Over the past 20 years, organised efforts in Africa have described and addressed the burden of sickle cell disease, with commendable achievements. However, there have been four limiting factors. First, there have been few multisite, well described cohort studies of sickle cell disease in Africa. Second, there is no evidence yet that consistent standards of care are applied across Africa. Third, there are insufficient human resources, both in numbers and skills. Finally, there are few programmes exploring pertinent research questions related to sickle cell disease in Africa to guide locally appropriate interventions. This situation is compounded by inadequate collaboration within Africa that would otherwise allow sharing of experience and reduce duplication of efforts. SickleInAfrica is a consortium set up to address these factors by shaping health policy in countries that bear the greatest burden of sickle cell disease worldwide. The countries selected are characterised by high sickle cell disease prevalence, mortality and morbidity, and suboptimal use of interventions that could reduce mortality in children younger than 5 years. The time for this initiative is optimal, as there has been considerable progress in developing genomic research in Africa, specifically in sickle cell disease. These advances will not only improve our understanding of genetic diversity in Africa, but will also clarify how a monogenic disease can have such heterogeneous manifestations. It is imperative that Africa contributes to genomics research to improve health and introduce curative treatments of sickle cell disease.
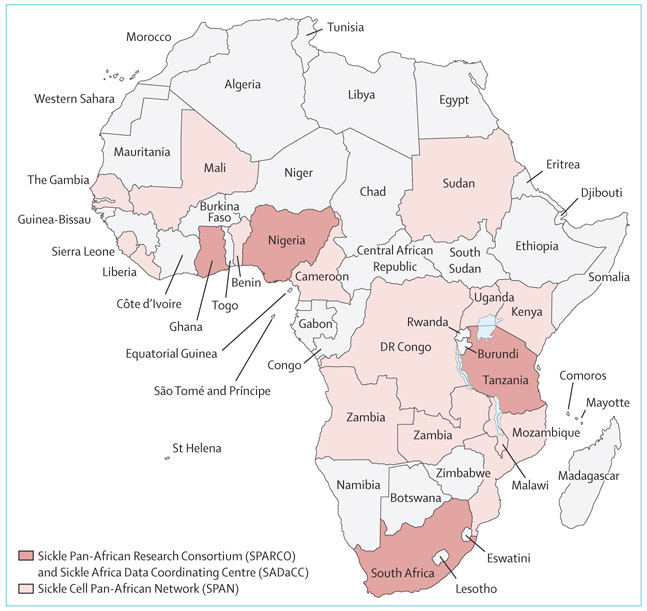
SickleInAfrica has unique and innovative features as it brings together clinicians, academics, and scientists from existing sickle cell disease programmes, and ongoing activities in health, education, and research embedded in local infrastructures. It has three initiatives (figure). The first is the Sickle Pan-African Research Consortium (SPARCO), with sites in Tanzania (Muhimbili University of Health and Allied Sciences, Dar es Salaam), Nigeria (University of Abuja, Abuja), and Ghana (Kwame Nkrumah University of Science and Technology, Kumasi) that aims to develop research capacity for sickle cell disease through a multidimensional approach, addressing infrastructure, education and skills, provision of longitudinal research data, and the translation of research into practice. The second is the Sickle Africa Data Coordinating Center (SADaCC) based in the University of Cape Town (Cape Town, South Africa); it is the administrative centre coordinating data standardisation and supporting communications for SPARCO. The third is the Sickle Cell Pan-African Network (SPAN), a network of researchers, clinicians, funders, and centres working in sickle cell disease in 22 sites in 17 countries across Africa.
Figure:
Countries involved in the Sickle Pan-African Research Consortium (SPARCO) and the Sickle Africa Data Coordinating Centre (SADaCC), and the Sickle Cell Pan-African Network (SPAN)
SPARCO and SADaCC are establishing a disease registry set with the target to register 13 000 patients with sickle cell disease across Africa over 3 years and which will be linked to institutional health records. Between October, 2017, and March, 2019, 6285 (48%) of the target number of patients with sickle cell disease were enrolled (1751 [28%] in Ghana, 2900 [46%] in Nigeria, and 1634 [26%] in Tanzania). The consortium has developed standard operating procedures and guidelines to help with quality and accurate data collection. SADaCC coordinated the development of the most comprehensive knowledge portal for sickle cell disease to date, Sickle Cell Disease Ontology, which provides a centralised, electronic database of all patients attending participating centres. Guidelines for locally appropriate standards of care are being developed, considering resources available at primary, secondary and tertiary care services, as well as those needed for care at home. These guidelines are based on 12 model guidelines published in the past 10 years, including seven general guidelines (four African, from Nigeria, Tanzania, South Africa, and Ghana, and three from Jamaica, USA, and Canada), three European paediatric guidelines, and one adult and one parents-specific guideline from the UK. Priority subject areas were selected and reviewed, and the first draft of standards of care at tertiary level is being used at consortium sites.
