Dear Editor,
We read with interest a study published in your journal. Zhaohai Zheng and colleagues through a systematic review of clinical trials found that smoking was risk factors for disease progression in patients with COVID-19.1 However, there is no study to show whether the severity of (Coronavirus disease 2019) COVID-19 is related to drinking. Only some studies have shown that no substantial difference was observed in the habits of drinking between severe and non-severe COVID-19 patients.2 , 3 But these studies drew conclusions only based on the cohort study which the sample size is limited. The aim of this study is getting a more convincing conclusion by a systematic review and meta analysis to quantitatively assess whether drinking is associated with the severity of COVID-19.
In this study, patients with acute respiratory distress syndrome (ARDS) who requires life support, mechanical ventilation, or intensive care unit (ICU) support are considered as severe patients.4 Due to the use of public anonymous data, this work does not require ethical approval. Studies that meet the following criteria were included: (1) patients have a laboratory confirmed diagnosis of COVID-19; (2) provided data of severe or no-severe between patients with drinking and non-drinking; (3) published in Chinese and English, no restricted on publication date. Case reports, studies with a sample size of no more than 10 patients, review articles, and conference abstracts were excluded. We only focused on the outcomes of the incidence of severe or non-severe COVID-19 disease between drinking and non-drinking patients.
We searched the following databases up to May 8, 2020 without language limitations: PubMed, EMBASE.com, Web of Science, the Cochrane Central Register of Controlled Trials (CENTRAL), China National Knowledge Infrastructure (CNKI), Chinese Biomedical Literature Database (CBM), and Wanfang. Various combinations and permutations of the following search terms “coronavirus”, “COVID-19”, “SARS-COV-2”, “2019-nCOV”, “drinking” and “alcohol consumption” were used. We also searched the reference lists of eligible studies and relevant systematic reviews to find eligible studies.
Two reviewers independently conducted study selection and data extraction. Any disagreement among authors about study selection and data collection was investigated by supervising authors. The following data were collected: name of the first author, journal title, publication date, location of the study, publication language, recruitment time frame, sample size, age and sex of patients, and outcomes of interest.
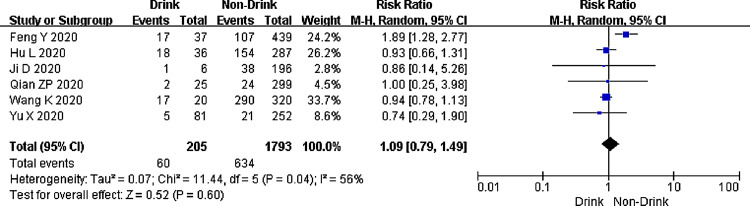
Data analyses were performed using Review Manager 5.3 (Nordic Cochrane Centre, Copenhagen, Denmark). The risk ratio (RR) and the corresponding 95% confidence interval (CI) were the principal measures. We used the chi-square test together with the I2 statistic to assess the heterogeneity, considering I2 ≥ 50% indicative of considerable heterogeneity. If heterogeneity exists, the random effects model was used; if not, the fixed effects model was used. In addition, we also conducted sensitivity analysis by excluding studies published in Chinese to assess the stability of the results.
A total of 2472 were retrieved from the electronic database. After sequentially screening through the titles/abstracts and the full texts, six studies met the inclusion criteria and were pooled into a meta-analysis. All studies were conducted in China. One study published in Chinese,6 five studies published in English.2 , 3 , 5 , 7 , 8 All studies incorporated a total of 1998 patients (1053 males) between December 18, 2019 and February 24, 2020. The sample size of patients per study ranged from 202 to 476 (Table 1 ).
Table 1.
Characteristics of included studies.
| Study | Country | Language | Recruitment time frame | Sample | Age. (years)a | Sex |
Drinking |
Non-drinking |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Severe | Non-severe | Severe | Non-severe | ||||||
| Ji D5 | China | English | 2020.01.20-2020.02.18 | 202 | 44.5(34.8-54.1) | 113 | 89 | 1 | 6 | 38 | 196 |
| Feng Y2 | China | English | 2020.01.01-2020.02.15 | 476 | 53(40-64) | 271 | 205 | 17 | 747 | 107 | 439 |
| Qian ZP6 | China | Chinese | 2020.01.20-2020.02.24 | 324 | 51(36,64) | 167 | 157 | 2 | 491 | 24 | 299 |
| Yu X7 | China | English | 2019.12.18-2020.02.19 | 333 | 50(35-63) | 172 | 161 | 5 | 505 | 21 | 252 |
| Hu L3 | China | English | 2020.01.08-2020.02.20 | 323 | 61(23-91) | 166 | 157 | 18 | 489 | 154 | 287 |
| Wang K8 | China | English | 2020.01.01-2020.02.20 | 340 | NR | 164 | 176 | 17 | 504 | 290 | 320 |
Age data presented as median (IQR) or mean (SD). NR, not reported.
