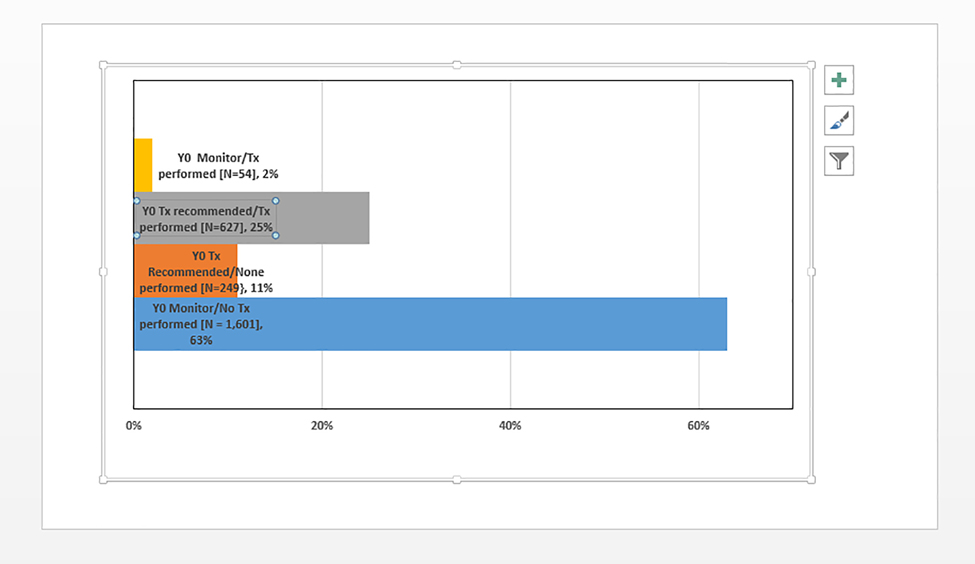
Presented in Figure 1 is the distribution of patients according to their baseline treatment recommendation, specifically whether they a) were recommended to be monitored (no invasive treatment planned) and b) had any treatment performed prior to coming in for the Y1 follow-up visit. There were 1,850 patients who came in for the Y1 follow-up visit who did not have any treatment performed on their cracked tooth; 1,601 of these were recommended to be monitored at baseline and 249 were recommended to have some treatment (244 restorative treatment; only; 4 endodontic plus restorative treatment; 1 endodontic treatment only), but treatment was not performed by the time of the Y1 follow-up visit. Six hundred and twenty-seven patients (25%) had a baseline treatment recommended and performed prior to Y1, and 54 (2%) did not have a baseline treatment recommended but did have a treatment performed at an interim visit prior to the Y1 recall (Details on interim visits are available in supplemental materials).
Figure 1:
Distribution of 2,351 patients attending Y1 visit according to baseline (Y0) treatment (Tx) recommendations and whether any treatment on the cracked teeth was performed prior to Y1 visit.
Changes in symptoms
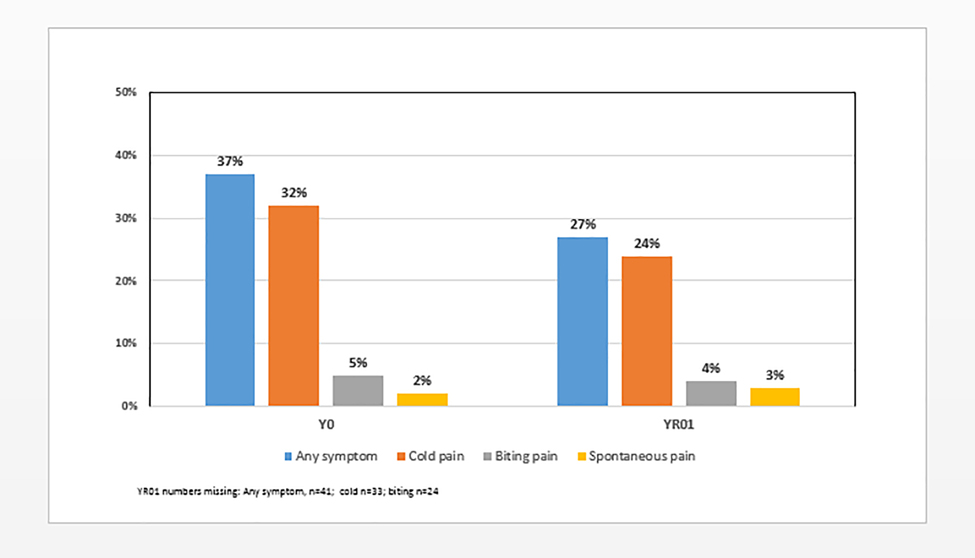
Among the 1,850 patients who did not have any treatment performed on the cracked tooth between the baseline and the Y1 visit, 37% (n=689) were symptomatic at baseline, 32% (n=582) had cold pain, 5% (n=150) had biting pain and 8% (n=143) had spontaneous pain; and at Y1, 27% (n=481) were symptomatic, 24% (n=428) had cold pain, 4% (n=70) had biting pain and 3% (n=54) had spontaneous pain (Figure 2). The primary difference between the baseline and Y1 distribution of symptoms among this cohort of 1,850 patients is a lower percentage of patients with cold pain at Y1 compared to baseline (p<0.001).
Figure 2.
Distribution of types of symptoms at baseline (Y0) and Y1 visit among 1,850 patients who had no treatment (Tx) performed prior to Y1 visit.
