Abstract
Background
Dental health care workers (DHCW's) are invariably at a higher risk of contracting COVID-19. The objectives were; to investigate the current knowledge on COVID-19 among the DHCW's; and to conduct quasi-experiment among the DHCW's who were unaware of the disseminated COVID-19 information.
Methods
A nationwide cross-sectional study targeting dental interns, auxiliaries, and specialists with a two-staged cluster sampling technique was performed. A 17-item questionnaire was subjected to reliability and validity tests before being administered. The participants for quasi-experiment were separated from the original sample after their initial response. Chi-square test assessed responses to knowledge statements between the participants. Difference in mean knowledge scores between the categories of DHCW's and sources of COVID-19 information was assessed using ANOVA. Data from the quasi experiment (pre vs post knowledge intervention) was subjected to paired t-test. Percentage of DHCWs providing correct or wrong responses to each knowledge statement at baseline and after 7 days were compared using McNemar test.
Results
The overall sample consisted of 706 (N) participants, and the DHCW's with no prior knowledge on COVID-19 (N = 206) were part of the quasi experiment. Findings from cross-sectional study revealed that knowledge was significantly (p < 0.05) related to the qualification level (interns vs auxiliaries vs specialists). However, the difference in the source of information (WHO/CDC vs Journal articles vs MoH) did not demonstrate any effect. Number of participants with correct responses to knowledge questions had significantly (p < 0.05) increased after intervention. Also, the overall mean knowledge score (10.74 ± 2.32 vs 12.47 ± 1.68; p < 0.001) had increased significantly after the intervention.
Conclusion
In conclusion, the basic knowledge on COVID-19 among the DHCW's in Saudi Arabia is acceptable. Timely dissemination of information by the Ministry of Health, Saudi Arabia had a positive impact on the COVID-19 knowledge score of the DHCW's.
Keywords: COVID-19, 2019-nCoV, Corona virus, Knowledge, Awareness, Oral health care workers, Dentists, Dental Auxiliaries
Introduction
December 2019 had witnessed the sudden outbreak of novel corona virus (2019-nCoV), which initiated from the city of Wuhan in China and had rapidly spread to other parts of the country [1], [2]. The World Health Organization (WHO) has recently announced it to be pandemic, as the number of people suffering from the Corona virus disease (COVID-19) has increased globally [3]. Experts have regarded it to be more concerning than SARS-CoV and MERS-CoV [4], [5], [6]. The patients suffering from corona virus disease (COVID-19) have symptoms which include fever, cough, myalgia or fatigue, headache, and hemoptysis [7], [8]. Research updates since 2019 have established grave consequences of COVID-19 through its serious effects on the lungs causing severe pneumonia and finally death [9], [10].
Dental health care workers (DHCW's) are invariably at a higher risk of contracting this infectious disease; and oral health care settings may act as a means of disease transfer [11]. Another published report also suggests that the patients visiting dental settings for their routine or other emergency treatments and the DHCW's can serve as a reservoir for the microorganisms that cause various infectious diseases, including COVID-19 [12]. The Public Health Administrators throughout the world [13], [14] and specifically the Ministry of Health (MoH) in Saudi Arabia are actively working toward the control of spread of the Novel corona virus (2019-nCoV) by disseminating timely educational videos, educational brochures, and social media updates for health care practitioners and also for general population [15]. Frequent hand sanitizing, following cough etiquettes, and using personal protective equipment's (masks, gloves, eye shields etc.) have been encouraged. In addition, travel history of the patients has been added to the health charting, and contact information of a nearby tertiary hospital equipped with diagnostic tests and quarantine facilities for suspected cases are made available.
A well-informed health care professional on COVID-19 such as a DHCW may not only be a prominent source to promulgate correct knowledge in the community but also to create a safe haven for the work colleagues and patients. Currently, there is no study conducted to assess the awareness of COVID-19 among the DHCW's. The objective of the current study is to conduct a nationwide survey in order to investigate the current knowledge and plausible misconceptions among the dental interns, auxiliaries, and specialists working in different regions of Saudi Arabia. It is hypothesized that the online dissemination of educational materials on COVID-19 by various international health authorities such as the Center for Disease Control (CDC), World Health Organization (WHO), and also the regional bodies like the Ministry of Health (MoH), Saudi Arabia have kept the DHCW's well informed. A secondary objective of the study was to conduct a quasi-experiment among the DHCW's who were not aware of the information provided by the aforementioned sources in order to see the effect of the COVID-19 brochures disseminated by the MoH on their level of knowledge. As the situation is changing rapidly, it is imperative to evaluate the effectiveness of the education materials from the regulatory authorities in improving the knowledge and eventually practices of the DHCW's. Such information could help in providing necessary feedback to the regulatory authorities.
Methodology
Study design, study sample, and sampling technique
A nationwide cross-sectional study was conducted in March 2020 with a representative sample targeting dental interns, auxiliaries, and specialists working across various universities in Saudi Arabia. A two-staged cluster sampling technique was utilized. In the first stage, the university clusters having dental treatment facilities were isolated according to their specific regions (n = 14). Simple random procedure was applied to select 4 regions (Riyadh, Jeddah, Asir, Jazan) out of 14. In the second stage, one government university from each region was selected and all interns, auxiliaries, and specialists were requested to complete the survey.
Sample size calculation
A computation for a sample size was not required, as a probability sampling technique was utilized. However, a post hoc sample size for the quasi-experiment design addressing the secondary objective was calculated. The required sample size was nearly 100 [15], [16], [17], with the power of 80%, α value of 0.05, a β of 0.2, with 50% estimation of good knowledge, and a possible dropout rate of 20%.