The pooled RR of these studies is summarized in Fig. 1 , which shows that the drinking did not impact the severity of COVID-19 (RR: 1.09, 95%CI: 0.79-1.49, P=0.600, I2=56%). We explored the source of heterogeneity by excluding each study sequentially. When we excluded the study published by Feng Y et al.,2 the pooled RR of other studies was 0.93 (95%CI: 0.79-1.09, P=0.38) and I2 was 0. It shows that the heterogeneity may come from this study.2 In addition, sensitivity analysis indicated the result (RR: 1.09, 95%CI: 0.78-1.53) did not change substantially after excluding the Chinese study.
Fig. 1.
Forest plot of the meta-analysis of the impact of drinking to COVID-19.
Currently, there are two diametrically opposed views on whether alcohol consumption will increase during the COVID-19 pandemic: (1) increase in consumption for some populations, particularly men, due to distress experienced as a result of the pandemic; (2) a lowered level of consumption, based on the decreased physical and financial availability of alcohol.9 Therefore, it is meaningful to explore whether the severity of COVID-19 related to drinking. It can guide people's lifestyle during the epidemic. Our study showed that drinking is not related to the severity of COVID-19. However, this study did not consider the volume and time of drinking. In future, researcher should pay attention to whether drinking volume and time are related to the increase of covid-19. In addition, researcher can focus more on changing other lifestyles, such as smoking.10
However, this study was limited by small sample size and the study location (all in China). If more data is published, this study should be re-analyzed to provide more reliable evidence.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgments
Funding
This work was supported by the Emergency Research Project of Key Laboratory of Evidence-based Medicine and Knowledge Translation of Gansu Province (Grant No. GSEBMKT-2020YJ01).
Role of the Funding Source
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1.Zheng Z., Peng F., Xu B. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis [published online ahead of print, 2020 Apr 23] J Infect. 2020 doi: 10.1016/j.jinf.2020.04.021. S0163-4453(20)30234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feng Y., Ling Y., Bai T. COVID-19 with Different Severity: A Multi-center Study of Clinical Features. American Journal of Respiratory and Critical Care Medicine. 2020 doi: 10.1164/rccm.202002-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu L., Chen S., Fu Y. Risk Factors Associated with Clinical Outcomes in 323 COVID-19 Hospitalized Patients in Wuhan, China. Clinical infectious diseases. 2020 doi: 10.1093/cid/ciaa539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Su Y., Tu G.W., Ju M.J. Comparison of CRB-65 and quick sepsis-related organ failure assessment for predicting the need for intensive respiratory or vasopressor support in patients with COVID-19. Journal of Infection. 2020 doi: 10.1016/j.jinf.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ji D., Qin E., Xu J. Implication of non-alcoholic fatty liver diseases (NAFLD) in patients with COVID-19: a preliminary analysis. Journal of hepatology. 2020 doi: 10.1016/j.jhep.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qian Z.P., Mei X., Zhang Y.Y. Analysis of baseline liver biochemical parameters in 324 cases with novel coronavirus pneumonia in Shanghai area. Zhonghua Gan Zang Bing Za Zhi. 2020 doi: 10.3760/cma.j.cn501113-20200229-00076. [DOI] [PubMed] [Google Scholar]
- 7.Yu X., Sun X., Cui P. Epidemiological and Clinical Characteristics of 333 Confirmed Cases with Coronavirus Disease 2019 in Shanghai, China. Transboundary and emerging diseases. 2020 doi: 10.1111/tbed.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang K., Zuo P., Liu Y. Clinical and laboratory predictors of in-hospital mortality in patients with COVID-19: a cohort study in Wuhan, China. Clinical infectious diseases. 2020 doi: 10.1093/cid/ciaa538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rehm J., Kilian C., Ferreira-Borges C. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug Alcohol Rev. 2020 doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vardavas C.I., Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis. 2020 doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]