Although the overall symptom distributions at the baseline and Y1 examinations were similar at the level of the cohort of 1,850 patients, there was substantial change in symptoms at the level of the individual patient. Specifically, 32% (n=585) of this cohort of 1,850 patients had some type of changes in symptoms between the baseline and Y1 visits. Decreases (23%, n=421) were more than twice as frequent as increases (10%, n=194) (Table 1). Only 30 patients (2%) had both an increase and a decrease in some type of symptom. In examining changes by type of symptoms, the same pattern was observed, namely, more decreases than increases: for cold pain 16% (n=286) decreased and 8% (n=145) increased; for biting pain 6% (n=117) decreased and 2% (n=42) increased; for spontaneous pain 7% (n=123) decreased and 2% increased (n=34) (Table 1). Most cracked teeth had changes in only one direction: 67% (n=391) showed only decreases, 28% (n=164) showed only increases, and only 5% (n=30) had both increases and decreases. Most of the latter involved changes in cold pain, where 12 teeth had decreases and 14 had increases. Among the 194 patients who had an increase in symptoms, 89% (n=173) had increases in one type of pain, 6% (n=15) had increases in two pain types and 3% (n=6) in all three types. Similarly, among the 421 patients who had a decrease in symptoms, 80% (n=337) had increases in one type of symptom, 15% (n=63) had increases in two types of symptoms and 5% (n=21) in all three types.
Table 1.
Changes in symptoms overall and association with increase in number of cracks and with baseline treatment recommendations for the 1,850 subjects with one-year follow up data.
| Baseline recommendation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Monitor (N=1,601) | Treatment (N=249) | Any increase in # of cracks (N = 106) | |||||||||
| Change in symptoms | N1 | %2 | N1 | %2 | N1 | %2 | P4 | N | Row % | p4 | ||
| Any changes in symptoms | <0.001 | 0.7 | ||||||||||
| Yes | 585 | 32% | 448 | 28% | 137 | 55% | 36 | 6% | ||||
| No | 1,265 | 68% | 1,153 | 72% | 112 | 45% | 70 | 6% | ||||
| Any decrease in symptoms | <0.001 | 0.8 | ||||||||||
| Yes | 421 | 23% | 310 | 19% | 111 | 45% | 24 | 6% | ||||
| No (includes increases) | 1,429 | 77% | 1,291 | 81% | 138 | 55% | 82 | 6% | ||||
| Any increase in symptoms | 0.045 | 0.3 | ||||||||||
| Yes | 194 | 10% | 157 | 10% | 37 | 15% | 15 | 8% | ||||
| No (includes decreases) | 1,656 | 90% | 1,444 | 90% | 212 | 85% | 91 | 6% | ||||
| Any symptom | <0.001 | 0.8 | ||||||||||
| Decrease only | 391 | 21% | 291 | 18% | 100 | 40% | 21 | 5% | ||||
| Both increase & decrease | 30 | 2% | 19 | 1% | 11 | 4% | 3 | 10% | ||||
| No change | 1,265 | 68% | 1,153 | 72% | 112 | 45% | 70 | 6% | ||||
| Increase only | 164 | 9% | 138 | 9% | 26 | 10% | 12 | 7% | ||||
| Cold pain | 0.001 | 0.9 | ||||||||||
| Decrease | 286 | 16% | 219 | 14% | 67 | 27% | 15 | 5% | ||||
| No change | 1,386 | 76% | 1,232 | 77% | 154 | 62% | 78 | 6% | ||||
| Increase | 145 | 8% | 122 | 8% | 23 | 9% | 10 | 7% | ||||
| Bite pain | <0.001 | 0.6 | ||||||||||
| Decrease | 117 | 6% | 69 | 4% | 48 | 19% | 8 | 7% | ||||
| No change | 1,667 | 91% | 1,483 | 93% | 184 | 74% | 93 | 6% | ||||
| Increase | 42 | 2% | 31 | 2% | 11 | 4% | 4 | 10% | ||||
| Spontaneous | <0.001 | 0.14 | ||||||||||
| Decrease | 123 | 7% | 78 | 5% | 45 | 18% | 4 | 3% | ||||
| No change | 1,693 | 91% | 1,497 | 94% | 196 | 79% | 100 | 6% | ||||
| Increase | 34 | 2% | 26 | 2% | 8 | 3% | 2 | 6% | ||||
| # Symptom types increased | 0.045 | 0.4 | ||||||||||
| 0 | 1,656 | 90% | 1,444 | 90% | 212 | 85% | 91 | 6% | ||||
| 1 | 173 | 9% | 141 | 9% | 32 | 13% | 14 | 8% | ||||
| 2 | 15 | 1% | 10 | 1% | 5 | 2% | 1 | 7% | ||||
| 3 | 6 | <1% | 6 | 0% | 0 | 0% | 0 | 0% | ||||
| # Symptom types decreased | <0.001 | 0.4 | ||||||||||
| 0 | 1,429 | 77% | 1,291 | 81% | 138 | 55% | 82 | 6% | ||||
| 1 | 337 | 18% | 264 | 16% | 73 | 29% | 21 | 6% | ||||
| 2 | 63 | 3% | 36 | 2% | 27 | 11% | 3 | 5% | ||||
| 3 | 21 | 1% | 10 | 1% | 11 | 4% | 0 | 0% | ||||
Column Ns not summing to column total N above due to missing data (33 and 24 missing changes in cold and biting pain, respectively).
Column percents not summing to 100 due to rounding.
Changes in symptoms differed among untreated teeth according to baseline treatment recommendation (Table 1), with 55% of those recommended for treatment having greater changes in all types of symptoms compared with 28% recommended for monitoring (p<0.001). This was marginally significant for increases in symptoms (15% vs 10%, p=0.045), but strongly significant for decreases in symptoms (45% vs. 19%, p<0.001).
Changes in cracks
Among the 1,850 untreated cracked teeth, 106 (6%) had increases in the number of cracks from baseline to Y1: 81 (77%) had one additional crack, 19 (18%) had two and 5 (5%) had three additional cracks. There were no consistent/measurable changes in characteristics of cracks at Y1 that were present at baseline, e.g., detectable by explorer, blocking trans-illuminated light, directions of cracks or number of surfaces involved. There was no association of an increase in the number of cracks with any indices of changes in symptoms (Table 1). Increases in the number of cracks did not differ (p=0.6) between those recommended to be monitored (6%, 94/1,801) and those recommended to be treated at baseline (5%, 12/249).