Assessment tool and method of administration
The questionnaire comprised of 17 questions pertaining to the knowledge on COVID-19. In addition, their qualification level (dental interns, dental auxiliaries, and dental specialists) and source of COVID-19 information (WHO/CDC websites, Journal articles, MoH, or No information) was also enquired. The questionnaire was initially subjected to pilot testing to evaluate face and content validity. For content validity, the questionnaire was administered to two subject experts from the Department of Preventive Dental Sciences, who had a clear understanding of the COVID-19 guidelines for health workers from the Ministry of Health. The questionnaire was then administered to 20 interns at the College of Dentistry, Jazan University through interviews to assess its face validity. They were asked if they had difficulty in understanding any questions. All the participants found the questionnaire to be appropriate and easy to understand, only minor grammatical corrections were made at this stage. The questionnaire was then subjected to Test-retest (with a time gap of one week) reliability and Cronbach's alpha value of 0.84 (p < 0.05) was obtained.
The tested questionnaire was administered to the potential participants (N = 706) using Survey Monkey software [18]. This method was adopted in accordance with the current distant socialization being implemented throughout the country. The participants (n = 206) who did not come across any reliable source of information were separated from the original sample after their initial response; and a quasi-experiment was performed to investigate the effect of intervention. These participants were then provided (via email) with the brochure that was circulated by the Ministry of Health, Saudi Arabia and the questionnaire was repeated after a period of 7 days (n = 206).
Statistical analysis
Descriptive statistics were conducted. Frequencies and percentages were used to demonstrate the responses of the DHCW's to knowledge statements. Mean and standard deviations were used to present the overall knowledge scores. Chi-square test was used to assess the differences in responses to the knowledge statements based on their occupational role or qualification level. One-way analysis of variance was used to evaluate the difference in mean knowledge scores between the categories of occupation roles and sources of COVID-19 information. To assess the difference in COVID-19 mean knowledge scores among the participants who were included in the quasi experiment design (pre vs post knowledge intervention), a paired t-test was computed. Percentage of DHCWs providing correct or wrong responses to each knowledge statement at baseline and after 7 days were compared using McNemar test. There was no missing data. All the analyses were performed using SPSS version 24 and a p value of <0.05 was considered statistically significant.
Ethical considerations and source of funds
Permissions from the human research ethics review board, Jazan University was obtained (dated: 10-03-2020). An informed consent was obtained from all the study participants. The research was self-funded and there are no conflicts of interest to be reported.
Results
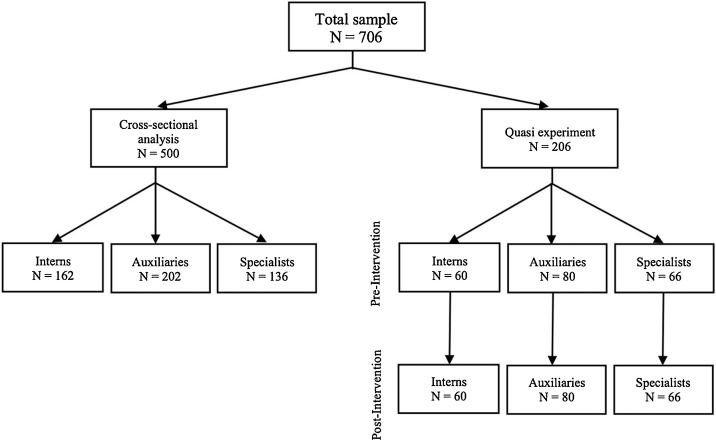
The total number of participants for the current study were 706 (N) with an overall response rate of 70%. The study population was then stratified into two groups based on the self-reported knowledge of COVID-19. The result section first describes findings from the sample of DHCW (interns, auxiliaries, and specialists) who reported to have received information of COVID-19 from a reliable source (WHO, CDC, Journal articles, or MoH) prior to the current study, and it comprised of 500 (n) participants. Then, the findings from the sample of DHCW (29.4%) who did not receive any information was reported in the subsequent section, and it included 206 (n) participants (Fig. 1 ).
Fig. 1.
Diagrammatic representation of the study flow and the number of participants at each step.
Findings from the cross-sectional study
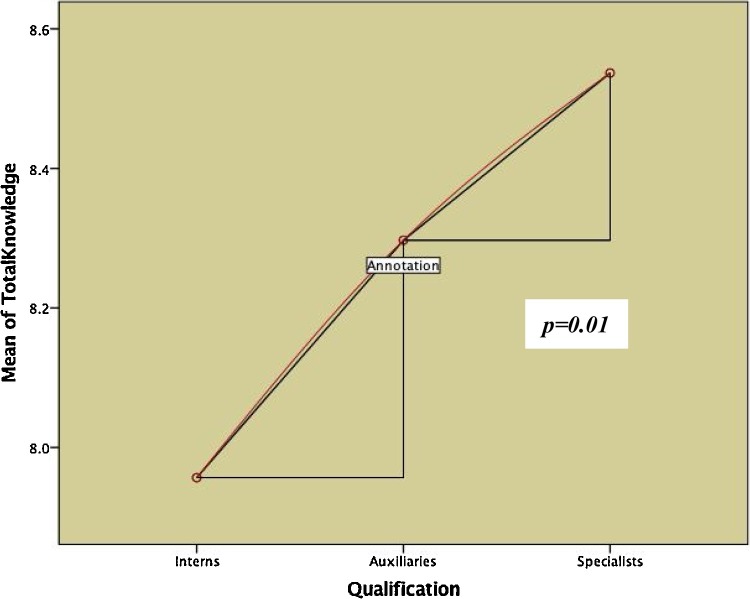
There were 500 (N) study participants who reported to have received information on COVID-19 from sources such as WHO/CDC website (5.8%), journal articles (74.4%), and Ministry of Health website (19.8%). Among them, 32.4% were dental interns, 40.4% were dental auxiliaries, and 27.2% were dental specialists. The most common misconception among the interns (90%), auxiliaries (81.7%), and specialists (85.3%) was the consideration of sneezing as a common symptom of COVID-19, rather than a means of infection transmission (Table 1 ). It was observed that the responses obtained on the knowledge questions was significantly (p < 0.05) related to the qualification level (interns vs auxiliaries vs specialists) of the study participants (Table 1). Also, Fig. 2 demonstrated that the mean knowledge score between the study participants significantly (p = 0.01) increased as the level of qualification (job title) increased. However, the difference in the source of information (WHO/CDC vs Journal articles vs MoH) did not have any effect on the mean knowledge scores (Table 2 ).