Working with existing programmes, SickleInAfrica is supporting education with the aim of increasing the quantity and quality of skills available and train enough health-care professionals, educators, and scientists working in sickle cell disease. A review of existing training programmes in Africa is underway and there are ongoing skill-strengthening initiatives in health care, data management, and research methodology at individual sites and at the consortium level. The consortium has also collaborated with academic and professional entities to improve training by developing new courses or strengthening existing ones in universities in Ghana, Nigeria, Tanzania, and South Africa. Research fellows supported by the consortium participate in programmes with partners from the public and private sectors.
In preparation for multi-country research, informed consent and assent forms and data sharing agreements are in place. Participating sites are also evaluating existing data for comparative analysis, and SPARCO is building on existing research activities to develop concept notes for future research with a priority on large cohort studies describing the spectrum of disease and evaluating disease modifying factors, including genomics. Furthermore, SickleInAfrica is developing implementation studies focusing on screening of infants, infection prevention, and increasing the use of hydroxyurea systematically. As an infrastructure programme, SickleInAfrica is not only planning to do research, but will collaborate with existing research initiatives and programmes that can complement, rather than compete or duplicate efforts in resource-constrained settings, including SickleGenAfrica, REACH, REDAC, AFROSickleNet, and sickle cell disease initiatives of the American Society of Hematology.
To ensure coordination, organisational structures, operating manuals, and work plans have been established through the development of working relationships, online meeting platforms, and operating procedures with stakeholders and other partners. The teams at SPARCO sites and working groups hold monthly online meetings with the coordinating SPARCO Hub and SADaCC. Four consortium meetings have been held so far, in November, 2016 (Dar-es-Salaam, Tanzania), April, 2018 (Accra, Ghana), November, 2018 (Abuja, Nigeria), and March, 2019 (Tunis, Tunisia). An independent observational and monitoring board nominated by the funder (National Institute of Health, Bethesda, MD, USA) provides oversight.
A crucial part of the consortium is engagement of key stakeholders, particularly communities of patients with sickle cell disease and governments. For community engagement, all consortium sites have appointed a representative to engage the sickle cell disease community at institutional or national level, and participating countries are actively engaged with patient groups and organisations, and are working together to raise awareness and resources. The appointed community representatives from each country are involved in discussions and activities to inform the research, standards of care, and education initiatives. Engagement with governments is crucial for the sustainability of SickleInAfrica beyond the funding period for SPARCO and SADaCC, which ends in 2021. As such, SickleInAfrica has strengthened and established partnerships by creating SPAN and is providing administrative support for the network to become an autonomous entity by 2021. Nationally, member countries provide regular updates to their health ministries to align activities with government policies and plans and leverage existing health and research networks. At regional level, consortium countries are also working with medical organisations, such as the West African College of Physicians (Ghana, Nigeria) and the College of Pathologists of Central Eastern and Southern Africa (COPECSA; Arusha, Tanzania). At continental level, SickleInAfrica is informing and sharing learning experience with WHO, and globally, working with the Global Sickle Cell Disease Network, World Bank, and other entities investing in health, education, and research in Africa.
It has been long known that the highest burden of sickle cell disease is in Africa. However, the provision of services and health care for patients in Africa has been sub-optimal. In certain aspects, the gap between knowledge and action has been widening. For example, most patients with sickle cell disease in Africa do not have the benefit of an early diagnosis, and even those diagnosed do not receive chemoprophylaxis with penicillin or non-curative, but disease-modifying, treatments such as hydroxyurea. Furthermore, doing research in a region without helping to improve health services and build capacity in a sustainable manner is not ethical. It is time that the academic community, health-care providers, and educational institutions in Africa take the lead to obtain the commitment and resources from partners in the public and private sectors for the implementation of evidence-based and widely accepted policies to manage sickle cell disease in the continent. SickleInAfrica aims to reduce the gap between knowledge and action by developing effective partnerships, which will result in substantial advances to health and research outcomes, and we think that we will have the influence to achieve this goal.
Footnotes
We declare no competing interests.
Contributor Information
Julie Makani, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Raphael Z Sangeda, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Obiageli Nnodu, University of Abuja, Abuja, Nigeria.
Victoria Nembaware, University of Cape Town, Cape Town, South Africa.
Alex Osei-Akoto, Komfo Anokye Teaching Hospital, Kumasi, Ghana; Kwame Nkrumah University of Science and Technology, Kumasi, Ghana.
Vivian Paintsil, Komfo Anokye Teaching Hospital, Kumasi, Ghana.
Emmanuel Balandya, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Jill Kent, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Lucio Luzzatto, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Solomon Ofori-Acquah, University of Pittsburgh, Pittsburgh, PA, USA and University of Ghana, Accra, Ghana.
Olofunmi I Olopade, University of Chicago, Chicago, IL, USA.
Kisali Pallangyo, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Irene K Minja, Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania.
Mario Jonas, University of Cape Town, Cape Town, South Africa.
Gaston K Mazandu, University of Cape Town, Cape Town, South Africa.
Nicola Mulder, University of Cape Town, Cape Town, South Africa.
Kwaku Ohene-Frempong, Sickle Cell Foundation of Ghana, Kumasi, Ghana.
Ambroise Wonkam, University of Cape Town, Cape Town, South Africa.