Patient-level Characteristics (Table 2)
Table 2.
Patient-level characteristics of subjects with a cracked tooth.
| ALL | Increase in # cracks | Increase in # symptoms | Decrease in # of symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 1,850) | (N = 106) | (N = 194) | (N = 421) | ||||||||
| Characteristics | N1 | Col%2 | N | Row %3 | N | Row %3 | N | Row %3 | |||
| Gender | |||||||||||
| Male | 666 | 36% | 39 | 6% | 61 | 9% | 125 | 19% | |||
| Female | 1,183 | 64% | 67 | 6% | 132 | 11% | 296 | 25% | |||
| adjusted OR4 | OR = 0.96 | OR = 1.26 | OR =1.40 | ||||||||
| adjusted p5 | P = 0.9 | P = 0.086 | P= 0.002 | ||||||||
| Race6-ethnicity | |||||||||||
| White | 1,553 | 85% | 95 | 6% | 167 | 11% | 3.0 | 22% | |||
| Black | 77 | 4% | 2 | 3% | 13 | 17% | 16 | 21% | |||
| Asian | 35 | 2% | 1 | 3% | 1 | 3% | 9 | 26% | |||
| Hispanic | 122 | 7% | 7 | 6% | 10 | 8% | 32 | 26% | |||
| Other | 42 | 2% | 1 | 2% | 3 | 7% | 19 | 45% | |||
| adjusted p | P = 0.052 | P = 0.15 | P = 0.55 | ||||||||
| Age (years) | |||||||||||
| < 35 | 112 | 6% | 1 | 1% | 9 | 8% | 29 | 26% | |||
| 35 – 44 | 260 | 14% | 19 | 7% | 33 | 13% | 67 | 26% | |||
| 45 – 54 | 531 | 29% | 33 | 6% | 59 | 11% | 123 | 23% | |||
| 55 – 64 | 593 | 32% | 34 | 6% | 58 | 10% | 141 | 24% | |||
| 65 and older | 353 | 19% | 19 | 5% | 34 | 10% | 60 | 17% | |||
| adjusted OR [per 10 years] | OR = 1.02 | OR = 0.95 | OR = 0.91 | ||||||||
| adjusted p [trend] | P = 0.7 | P = 0.4 | P = 0.038 | ||||||||
| Dental insurance | |||||||||||
| None | 452 | 24% | 26 | 6% | 43 | 10% | 104 | 23% | |||
| Any | 1,398 | 76% | 80 | 6% | 151 | 11% | 317 | 23% | |||
| adjusted OR | OR = 0.85 | OR = 1.00 | OR = 0.91 | ||||||||
| adjusted p | P = 0.5 | P = 0.98 | P = 0.43 | ||||||||
| Education | |||||||||||
| <= High school | 271 | 15% | 8 | 3% | 25 | 9% | 68 | 25% | |||
| Some college/Associate | 642 | 35% | 40 | 6% | 61 | 10% | 153 | 24% | |||
| Bachelor | 541 | 29% | 31 | 6% | 69 | 13% | 124 | 23% | |||
| Graduate degree | 384 | 21% | 26 | 7% | 38 | 10% | 74 | 19% | |||
| adjusted p | P = 0.088 | P = 0.21 | P = 0.31 | ||||||||
| Region | |||||||||||
| Western | 254 | 14% | 21 | 8% | 31 | 12% | 59 | 23% | |||
| Midwest | 213 | 12% | 18 | 8% | 17 | 8% | 58 | 27% | |||
| Southwest | 370 | 20% | 19 | 5% | 28 | 8% | 94 | 25% | |||
| South Central | 382 | 21% | 11 | 3% | 50 | 13% | 93 | 24% | |||
| South Atlantic | 321 | 17% | 13 | 4% | 37 | 12% | 64 | 20% | |||
| Northeast | 310 | 17% | 24 | 8% | 31 | 10% | 53 | 17% | |||
| adjusted p | P = 0.087 | P = 0.4 | P = 0.21 | ||||||||
| Clench, grind, or press teeth together | |||||||||||
| No | 631 | 34% | 40 | 6% | 57 | 9% | 113 | 18% | |||
| Yes | 1,219 | 66% | 66 | 5% | 137 | 11% | 308 | 25% | |||
| adjusted OR | OR = 0.76 | OR = 1.28 | OR = 1.42 | ||||||||
| adjusted p | P = 0.18 | P = 0.13 | P = 0.004 | ||||||||
Column Ns not summing to column total N above due to missing data.
Column percents not summing to 100 due to rounding.
Percent of column within level of patient characteristic.
OR:Odds ratios adjusted for clustering of patients within practice.
P:P-value adjusted for clustering of patients within practice.
Race groups are all non-Hispanic.
Table 2 provides results about patient-level characteristics relative to changes in symptoms and increases in the number of cracks in enrolled teeth. No characteristic is associated with increases in cracks at p<0.05, although race-ethnicity, education and region are at p<0.10. For increase in symptoms, only patient gender had p<0.10 and none had p<0.05. For decreases in symptoms, female patients had more decreases than males (25% vs. 19%, p=0.002); the proportion of patients with a decrease in symptoms was higher for older patients (p=0.038); and ironically, patients with oral clenching/grinding habits reported at baseline appeared more likely to demonstrate a decrease in symptoms during follow-up compared to those who did not (25% vs 18%, p=0.004).
Tooth-level characteristics (Table 3)
Table 3.