Table 1.
Self-reported misconceptions on COVID-19 among the dental interns, auxiliaries, and specialists (N = 500).
| Knowledge items | Interns N = 162 | Auxiliaries N = 202 | Specialists N = 136 | p-value |
|---|---|---|---|---|
| Is sneezing a symptom | ||||
| Yes | 146 (90.1) | 165 (81.7) | 116 (85.3) | 0.1 |
| Noa | 16 (9.9) | 37 (18.3) | 20 (14.7) | |
| Immediate response for suspected case | ||||
| Call emergency | 74 (45.7) | 58 (28.7) | 44 (32.4) | <0.001 |
| Refer him to a doctor | 20 (12.3) | 15 (12.4) | 3 (2.2) | |
| Ask travel historya | 68 (42) | 114 (56.4) | 87 (64) | |
| Do not know | 0 | 5 (2.5) | 2 (1.5) | |
| Emergency number | ||||
| 937a | 152 (93.8) | 146 (72.3) | 128 (94.1) | <0.001 |
| 999 | 3 (1.9) | 25 (12.4) | 3 (2.2) | |
| 811 | 0 | 2 (1.0) | 0 | |
| Do not know | 7 (4.3) | 29 (14.4) | 5 (3.7) | |
| Safe distance | ||||
| Three feeta | 61 (37.7) | 131 (64.9) | 77 (56.6) | <0.001 |
| Six feet | 40 (24.7) | 27 (13.4) | 31 (22.8) | |
| Five feet | 29 (17.9) | 17 (8.4) | 12 (8.8) | |
| Do not know | 32 (19.8) | 27 (13.4) | 16 (11.8) | |
| Relatively low risk group | ||||
| 0–19 yearsa | 91 (56.2) | 110 (54.5) | 65 (47.8) | 0.1 |
| 20–29 years | 31 (19.1) | 41 (20.3) | 40 (29.4) | |
| 30 year and older | 6 (3.7) | 15 (7.4) | 13 (9.6) | |
| Do not know | 34 (21) | 36 (17.8) | 18 (13.2) | |
| What is COVID-19? | ||||
| Immunity Disorder | 49 (30.2) | 39 (19.3) | 20 (14.7) | 0.07 |
| SARS infection | 8 (4.9) | 26 (12.9) | 19 (14) | |
| Acquired Zoonotic | 36 (22.2) | 76 (37.6) | 54 (39.7) | |
| Pulmonary diseasea | 69 (42.6) | 61 (30.2) | 43 (31.6) | |
| High risk of infection transmits | ||||
| Dentists | 78 (48.1) | 34 (16.8) | 39 (28.7) | <0.001 |
| Nurses | 6 (3.7) | 16 (7.9) | 8 (5.9) | |
| Patients | 1 (0.6) | 5 (2.5) | 8 (5.9) | |
| Alla | 77 (47.5) | 147 (72.8) | 81 (59.6) | |
| Air borne | ||||
| Yesa | 81 (50) | 91 (45) | 78 (57.4) | <0.001 |
| No | 71 (43.8) | 95 (47) | 52 (38.2) | |
| I do not know | 10 (6.2) | 16 (7.9) | 6 (4.4) | |
| High proportion of morbidity | ||||
| Old peoplea | 150 (92.6) | 183 (90.6) | 130 (95.6) | 0.03 |
| Young children | 3 (1.9) | 3 (1.5) | 6 (4.4) | |
| I do not know | 9 (5.6) | 16 (7.9) | 0 | |
| Latency period | ||||
| Immediately | 0 | 2 (1) | 0 | 0.01 |
| 2–14 daysa | 100 (61.7) | 150 (74.3) | 100 (73.5) | |
| 14–28 days | 61 (37.7) | 47 (23.3) | 31 (22.8) | |
| I do not know | 1 (0.6) | 3 (1.5) | 5 (3.7) | |
| First symptoms | ||||
| Fever | 6 (3.7) | 9 (4.5) | 5 (3.7) | 0.01 |
| Difficulty in breathing | 9 (5.6) | 11 (5.4) | 14 (10.3) | |
| Botha | 144 (88.9) | 180 (89.1) | 117 (86) | |
| Do not know | 3 (1.9) | 2 (1.0) | 0 | |
| Common symptoms of flu and COVID-19 | ||||
| Sneezing and fever | 64 (39.5) | 93 (46) | 68 (50) | 0.5 |
| Coughing and fevera | 11 (6.8) | 23 (11.4) | 16 (11.8) | |
| Both right | 44 (27.2) | 42 (20.8) | 37 (27.2) | |
| Both wrong | 16 (9.9) | 22 (10.9) | 10 (7.4) | |
| Do not know | 27 (16.6) | 20 (9.9) | 5 (3.7) | |
| Antibiotics for treatment | ||||
| Yes | 13 (8) | 18 (8.9) | 10 (7.4) | 0.02 |
| Noa | 106 (65.4) | 141 (69.8) | 103 (75.7) | |
| Do not know | 43 (26.5) | 41 (20.3) | 20 (14.7) | |
| Recommended personal prevention | ||||
| Wear n95 mask | 22 (13.6) | 44 (21.8) | 37 (27.2) | 0.1 |
| Surgical mask | 4 (2.5) | 53 (26.2) | 68 (47.8) | |
| Washing handsa | 136 (84) | 103 (51) | 34 (25) | |
| Other recommended precaution | ||||
| Avoid Undercooked food | 3 (1.9) | 2 (1.0) | 0 | <0.001 |
| Inhale steam | 96 (59.3) | 151 (74.8) | 100 (73.5) | |