Tooth-level characteristics of subjects with a cracked tooth
| ALL | Increase in # cracks | Increase in # symptoms | Decrease in # of symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 1,850) | (N = 106) | (N = 194) | (N = 421) | ||||||||
| Tooth-level characteristic1 | N1 | Col%2 | N | Row %3 | N | Row %3 | N | Row %3 | |||
| Molar | 1,478 | 80% | 85 | 6% | 160 | 11% | 365 | 25% | |||
| Premolar | 372 | 20% | 21 | 6% | 34 | 9% | 56 | 15% | |||
| adjusted OR4 | OR = 1.02 | OR = 1.09 | OR = 1.84 | ||||||||
| adjusted p6 | P = 0.9 | P = 0.66 | P < 0.001 | ||||||||
| 2 or more external cracks | 1,191 | 64% | 78 | 7% | 136 | 11% | 300 | 25% | |||
| 1 external crack | 659 | 36% | 28 | 4% | 58 | 9% | 121 | 18% | |||
| adjusted OR | OR = 1.32 | OR = 1.15 | OR = 1.48 | ||||||||
| adjusted p | P = 0.22 | P = 0.36 | P = 0.001 | ||||||||
| Wear facet through enamel | 424 | 23% | 83 | 6% | 41 | 10% | 115 | 27% | |||
| No wear facet through enamel | 1,426 | 77% | 23 | 5% | 153 | 11% | 306 | 21% | |||
| adjusted OR | OR = 0.92 | OR = 0.86 | OR = 1.29 | ||||||||
| adjusted p | P = 0.8 | P = 0.47 | P = 0.12 | ||||||||
| Exposed roots | 442 | 24% | 30 | 7% | 50 | 11% | 97 | 22% | |||
| No exposed roots | 1,408 | 76% | 76 | 5% | 144 | 10% | 324 | 23% | |||
| adjusted OR | OR = 1.21 | OR = 1.07 | OR = 0.85 | ||||||||
| adjusted p | P = 0.4 | P = 0.67 | P = 0.20 | ||||||||
| Caries present | 51 | 3% | 4 | 8% | 11 | 22% | 15 | 29% | |||
| No caries present | 1,799 | 97% | 102 | 6% | 183 | 10% | 406 | 23% | |||
| adjusted OR | OR = 1.65 | OR = 2.03 | OR = 1.24 | ||||||||
| adjusted p | P = 0.4 | P = 0.19 | P = 0.44 | ||||||||
| NCCL6 present | 180 | 10% | 13 | 7% | 21 | 12% | 38 | 21% | |||
| No NCCL present | 1,670 | 90% | 93 | 6% | 173 | 10% | 383 | 23% | |||
| adjusted OR | OR = 1.26 | OR = 1.14 | OR = 0.86 | ||||||||
| adjusted p | P = 0.5 | P = 0.55 | P = 0.43 | ||||||||
Column Ns not summing to column total N above due to missing data.
Column percents not summing to 100 due to rounding.
Percent of column within level of tooth characteristic.
OR: Odds ratios adjusted for clustering of patients within practice.
P: P-value adjusted for clustering of patients within practice.
NCCL: Non-carious cervical lesion.
There were two tooth-level characteristics that were associated with a decrease in the number of symptoms: for molars compared to premolars (25% vs. 15%, p<0.001) and for teeth with two or more external cracks compared to those teeth with only one crack (25% vs. 18%, p=0.01).
Crack-level characteristics (Table 4)
Table 4.
Crack-level characteristics of subjects with a cracked tooth.
| ALL | Increase in # cracks | Increase in # symptoms | Decrease in # of symptoms | |||||
|---|---|---|---|---|---|---|---|---|
| (N = 1,850) | (N = 106) | (N = 194) | (N = 421) | |||||
| Crack-level characteristics. | N1 | Col%2 | N | Row %3 | N | Row %3 | N | Row %3 |
| Stained | 1,508 | 82% | 91 | 6% | 158 | 10% | 336 | 22% |
| None stained | 342 | 18% | 15 | 4% | 36 | 11% | 85 | 25% |
| adjusted OR4 | OR = 1.36 | OR = 0.90 | OR = 0.78 | |||||
| adjusted p5 | P = 0.22 | P = 0.61 | P = 0.075 | |||||
| Detectable with an explorer | 1,258 | 68% | 73 | 6% | 126 | 10% | 293 | 23% |
| None were … with explorer | 592 | 32% | 33 | 6% | 68 | 11% | 128 | 22% |
| adjusted OR | OR = 0.92 | OR = 0.95 | OR = 1.01 | |||||
| adjusted p | P =0.7 | P = 0.76 | P = 0.94 | |||||
| Block transilluminated light | 1,202 | 65% | 73 | 6% | 110 | 9% | 280 | 23% |
| None blocked … light | 648 | 35% | 33 | 5% | 84 | 13% | 141 | 22% |
| adjusted OR | OR = 0.99 | OR = 0.80 | OR = 1.07 | |||||
| adjusted p | P = 0.98 | P = 0.24 | P = 0.57 | |||||
| Connected with restoration | 1,337 | 72% | 83 | 6% | 142 | 11% | 319 | 24% |
| None … w/ restoration | 513 | 28% | 23 | 4% | 52 | 10% | 102 | 20% |
| adjusted OR | OR = 1.34 | OR = 0.94 | OR = 1.18 | |||||
| adjusted p | P = 0.20 | P = 0.75 | P = 0.24 | |||||
| Connected w/ another crack | 119 | 6% | 5 | 4% | 11 | 9% | 33 | 28% |
| None … with another crack | 1,731 | 94% | 101 | 6% | 183 | 11% | 388 | 22% |
| adjusted OR | OR = 0.61 | OR = 0.70 | OR = 1.29 | |||||
| adjusted p | P = 0.24 | P = 0.25 | P = 0.21 | |||||
| Extended to root | 353 | 19% | 23 | 7% | 54 | 15% | 93 | 26% |
| None extended to root | 1,497 | 81% | 83 | 6% | 140 | 9% | 328 | 22% |
| adjusted OR | OR = 1.25 | OR = 1.50 | OE = 1.23 | |||||
| adjusted p | P = 0.36 | P = 0.063 | P = 0.16 | |||||
| Directions of cracks | ||||||||
| In horizontal direction | 547 | 30% | 35 | 6% | 61 | 11% | 132 | 24% |
| None in horizontal … | 1,303 | 70% | 71 | 5% | 133 | 10% | 289 | 22% |
| adjusted OR | OR = 1.28 | OR = 1.08 | OR = 1.19 | |||||
| adjusted p | P = 0.26 | P = 0.72 | P = 0.18 | |||||
| In vertical direction | 1,733 | 94% | 100 | 6% | 184 | 11% | 397 | 23% |
| None in vertical direction | 117 | 6% | 6 | 5% | 10 | 9% | 24 | 21% |
| adjusted OR | OR = 0.89 | OR = 1.01 | OR= 1.35 | |||||
| adjusted p | P = 0.8 | P = 0.97 | P = 0.24 | |||||
| In oblique direction | 177 | 10% | 11 | 6% | 18 | 10% | 55 | 31% |
| None in oblique direction | 1,673 | 90% | 95 | 6% | 176 | 11% | 366 | 22% |
| adjusted OR | OR = 1.11 | OR = 1.01 | OR = 1.38 | |||||
| adjusted p | P = 0.8 | P = 0.96 | P = 0.11 | |||||
| Surfaces cracks involved | ||||||||
| Mesial | 798 | 43% | 56 | 7% | 100 | 12% | 198 | 25% |
| None involved mesial | 1,052 | 57% | 50 | 5% | 94 | 9% | 223 | 21% |
| adjusted OR | OR = 1.33 | OR = 1.42 | OR = 1.09 | |||||
| adjusted p | P = 0.19 | P = 0.02 | P = 0.49 | |||||
| Occlusal | 806 | 44% | 55 | 7% | 81 | 10% | 191 | 24% |
| None involved occlusal | 1,044 | 56% | 51 | 5% | 113 | 11% | 230 | 22% |
| adjusted OR | OR = 1.49 | OR = 0.81 | OR = 1.05 | |||||
| adjusted p | P = 0.10 | P = 0.22 | P = 0.70 | |||||
| Distal | 904 | 49% | 57 | 6% | 100 | 11% | 235 | 26% |
| None involved distal | 946 | 51% | 49 | 5% | 94 | 10% | 186 | 20% |
| adjusted OR | OR = 1.07 | OR = 1.06 | OR = 1.41 | |||||
| adjusted p | P = 0.7 | P = 0.65 | P = 0.005 | |||||
| Facial | 975 | 53% | 55 | 6% | 106 | 11% | 242 | 25% |
| None involved facial | 875 | 47% | 51 | 60% | 88 | 10% | 179 | 20% |
| adjusted OR | OR = 0.92 | OR = 1.00 | OR = 1.38 | |||||
| adjusted p | P = 0.6 | P = 0.98 | P = 0.008 | |||||
| Lingual | 941 | 51% | 55 | 6% | 110 | 12% | 218 | 23% |
| None involved lingual | 909 | 49% | 51 | 6% | 84 | 9% | 203 | 22% |
| adjusted OR | OR = 0.90 | OR = 1.12 | OR = 1.08 | |||||
| adjusted p | P = 0.6 | P = 0.48 | P = 0.52 | |||||
| More than 1 surface | 846 | 46% | 59 | 7% | 87 | 10% | 206 | 24% |
| None involved > 1 surface | 1,004 | 54% | 47 | 5% | 107 | 11% | 215 | 21% |
| adjusted OR | OR = 1.55 | OR = 0.90 | OR = 1.11 | |||||
| adjusted p | P = 0.053 | P = 0.50 | P = 0.38 | |||||
Column Ns not summing to column total N above due to missing data.
Column percents not summing to 100 due to rounding.
Percent of column within level of crack characteristic.
OR: Odds ratios adjusted for clustering of patients within practice.
P: P-value adjusted for clustering of patients within practice.
No crack-level characteristic at baseline was associated with an increase in the number of cracks during follow-up. Teeth at baseline with a crack that extended to the root (15% vs. 9% with no crack on the root, p=0.063), and one that at baseline involved the mesial surface (12% vs. 9% that did not involve the mesial surface, p=0.02) were more likely to have increases in symptoms during follow-up.
Cracks at baseline that involved the distal surface (26% vs 20% that did not involve the distal surface, p=0.005) or the facial surface (25% vs. 20% not involving the facial surface, p=0.008) were more common on teeth that had decreases in symptoms during follow-up. Having a crack at baseline that was stained was associated with a decrease in symptoms (25% vs. 22% not stained cracks, p=0.075) but not at a statistically significant level.
Independent associations (Table 5)
Table 5.
Independent associations with increase in number of cracks and changes in symptoms from multivariable models.