| Avoid large crowdsa | 41 (25.3) | 31 (15.3) | 23 (16.9) | |
| Do not touch face with hands | 19 (11.7) | 2 (1) | 2 (1.5) | |
| Do not know | 3 (1.9) | 14 (6.9) | 11 (8.1) | |
| Availability of vaccine for COVID-19 | ||||
| Yes | 5 (3.1) | 11 (5.4) | 13 (9.6) | <0.001 |
| Noa | 130 (80.2) | 160 (79.2) | 110 (80.9) | |
| Do not know | 27 (16.7) | 29 (14.4) | 13 (9.6) | |
| Hot air prevents COVID-19 | ||||
| Yes | 8 (4.9) | 9 (4.5) | 4 (2.9) | 0.1 |
| Noa | 139 (85.8) | 179 (88.6) | 130 (95.6) | |
| Do not know | 15 (9.3) | 14 (6.9) | 2 (1.5) | |
Chi-square test.
Bold values are for the significant p-values.
Correct responses.
Fig. 2.
Difference in the mean COVID-19 knowledge scores of DHCW's, by qualification.
Table 2.
Mean difference in the COVID-19 knowledge score, by qualification of participants and the source of knowledge (N = 500).
| Qualification | Knowledge score |
|||
|---|---|---|---|---|
| Mean (SD) | df | Mean square | p-value | |
| Interns | 7.96 (1.61) | 2 | 12.78 | 0.01 |
| Auxiliaries | 8.30 (1.78) | |||
| Specialists | 8.54 (1.39) | |||
| Source | ||||
| WHO/CDC | 7.66 (2.06) | 2 | 6.47 | 0.1 |
| Journal article | 8.26 (1.65) | |||
| Ministry of Health | 8.41 (1.41) | |||
One-way ANOVA.
Bold values are for the significant p-values.
Findings from the quasi-experiment
In the segregated sample of study participants who had not yet received information on COVID-19 at the time of data collection, a quasi-experiment was performed. The intervention source utilized was the MoH brochure (supplementary file), which was provided to them immediately after their first response (pre-intervention). The post-intervention response from the same participants was collected after a duration of one week. In this study sample (N = 206); 29.1% were dental interns, 38.8% were dental auxiliaries, and 32% were specialists. Similar to the previous sample, the findings from the misconceptions revealed that most of the interns (76.7%), auxiliaries (78.8%), and specialists (83.3%) thought that sneezing was a symptom of COVID-19 (Table 3 ). Also, the responses for most of the knowledge questions was significantly (p < 0.05) dependent on the qualification level of the study participants (Table 3).
Table 3.
Self-reported misconceptions on COVID-19 among dental interns, auxiliaries, and specialists (N = 206).
| Knowledge items | Interns N = 60 | Auxiliaries N = 80 | Specialists N = 66 | p-value |
|---|---|---|---|---|
| Is sneezing a symptom | ||||
| Yes | 46 (76.7) | 63 (78.8) | 55 (83.3) | 0.6 |
| Noa | 14 (23.3) | 17 (21.3) | 11 (16.7) | |
| Immediate response for suspected case | ||||
| Call emergency | 29 (48.3) | 22 (27.5) | 26 (39.4) | 0.2 |
| Refer him to a doctor | 13 (21.7) | 18 (22.5) | 10 (15.2) | |
| Ask travel historya | 16 (26.7) | 38 (47.5) | 28 (42.4) | |
| Do not know | 2 (3.3) | 2 (2.5) | 2 (3) | |
| Emergency number | ||||
| 937a | 49 (81.7) | 49 (61.3) | 51 (77.3) | 0.1 |
| 999 | 1 (1.7) | 12 (15) | 5 (7.6) | |
| 811 | 1 (1.7) | 2 (2.5) | 0 (0) | |
| Do not know | 9 (15) | 17 (21.3) | 10 (15.2) | |
| Safe distance | ||||
| Three feeta | 27 (45) | 59 (73.8) | 47 (71.2) | 0.004 |
| Six feet | 10 (16.7) | 4 (5) | 7 (10.6) | |
| Five feet | 4 (6.7) | 7 (8.8) | 4 (6.1) | |
| Do not know | 19 (31.7) | 10 (12.5) | 8 (12.1) | |
| Relatively low risk group | ||||
| 0–19 yearsa | 23 (38.3) | 45 (56.3) | 29 (43.9) | 0.2 |
| 20–29 years | 14 (23.3) | 13 (16.3) | 19 (28.8) | |
| 30 year and older | 3 (5) | 4 (5) | 5 (7.6) | |