| Individual1 | Full model3 | Reduced model4 | |||||
|---|---|---|---|---|---|---|---|
| Outcome of interest | Odds Ratio | P2 | Odds Ratio | P | Odds Ratio | 95% Confidence Interval | P |
| With increase in # external cracks | |||||||
| Race-ethnicity (categorical) | X5 | 0.052 | x | 0.15 | Removed6 | ||
| Education AD or higher | 1.96 | 0.02 | 1.60 | 0.018 | 1.63 | 1.03 – 2.58 | 0.019 |
| Region (categorical) | x | 0.087 | x | 0.042 | x | 0.04 | |
| Crack >= 2 surfaces | 1.55 | 0.053 | 2.04 | 0.038 | 2.01 | 1.01 – 4.00 | 0.03 |
| With increase in symptoms | |||||||
| Female | 1.26 | 0.086 | 1.24 | 0.12 | removed | ||
| Has crack that extends to root | 1.50 | 0.063 | 1.49 | 0.064 | removed | ||
| Has crack … mesial surface | 1.42 | 0.02 | 1.14 | 0.024 | 1.42 | 1.07 – 1.89 | 0.02 |
| With decrease in symptoms | |||||||
| Female | 1.40 | 0.002 | 1.35 | 0.008 | 1.36 | 1.09 – 1.68 | 0.006 |
| Age (per 10 years) | 0.91 | 0.038 | 0.97 | 0.48 | removed | ||
| Clench/grind teeth | 1.42 | 0.004 | 1.32 | 0.02 | 1.34 | 1.05 – 1.69 | 0.018 |
| Molar | 1.84 | <0.001 | 1.60 | 0.004 | 1.66 | 1.18 -- 2.35 | 0.002 |
| 2 or more external cracks | 1.48 | 0.001 | 1.26 | 0.10 | removed | ||
| Has crack … stains | 0.78 | 0.075 | 0.65 | 0.004 | 0.67 | 0.52 – 0.87 | 0.006 |
| Has crack … distal surface | 1.41 | 0.005 | 1.30 | 0.042 | 1.39 | 1.10 – 1.75 | 0.006 |
| Has crack … facial surface | 1.38 | 0.008 | 1.24 | 0.11 | 1.36 | 1.09 – 1.69 | 0.010 |
Adjusted only for clustering of patients within practice.
P-value adjusted only for clustering of patients within practice; all characteristics with p<0.10 are listed.
Model with all characteristics that had p<0.10 when adjusted only for clustering of patients within practice.
Backwards elimination of full model until all characteristics had p<0.05.
x:Odds ratios for specific values/comparisons of categorical variables are not presented.
P-value >0.05, removed from model.
When considered together, having at least an Associate Degree, more than 2 cracks, and region (Southwest and South Central having the highest percentage of teeth with an increase in cracks, and Western and Midwest having the lowest) were each associated with having an increase in number of cracks at p<0.05. Only having a crack at baseline that involved the mesial surface was associated with an increase in symptoms. Several characteristics were independently associated with a decrease in symptoms: female gender, clenching or grinding of teeth as reported at baseline, being on a molar, having a crack at baseline that involved the distal or facial surface. Having a crack at baseline that was stained was less likely to occur on a tooth that demonstrated a decrease in symptoms. None of the associations were strong.
Discussion
This report is unique in that there are no other published reports in which the progression of cracked teeth has been systematically followed over time. Other longitudinal studies addressed cracked teeth that had been treated restoratively [31–33] or endodontically (34, 35] There is one published study reporting on characteristics of cracked teeth, but it was a cross-sectional investigation with no follow up [13]. All these articles are characterized by relatively low sample sizes in comparison to the nearly 3,000 patient cohort presented in this CTR.
There are a number of interesting findings to emphasize in this report. First is the relative stability of cracked teeth over one year. Of the 1,850 untreated cracked teeth that were available to be assessed for signs of pain progression over time, over two-thirds (68%) showed no changes in symptoms. Likewise, only 6% of the patients (n=106) demonstrated an increase in the number of observable external cracks over that same time.
A second interesting and unexpected discovery was that most of the symptom changes that did occur were in the opposite direction from what was anticipated. Over twice as many symptomatic cracked teeth showed a decrease in symptoms (23%) vs. an increase in symptoms (10%). It is the empirical belief of many practitioners that the fate of cracked teeth only proceeds in one direction, with the number and extent of cracks increasing with time, and subsequently symptoms worsening with time. This leads us to believe that there are distinct differences in crack systems within teeth, with only a minority of teeth with cracks requiring intervention within the one-year period reported here. These results suggest that the majority of cracked teeth are relatively stable and lend themselves to monitoring rather than treating during the one-year period. A complication is that while this study is longitudinal, there is no way to know how long each tooth existed in its current condition before the study began. As this study is conducted in private practices with what are expected to be reasonably stable patient populations, it is likely that these teeth have been indirectly monitored for some time, and that there is a sporadic change in symptoms that occurs that does not imply a particular trend, and thus does not instigate the desire for treatment by either the patient or dentist. Two key questions can be asked: over how long a period of time will these cracked teeth remain stable, and what characteristics differentiate the stable teeth vs. those that are likely to degrade in the immediate future? These questions will be addressed soon in the three-year follow-up of this study.
The observational results of patient-, tooth- and crack-level characteristics relative to symptom changes and increased number of cracks were interesting in that some results (similar to other previously noted findings) were opposite to what would typically be expected. For example, at the patient level, individuals who admitted at baseline to clenching and grinding showed a trend towards decreasing symptoms over time. It is possible that the patient’s tolerance of the pain associated with a continuing habit, such as clenching or grinding, is increased with time, thus explaining the fact that they appear to experience less pain over time. Likewise, at the tooth level, cracked teeth with two or more cracks showed a somewhat decreased number of symptoms compared to teeth with only one crack. One may hypothesize that the creation of an additional crack or small cracks from an existing crack may relieve pain-stimulating tension, or perhaps physical strain, on the previously existing crack that had elicited symptoms, thus reducing the overall pain in the tooth. This would serve as a stress relieving mechanism commonly found in materials/objects under stress. For example, during cycling loading, such as chewing, significant sub-surface degradation occurs in enamel that allows it to avoid fracture through secondary cracking and crack bridging toughening mechanisms.[36]. We anticipate that the true association of characteristics to symptom and crack changes will ultimately be determined when the three-year results are analyzed and reported.
Another interesting finding was that of the patients who came to the dentist for an interim, but unplanned visit, 95% were symptomatic. In addition, 93% of these patients reported pain on biting, suggesting that the purpose of their visit was the presence of this new or enhanced pain due to biting on the study tooth with a crack.