| Do not know | 20 (33.3) | 18 (22.5) | 13 (19.7) | |
| What is COVID-19? | ||||
| Immunity Disorder | 5 (8.3) | 17 (21.3) | 9 (13.6) | 0.01 |
| SARS infection | 7 (11.7) | 11 (13.8) | 5 (7.6) | |
| Acquired Zoonotic | 44 (73.3) | 33 (41.3) | 40 (60.6) | |
| Pulmonary diseasea | 4 (6.7) | 19 (23.8) | 12 (18.2) | |
| High risk of infection transmits | ||||
| Dentists | 11 (18.3) | 4 (5) | 14 (21.2) | 0.01 |
| Nurses | 14 (23.3) | 11 (13.8) | 7 (10.6) | |
| Patients | 0 (0) | 0 (0) | 1 (1.5) | |
| Alla | 35 (58.3) | 65 (81.3) | 44 (66.7) | |
| Air borne | ||||
| Yesa | 38 (63.3) | 26 (32.5) | 41 (62.1) | <0.001 |
| No | 20 (33.3) | 44 (55) | 25 (37.9) | |
| I do not know | 2 (3.3) | 10 (12.5) | 0 (0) | |
| High proportion of morbidity | ||||
| Old peoplea | 54 (90) | 69 (86.3) | 66 (100) | 0.02 |
| Young children | 1 (1.7) | 0 (0) | 0 (0) | |
| I do not know | 5 (8.3) | 11 (13.8) | 0 (0) | |
| Latency period | ||||
| Immediately | 0 (0) | 1 (1.3) | 0 (0) | 0.4 |
| 2–14 daysa | 46 (76.7) | 61 (76.3) | 43 (65.2) | |
| 14–28 days | 13 (21.7) | 17 (21.3) | 23 (34.8) | |
| I do not know | 1 (1.7) | 1 (1.3) | 0 (0) | |
| First symptoms | ||||
| Fever | 3 (5) | 2 (2.5) | 3 (4.5) | 0.5 |
| Difficulty in breathing | 5 (8.3) | 4 (4) | 1 (1.5) | |
| Botha | 49 (81.7) | 73 (91.3) | 62 (93.9) | |
| Do not know | 1 (1.7) | 1 (1.3) | 0 (0) | |
| Common symptoms of flu and COVID-19 | ||||
| Sneezing and fever | 22 (36.7) | 35 (43.8) | 40 (60.6) | 0.1 |
| Coughing and fevera | 10 (16.7) | 9 (11.3) | 8 (12.1) | |
| Both right | 13 (21.7) | 12 (15) | 10 (15.2) | |
| Both wrong | 9 (15) | 10 (12.5) | 3 (4.5) | |
| Do not know | 6 (10) | 13 (16.3) | 5 (7.6) | |
| Antibiotics for treatment | ||||
| Yes | 5 (8.3) | 6 (7.5) | 2 (3) | <0.001 |
| Noa | 36 (60) | 55 (68.8) | 62 (93.9) | |
| Do not know | 19 (31.7) | 18 (22.5) | 2 (3) | |
| Recommended personal prevention | ||||
| Wear n95 mask | 13 (21.7) | 17 (21.3) | 23 (34.8) | 0.2 |
| Surgical mask | 1 (1.7) | 5 (6.3) | 4 (6.1) | |
| Washing handsa | 44 (73.3) | 57 (71.3) | 39 (59.1) | |
| Other recommended precaution | ||||
| Avoid Undercooked food | 1 (1.7) | 2 (2.5) | 2 (3) | <0.001 |
| Inhale steam | 27 (45) | 54 (67.5) | 39 (59.1) | |
| Avoid large crowdsa | 25 (41.7) | 12 (15) | 8 (12.2) | |
| Do not touch face with hands | 1 (1.7) | 1 (1.3) | 6 (9.1) | |
| Do not know | 4 (6.7) | 10 (12.5) | 11 (16.7) | |
| Availability of vaccine for COVID-19 | ||||
| Yes | 0 (0) | 2 (2.5) | 0 (0) | 0.1 |
| Noa | 46 (76.7) | 61 (76.3) | 59 (89.4) | |
| Do not know | 12 (20) | 16 (20) | 7 (10.6) | |
| Hot air prevents COVID-19 | ||||
| Yes | 3 (5) | 5 (6.3) | 0 (0) | 0.5 |
| Noa | 51 (85) | 64 (80) | 64 (97) | |
| Do not know | 6 (10) | 11 (13.8) | 2 (3) | |
Chi-square test.
Bold values are for the significant p-values.
Correct responses.
The comparative findings for pre and post intervention knowledge score independently for dental interns, dental auxiliaries, and dental specialists are presented in Table 4 . It was observed that number of participants with correct responses to most of the knowledge questions significantly (p < 0.05) increased after the intervention. Also, the overall mean knowledge score (10.74 ± 2.32 vs 12.47 ± 1.68; p < 0.001), and the individual knowledge scores among the interns (10.18 ± 2.17 vs 12.43 ± 1.62; p < 0.001), auxiliaries (10.64 ± 2.69 vs 12.60 ± 1.67; p < 0.001), and the specialists (11.36 ± 1.81 vs 12.35 ± 1.77; p = 0.003) increased significantly after the intervention (Table 5 ).
Table 4.
Comparative difference in the proportion of dental interns, auxiliaries, and specialists before and after the intervention.
| Knowledge items | Interns N = 60 |
Auxiliaries N = 80 |
Specialists N = 66 |
|||
|---|---|---|---|---|---|---|
| Pre n (%) | Post n (%) | Pre n (%) | Post n (%) | Pre n (%) | Post n (%) | |
| Is sneezing a symptom? | ||||||
| Incorrect response | 14 (23.3) | 6 (10) | 17 (21.3) | 11 (13.8) | 11 (16.7) | 9 (13.6) |
| Correct response | 46 (76.7) | 54 (90) | 63 (78.8) | 69 (86.3) | 55 (83.3) | 57 (86.4) |
| p-value | 0.1 | 0.2 | 0.6 | |||
| Immediate response for suspected case | ||||||
| Incorrect response | 44 (73.3) | 34 (56.7) | 42 (52.5) | 26 (32.5) | 38 (57.6) | 22 (33.3) |
| Correct response | 16 (26.7) | 26 (43.3) | 38 (47.5) | 54 (67.5) | 28 (42.4) | 44 (66.7) |
| p-value | 0.02 | 0.01 | 0.01 | |||
| Emergency number | ||||||
| Incorrect response | 11 (18.3) | 4 (6.7) | 31 (38.8) | 4 (5) | 15 (22.7) | 4 (6.1) |
| Correct response | 49 (81.7) | 56 (93.3) | 49 (69.3) | 76 (95) | 51 (77.3) | 62 (93.9) |
| p-value | 0.03 | <0.001 | 0.01 | |||
| Safe distance | ||||||
| Incorrect response | 33 (55) | 1 (1.7) | 21 (26.3) | 3 (3.8) | 19 (28.8) | 6 (9.1) |
| Correct response | 27 (45) | 59 (98.3) | 59 (73.8) | 77 (96.3) | 47 (71.2) | 60 (90.9) |
| p-value | <0.001 | <0.001 | 0.004 | |||
| Relatively low risk group | ||||||
| Incorrect response | 37 (61.7) | 2 (3.3) | 35 (43.8) | 4 (5) | 37 (56.1) | 6 (9.1) |
| Correct response | 23 (38.3) | 58 (96.7) | 45 (56.3) | 76 (95) | 29 (43.9) | 60 (90.9) |
| p-value | <0.001 | <0.001 | <0.001 | |||
| What is COVID-19? | ||||||
| Incorrect response | 56 (93.3) | 8 (13.3) | 61 (76.3) | 7 (8.8) | 54 (81.8) | 9 (13.6) |
| Correct response | 4 (6.7) | 52 (86.7) | 19 (23.8) | 73 (91.3) | 12 (18.2) | 57 (86.4) |
| p-value | <0.001 | <0.001 | <0.001 | |||
| High risk of infection transmits | ||||||
| Incorrect response | 25 (41.7) | 30 (50) | 15 (18.8) | 35 (43.8) | 22 (33.3) | 28 (42.4) |
| Correct response | 35 (58.3) | 30 (50) | 65 (81.3) | 45 (56.3) | 44 (66.7) | 38 (57.6) |
| p-value | 0.3 | <0.001 | 0.3 | |||
| Air borne | ||||||
| Incorrect response | 22 (36.7) | 29 (48.3) | 54 (67.5) | 32 (40) | 25 (37.9) | 28 (42.4) |
| Correct response | 38 (63.3) | 31 (51.7) | 26 (32.5) | 48 (60) | 41 (62.1) | 38 (57.6) |
| p-value | 0.1 | <0.001 | 0.6 | |||
| High proportion of morbidity | ||||||
| Incorrect response | 6 (10) | 4 (6.7) | 11 (13.8) | 3 (3.8) | 0 | 4 (6.1) |
| Correct response | 54 (90) | 56 (93.3) | 69 (86.3) | 77 (96.3) | 66 (100) | 62 (93.9) |
| p-value | 0.5 | 0.03 | 0.04 | |||
| Latency period | ||||||
| Incorrect response | 14 (23.3) | 23 (38.3) | 19 (23.8) | 22 (27.5) | 23 (34.8) | 18 (27.3) |
| Correct response | 46 (76.7) | 37 (61.7) | 61 (76.3) | 58 (72.5) | 43 (65.2) | 48 (72.7) |
| p-value | 0.1 | 0.6 | 0.3 | |||
| First symptoms | ||||||
| Incorrect response | 11 (18.3) | 6 (10) | 7 (8.8) | 11 (13.8) | 4 (6.1) | 10 (15.2) |
| Correct response | 49 (89.7) | 54 (90) | 73 (91.3) | 69 (86.3) | 62 (93.9) | 56 (84.8) |
| p-value | 0.2 | 0.3 | 0.1 | |||
| Common symptoms of flu and COVID | ||||||
| Incorrect response | 38 (63.3) | 2 (3.3) | 45 (56.3) | 24 (30)) | 26 (39.4) | 24 (36.4) |
| Correct response | 22 (36.7) | 58 (96.7) | 35 (43.8) | 56 (70) | 40 (60.6) | 42 (63.6) |
| p-value | <0.001 | 0.001 | 0.7 | |||
| Antibiotics for treatment | ||||||
| Incorrect response | 24 (40) | 23 (38.3) | 25 (31.3) | 23 (28.8) | 4 (6.1) | 17 (25.8) |
| Correct response | 36 (60) | 37 (61.7) | 55 (68.8) | 57 (71.3) | 62 (93.9) | 49 (74.2) |
| p-value | 0.8 | 0.7 | 0.004 | |||
| Recommended personal prevention | ||||||
| Incorrect response | 16 (26.7) | 35 (58.3) | 23 (28.8) | 62 (77.5) | 27 (40.9) | 52 (78.8) |
| Correct response | 44 (73.3) | 25 (41.7) | 57 (71.3) | 18 (22.5) | 39 (59.1) | 14 (21.2) |
| p-value | <0.001 | <0.001 | <0.001 | |||
| Other recommended precaution | ||||||
| Incorrect response | 35 (58.3) | 45 (75) | 68 (85) | 66 (82.5) | 58 (87.9) | 54 (81.8) |
| Correct response | 25 (41.7) | 15 (25) | 12 (15) | 14 (17.5) | 8 (12.1) | 12 (18.2) |
| p-value | 0.1 | 0.6 | 0.3 | |||
| Availability of vaccine for COVID-19 | ||||||
| Incorrect response | 14 (23.3) | 13 (21.7) | 19 (23.8) | 16 (20) | 7 (10.6) | 13 (19.7) |
| Correct response | 46 (76.7) | 47 (78.3) | 61 (76.3) | 64 (80) | 59 (89.4) | 53 (80.3) |
| p-value | 0.8 | 0.6 | 0.03 | |||
| Hot air prevents COVID-19 | ||||||
| Incorrect response | 9 (15) | 9 (15) | 16 (20) | 3 (3.8) | 2 (3) | 3 (4.5) |
| Correct response | 51 (85) | 51 (85) | 64 (80) | 77 (96.3) | 64 (97) | 63 (95.5) |
| p-value | 1.0 | 0.002 | 0.6 | |||
McNemar test.