Although nearly 3,000 patients were seen in this study, the cohort for analysis in this report was limited to 1,850 untreated patients. It is only possible to assess the natural progress of cracks in teeth that are not treated. While some study teeth had been extracted and therefore were not available for observation, and some others received endodontic treatment, the vast majority of treatment of cracked teeth was restorative [28]. Restorations can potentially affect the progression of cracks, as well as make cracks impossible to visualize, particularly if the restoration is a complete-coverage crown.
This study has a number of limitations. The study population was not randomly selected, which allowed practitioners to screen participants not only on the basis of meeting inclusion criteria, but for the practical reason of selecting those patients most likely to return for follow-up visits. While this is a relevant consideration in practice-based research, it is also possible that non-random selection could introduce bias, if study patients are not representative of the overall patient demographics in the practice. Similarly, conclusions from a study based on patients in a set number of practices may be limited to the populations represented by those practices. Since data were collected from nearly 3,000 patients in approximately 200 practices, across the entire U.S., the generalizability of the findings is likely quite good. Another potential weakness is the inherently subjective nature of certain data collected in the study. For example, a variety of factors can impact the validity of vitality testing, including preoperative pain, medications, patient age, patient gender and dentist training (30). However, cold testing has been found to exhibit higher validity than tooth percussion (30), heat (37) or electric pulp tester (37). To reduce variability between evaluations, dentists were asked to always use the same method for pulp and cold testing throughout the study. In addition, all participating personnel underwent training prior to participating. However, it must be recognized that some of the assessments are not objective measures, which could allow for some variation in recorded data among the participants.
The study strengths include a high number of a diverse patient population seen longitudinally, collecting a large amount of data in a systematic manner from a large variety of dental practices across the entire U.S.
Conclusion
This practice-based, longitudinal observational study followed the natural progression of a cohort of 1,850 patients with untreated cracked teeth. Cracked teeth remained relatively stable in terms of crack increases and symptom changes over one year of observation. In fact, there was greater reduction in symptoms, particularly pain due to cold, than increases. Cracked teeth that were originally recommended for treatment but remained untreated showed more changes in symptoms than teeth originally recommended for monitoring.
The ongoing importance of this project will be with continued observation of these teeth for an additional two years with the ultimate goal of determining those factors that are most predictive of adverse outcomes in cracked teeth.
Supplementary Material
Acknowledgments
This work was supported by NIH grants U19-DE-28717 and U19-DE-22516. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully. The manuscript co-authors report having no conflicts of interest. An Internet site devoted to details about the nation’s network is located at http://NationalDentalPBRN.org. We are very grateful to the network’s Node Coordinators and other network staff (Midwest Region: Tracy Shea, RDH, BSDH; Western Region: Stephanie Hodge, MA; Northeast Region: Christine O’Brien, RDH; South Atlantic Region: Hanna Knopf, BA, and Deborah McEdward, RDH, BS, CCRP; South Central Region: Shermetria Massengale, MPH, CHES, and Ellen Sowell, BA; Southwest Region: Stephanie Reyes, BA, Meredith Buchberg, MPH, and Colleen Dolan, MPH; network program manager (Andrea Mathews, BS, RDH) and program coordinator (Terri Jones)), along with network practitioners and their dedicated staffs to conduct the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Bader JD, Shugars DA, Roberson TM. Using crowns to prevent tooth fracture. Community Dent Oral Epidemiol 24 (1996) 47–51. [DOI] [PubMed] [Google Scholar]
- [2].Lubisich E, Hilton T, Ferracane J. Cracked teeth: a review of the literature. J Esthet Restor Dent 22 (2010) 158–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Cameron CE Cracked Tooth Syndrome. J Am Dent Assoc 68 (1964) 405–411. [DOI] [PubMed] [Google Scholar]
- [4].Chong BS Bilateral cracked teeth: a case report. Int Endod J 22 (1989) 193–196. [DOI] [PubMed] [Google Scholar]
- [5].Thomas GA The diagnosis and treatment of the cracked tooth syndrome. Aust Prosthodont J 3 (1989) 63–67. [PubMed] [Google Scholar]
- [6].Geurtsen W The cracked-tooth syndrome: clinical features and case reports. Int J Periodontics Restorative Dent 12 (1992) 395–405. [PubMed] [Google Scholar]
- [7].Turp JC, Gobetti JP The Cracked Tooth Syndrome: an elusive diagnosis. J Am Dent Assoc 127 (1996) 1502–1507. [DOI] [PubMed] [Google Scholar]
- [8].Homewood CI Cracked tooth syndrome-Incidence, clinical findings, and treatment. Aust Dent J 43 (1998) 217–222. [PubMed] [Google Scholar]
- [9].Davis R, Overton JD Efficacy of bonded and nonbonded amalgam in the treatment of teeth with incomplete fractures. J Am Dent Assoc 130 (1999) 571–572. [DOI] [PubMed] [Google Scholar]
- [10].Ratcliff S, Becker IM, Quinn L Type and incidence of cracks in posterior teeth. J Prosthet Dent 86 (2001) 168–172. [DOI] [PubMed] [Google Scholar]
- [11].Lynch CD, McConnell RJ The Cracked Tooth Syndrome. J Can Dent Assoc 68 (2002) 470–475. [PubMed] [Google Scholar]
- [12].Griffin JD Jr. Efficient, conservative treatment of symptomatic cracked teeth. Compend Contin Educ Dent 27 (2006) 93–102. [PubMed] [Google Scholar]
- [13].Seo D, Yi Y, Shin S, Park J. Analysis of factors associated with cracked teeth. J Endod 38 (2012) 288–292. [DOI] [PubMed] [Google Scholar]
- [14].Ailor JE Managing incomplete tooth fractures. J Am Dent Assoc 131 (2000) 1168–1174. [DOI] [PubMed] [Google Scholar]
- [15].Wright HM, Loushine RJ, Weller RN, Kimbrough WF, Waller J, Pashley DH Identification of resected root-end dentinal cracks: a comparative study of transillumination and dyes, J Endod 30 (2004) 712–715. [DOI] [PubMed] [Google Scholar]
- [16].Clark DJ, Sheets CG, Paquette JM, Definitive diagnosis of early enamel and dentin cracks based on microscopic evaluation. J. Esthet Restor Dent 17(Special Issue) (2003) 15: SI 7–SI. [DOI] [PubMed] [Google Scholar]
- [17].Culjat MO, Singh RS, Brown ER, Neurgaonkar RR, Yoon DC, White SN Ultrasound crack detection in a simulated human tooth. Dentomaxillofac Radiol 34 (2005) 80–85. [DOI] [PubMed] [Google Scholar]
- [18].Imai K, Shimada Y, Sadr A, Sumi Y, Tagami J. Noninvasive cross-sectional visualization of enamel cracks by optical coherence tomography in vitro. J Endod 38 (2012) 1269–1274. [DOI] [PubMed] [Google Scholar]
- [19].Jun M, Ku H, Kim E, Kim H, Kwon HH, Kim B. Detection and Analysis of Enamel Cracks by Quantitative Light-induced Fluorescence Technology. J Endod 42 (2016) 500–504. [DOI] [PubMed] [Google Scholar]
- [20].Sheets C, Wu J, Rashad S, Phelan M, Earthman J. In vivo study of the effectiveness of quantitative percussion diagnostics as an indicator of the level of the structural pathology of teeth. J Prosthet Dent 116 (2016) 191–199. [DOI] [PubMed] [Google Scholar]
- [21].Sheets C, Wu J, Rashad S, Phelan M, Earthman J. In vivo study of the effectiveness of quantitative percussion diagnostics as an indicator of the level of the structural pathology of teeth after restoration. J Prosthet Dent 117 (2017) 218–225. [DOI] [PubMed] [Google Scholar]
- [22].Sheets C, Wu J, Earthman J. Quantitative percussion diagnostics as an indicator of the level of the structural pathology of teeth: Retrospective follow-up investigation of high-risk sites that remained pathological after restorative treatment. J Prosthet Dent 119 (2018) 119: 928–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Banerji S, Mehta S, Millar B. Cracked tooth syndrome. Part 2: restorative options for the management of cracked tooth syndrome. British Dent J 208 (2010) 503–514. [DOI] [PubMed] [Google Scholar]
- [24].Alkhalifah S, Alkandari H, Sharma P, Moule A. Treatment of cracked teeth. J Endod 43 (2017) 1579–1586. [DOI] [PubMed] [Google Scholar]
- [25].Hilton TJ, Funkhouser E, Ferracane JL, Gilbert GH, Baltuck C, Benjamin P, Louis D, Mungia R, Meyerowitz C. Correlation between symptoms and external cracked tooth characteristics: findings from the National Dental Practice-Based Research Network. J Am Dent Assoc 148 (2017) 246–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hilton T, Funkhouser E, Ferracane J, Gordan V, Huff K, Barna J, Mungia R, Marker T, Gilbert GH, NDPBRN Collaborative Group. Associates of types of pain with crack-level, tooth-level, and patient-level characteristics in posterior teeth with visible cracks: Findings from the National Dental PBRN Collaborative Group. J Dent 70 (2018) 67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ferracane JL, Funkhouser E, Hilton TJ, Gordan VV, Graves CL, Giese KA, Shea W, Pihlstrom D, Gilbert GH; National Dental Practice-Based Research Network Collaborative Group. Observable characteristics coincident with internal cracks in teeth: Findings from The National Dental Practice-Based Research Network. J Am Dent Assoc 149 (2018)885–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hilton T, Funkhouser E, Ferracane J, Schultz-Robins M, Gordan V, Bramblett B, Snead R, Manning W, Remakel J, NDPBRN Collaborative Group. Recommended treatment of cracked teeth: Results from the National Dental Practice-Based Research Network. J Prosthet Dent, epub in advance of publication (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Gilbert GH, Williams OD, Korelitz JJ, et al. Purpose, structure, and function of the United States National Dental Practice-Based Research Network. J Dent 41 (2013) 1051–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Pigg M, Nixdorf D, Nguyen R, Law. A Validity of preoperative clinical findings to identify dental pulp status: a National Dental Practice-Based Research Network Study. J Endod 42 (2016) 935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Krell K, Rivera E. A six-year evaluation of cracked teeth diagnosed with reversible pulpitis: treatment and prognosis. J Endod 33 (2007) 1405–1407. [DOI] [PubMed] [Google Scholar]
- [32].Opdam N, Roeters J, Loomans B. Bronkhorst E. Seven-year Clinical Evaluation of Painful Cracked Teeth Restored with a Direct Composite Restoration. J Endod 34 (2008) 808–811. [DOI] [PubMed] [Google Scholar]
- [33].Tan L, Chen N, Poon C, Wong H. Survival of root filled cracked teeth in a tertiary institution. International Endodontic Journal, 39 (2006) 886–889. [DOI] [PubMed] [Google Scholar]
- [34].Sim I, Toh-Seong L, Chen N Decision Making for Retention of Endodontically Treated Posterior Cracked Teeth: A 5-year Follow-up Study. J Endod 42 (2016) 225–229. [DOI] [PubMed] [Google Scholar]
- [35].Krell K, Caplan D. 12-month Success of Cracked Teeth Treated with Orthograde Root Canal Treatment. J Endod 44 (2018) 543–548. [DOI] [PubMed] [Google Scholar]
- [36].Gao SS, An BB, Yahyazadehfar M, Zhang D, Arola DD. Contact fatigue of human enamel: Experiments, mechanisms and modeling. J Mech Behav Biomed Mater. 60 (2016) 438–450. [DOI] [PubMed] [Google Scholar]
- [37].Petersson K, Soderstrom C, Kiani-Anaraki M, Levy G. Ealuation of the ability of thermal and electric tests to register pulp vitality. Endon Dent Traumatol 15 (1999) 127–131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.