Bold values are for the significant p-values.
Table 5.
Impact of intervention on the overall knowledge score of dental interns, auxiliaries, and specialists.
| Level of qualificaWWWtion | Pre-intervention Mean (S.D.) |
Post-intervention Mean (S.D.) |
p-value |
|---|---|---|---|
| Interns | 10.18 (2.17) | 12.43 (1.62) | <0.001 |
| Auxiliaries | 10.64 (2.69) | 12.60 (1.67) | <0.001 |
| Specialists | 11.36 (1.81) | 12.35 (1.77) | 0.003 |
| Total sample | 10.74 (2.32) | 12.47 (1.68) | <0.001 |
Paired t-test.
Bold values are for the significant p-values.
Discussion
Due to its inconclusive latency period (ranging from day 1 to day 14) and delayed appearance of symptoms, the COVID-19 outbreak escalated rapidly and has been declared as a global public health emergency on the 30th of January 2020 [19]. The report published on the 27th of April 2020 indicated that more than two million people worldwide are currently affected [3]. The moral obligation of the DHCW's is to treat patients, but it should go hand-in-gloves with the evidence-based-decision making. DHCW's are required to be familiar with the updated concepts of COVID-19 [11]. This is the first study to provide a report on the knowledge of DHCW's; and also, the first study to check the effect of online disseminated information by MoH, Saudi Arabia on the knowledge of COVID-19 among the DHCW's. The findings from the current study demonstrated that the knowledge of COVID-19 among the DHCW's in Saudi Arabia is adequate (above the mean score). But, simple aspects to differentiate between the symptoms of common cold/flu and COVID-19 was not reported correctly by majority of the study participants. The CDC have clearly mentioned in their online brochures that fever, cough, and shortness of breath are the early conditions experienced [20] and till date, sneezing as a symptom of COVID-19 has not yet been established. On the contrary, a similar study performed in Saudi Arabia had found out that the DHCW's did not have adequate knowledge on the standard precautions to be followed for infectious diseases and their transmission [21]. Another study conducted among the DHCW's in Georgia revealed that more than half of the study population (dental students, residents, and specialists) did not possess enough knowledge or awareness on viral infections that are transmitted through human immunodeficiency virus (HIV) and hepatitis-B virus (HBV) [22]. However, there are no comparable findings from earlier studies which have demonstrated a higher level of knowledge on infectious diseases among the DHCW's.
Secondly, there are very few published reports that have segregated the DHCW's based on their level of qualification or their job title (interns vs auxiliaries vs specialists) while assessing the knowledge on viral infections such as COVID-19. The current study has shown that the knowledge score on COVID-19 was significantly related to their level of qualification, and dental specialists displayed the highest knowledge score, followed by dental auxiliaries and dental interns. Contrastingly, one published report investigating the overall infection control knowledge, attitude, and practices; suggested that there was no statistical significant difference between the level of knowledge among the dental students and dental faculty in a university of Saudi Arabia [23].
The current study also demonstrated the effectiveness of the COVID-19 brochure that was disseminated by the Ministry of Health, Saudi Arabia in successfully enhancing the knowledge of DHCW's on the disease. No similar study is currently available to compare these findings, however a study performed among the Oral Health Personnel's in Thailand revealed significant increase in their knowledge level on HIV after an intervention was performed [23]. Also, a randomized control trial to evaluate Acquired Immunodeficiency Disease (AIDS) education intervention program revealed that training workshops are needed in addition to knowledge intervention for the hospital workers [24].
The strength of the current study was the stratification of study sample according to the level of qualification or the job title prior to the analyses. This was done assuming that the dental interns, dental auxiliaries, and the dental specialists possess varying level of educational qualifications and hence their ease of understanding about COVID-19 would not be similar. Thus, a stratified analysis from the current study delivered more comprehensive findings. Next, a computed sample size with an adopted probability sampling technique provided results that were nationally representative. Finally, segregating the DHCW's who did not receive the knowledge from any of the reliable sources was beneficial in obtaining an impeccable result. However, there are certain limitations to the study. Firstly, the study design addressing the primary objective was cross-sectional, and provides lower quality of evidence in comparison to longitudinal studies. Also, the quasi-experiment conducted to address the secondary objective of the study may not be equivalent to a more comprehensive study design such as a randomized control trial. However, it is to note that a longitudinal study and a randomized control trial was not a feasible option with the current situation of social distancing and lockdown being implemented throughout the nation.
Conclusion
In conclusion, the basic knowledge on COVID-19 among the DHCW's in Saudi Arabia is acceptable. Timely dissemination of information by the Ministry of Health, Saudi Arabia had a positive impact on the COVID-19 knowledge score of the DHCW's.
Implications
Although, most of the oral health care settings are closed during the pandemic, a large number of patients with emergency requirements would still be needing dental treatments. A person–person spread has been established and countries have confirmed cases being transferred through healthcare settings [25], [26]. It is recommended to isolate all suspected cases from other patients and healthcare workers and keep a distance of at least 3 feet (1 m). The affected patients should be provided with a mask and the local health authorities should be called immediately [3].
Key points for DHCW's during the COVID-19 pandemic:
-
o
Do not sever ties with your patients, manage remotely (telephone or videocall) by advising them with in-home remedies, oral hygiene instructions, and if required prescribe analgesics and antimicrobials.
-
o
Dental emergency cases should follow the procedure of a telephonic-triage before appearing at the dental practice (Calling-in before Walking-in).
-
o
The receptionist and other auxiliaries should have a readily available diagnostic chart for telephonic-triage that includes a series of questions pertaining to travel history, and the signs and symptoms of COVID-19.
-
o
In the dental practice; protect yourself, colleagues, and the patients from any potential cross-infection by effectively using the personal protective equipment's (PPE).
Author contributions
MFAQ and MAJ designed and implemented the study. AA conducted the intervention. SA, NIO and AAD completed the data collection. MFAQ and SKT completed the data analyses. All authors contributed equally in writing and proof reading the manuscript.
Conflict of interest
The authors do not have any conflict of interest to declare.
Acknowledgements
The authors would like to take this opportunity to thank the dental interns, dental auxiliaries, and dental specialists for participating in this study.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Health emergencies vol. WHO; Geneva: 2020. Rolling updates on corona virus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. [Google Scholar]
- 4.Li Y., Guo F., Cao Y., Li L., Guo Y. Insight into COVID-2019 for pediatricians. Pediatr Pulmonol. 2020;(March) doi: 10.1002/ppul.24734. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;(March) doi: 10.1056/NEJMc2004973. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14(8):523–534. doi: 10.1038/nrmicro.2016.81. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan J.F.-W., Yuan S., Kok K.-H., To K.K.-W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.-L., Abiona O. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi: 10.1038/s41368-020-0075-9. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volgenant C.M.C., de Soet J.J. Cross-transmission in the dental office: does this make you ill? Curr Oral Health Rep. 2018;5(4):221–228. doi: 10.1007/s40496-018-0201-3. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarwar Shah S.G. A commentary on World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;(March) doi: 10.1016/j.ijsu.2020.03.001. [in English] [DOI] [Google Scholar]
- 14.Purcell L.N., Charles A.G. An invited commentary on World Health Organization declares global emergency: A review of the 2019 novel Coronavirus (COVID-19): emergency or new reality? Int J Surg. 2020;76(March):111. doi: 10.1016/j.ijsu.2020.03.002. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MOH, Ministry of Health, Kingdom of Saudi Arabia, Events and activities - Guide on COVID-19, 2020 (visited on 03-03-2020), https://www.moh.gov.sa/en/Ministry/MediaCenter/Pages/default.aspx.
- 16.W.B. Group . 2018. Middle East and North Africa.https://www.worldbank.org/en/region/mena [Google Scholar]
- 17.Sullivan K.M., Dean A., Soe M.M. OpenEpi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep. 2009;124(3 (May–June)):471–474. doi: 10.1177/003335490912400320. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waclawski E. How i use it: survey monkey. Occup Med (Lond) 2012;62(September (6)):477. doi: 10.1093/occmed/kqs075. [in English] [DOI] [PubMed] [Google Scholar]
- 19.Adhikari S.P., Meng S., Wu Y.-J., Mao Y.-P., Ye R.-X., Wang Q.-Z. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(March (1)):29. doi: 10.1186/s40249-020-00646-x. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Center for Disease Control . 2020. Symptoms of Corona virus disease, 2019.https://www.cdc.gov/coronavirus/2019-ncov/downloads/COVID19-symptoms.pdf [Google Scholar]
- 21.Haridi H., Al-Ammar A., MI A.A.-M. Knowledge of dental health care workers’ about standard precautions guidelines at health care facilities in Hail Region, Saudi Arabia. Int J Adv Res. 2016;4(1):1375–1385. [Google Scholar]
- 22.Kochlamazashvili M., Kamkamidze G., McNutt L.A., DeHovitz J., Chubinishvili O., Butsashvili M. Knowledge, attitudes and practice survey on blood-borne diseases among dental health care workers in Georgia. J Infect Dev Ctr. 2018;12(10):864–870. doi: 10.3855/jidc.9911. [in English] [DOI] [PubMed] [Google Scholar]
- 23.Alharbi G., Shono N., Alballaa L., Aloufi A. Knowledge, attitude and compliance of infection control guidelines among dental faculty members and students in KSU. BMC Oral Health. 2019;19(1):7. doi: 10.1186/s12903-018-0706-0. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santana R.T., Monzon O.T., Mandel J., Hall T.L., Hearst N. AIDS education for hospital workers in Manila: effects on knowledge, attitudes, and infection control practices. AIDS. 1992;6(November (11)):1359–1363. [in English] [PubMed] [Google Scholar]
- 25.Ramanathan K., Antognini D., Combes A., Paden M., Zakhary B., Ogino M. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. 2020;(March) doi: 10.1016/S2213-2600(20)30121-1. [in English] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anderson M., Mckee M., Mossialos E. Covid-19 exposes weaknesses in European response to outbreaks. BMJ. 2020;368:m1075. doi: 10.1136/bmj.m1075. [in English] [DOI] [PubMed] [Google Scholar]