Abstract
Background
There is a deluge of information and misinformation about COVID-19. The present survey was conducted to explore the sources of information /misinformation for healthcare professionals from India.
Methods
A cross-sectional online survey using snowballing technique was conducted from 24 Mar to 10 Apr 2020. The questionnaire was pretested and developed using standard techniques. It was circulated among medical students and physicians. Data were analysed using the STATA software.
Results
Data of 758 participants were analysed. A total of 255 (33.6%) medical students, 335 (44.2%) nonspecialists and 168 (22.1%) specialists participated. The most common source of formal and informal information was official government websites and online news, respectively. A total of 517 (68.2%) participants accepted receiving misinformation. Social media and family and friends were the most common sources of misinformation. Seventy-two percent of participants agreed that spread of information helped to contain COVID-19, but more than that 75% agreed to having received inaccurate information. Seventy-four percent of respondents felt the need for regulation of information during such times; 26% and 33% felt that information about COVID-19 made them feel uncomfortable and distracts routine decision-making, respectively, and 50% felt it was difficult to differentiate correct from incorrect information about COVID-19.
Conclusion
The study explored the sources of information and misinformation and found a high prevalence of misinformation, especially from social media. We suggest the need to better manage the flow of information so that it can be an effective weapon against SARS-CoV2. There is a need for doctors to adapt to the changing times of infodemics accompanying pandemics.
Keywords: COVID-19, SARS-CoV2, Pandemic, Infodemic, Misinformation
Introduction
The rules of engagement for COVID-19 are like never before. And it is not only the SARS CoV 2 that is spreading like wildfire but also the accompanying information surge which makes it a different challenge.
The term ‘infodemic’ has been used for the rapid spread of information of all kinds, including unreliable information, rumours and gossip. Infodemics as a term got popular when the World Health Organization (WHO) Director General Tedros Adhanom Ghebreyesus remarked during a speech in the Munich Security Conference on 15 Feb 2020 in the context of COVID-19 – “We're not just fighting an epidemic; we're fighting an infodemic”.1
Studies have documented the spread of information as well as misinformation in the context of COVID-19 across the world. Not only has the rapid spread of information helped to contain the novel virus across countries but also been a source of worry due to the spread of misinformation. Misinformation has been rampant, and Kouzy et al. have reported up to a quarter of tweets related to COVID-19 as misinformation as on 27 Feb 2020.2 Even information given out by government agencies across the world has turned out to be inaccurate at times, leading to more confusion. The dismissal of a warning tweet given out by a young Chinese ophthalmologist warning others about a brewing SARS-like illness by the authorities as a rumour is a reminder of how free flow of information is critical.3
Healthcare personnel are also not immune to infodemics. They too have been bombarded with information about COVID-19 and its pandemic from all sorts of official as well as unofficial sources. The authenticity and veracity of these can vary greatly, given that much of scientific information about COVID-19 is still evolving. They are expected to keep themselves abreast with the latest and evolving knowledge and guidelines as they evolve dynamically. However, so far, little is known about the sources of information the healthcare professionals rely on for acquiring scientific knowledge about COVID-19. Moreover, there are no data in the Indian context where information-seeking behaviour and misinformation channels might be influenced by local factors. Hence, the present survey was conducted to explore the sources of information for healthcare professionals about the COVID-19 pandemic. It also explores the sources of misinformation/inaccurate information the subset was exposed to.
Materials and method
A cross-sectional online survey was conducted among the healthcare personnel in India from 24 Mar 2020 to 10 Apr 2020. The snowballing sampling technique was used for this online survey. In the snowballing sampling technique, research participants recruit other participants of the study. A questionnaire was developed after a literature search and wide consultation amongst experts including epidemiologists and medical educationists. The questionnaire was converted and uploaded onto Google Forms. The first 30 respondents administered the survey in the presence of investigators, and feedback was taken in the form of loud thinking. The forms were modified after their feedback. The forms were then pilot-tested in another 50 respondents, and their responses were analysed and changes made in the form based on the analysis and feedback received from the participants. Email ID was used as a unique identifying field to avoid multiple submissions.
The final survey instrument was widely circulated among healthcare workers. The submission of form was taken as consent of the participant. Confidentiality of the data was maintained, and data were analysed as group data. The study was approved by the institutional ethics committee of the institute.
The healthcare workers who responded were divided into three groups based on their educational status as follows - medical students and medical practitioners who were nonspecialists and specialists.
It was assumed that 42.2% of the respondents would be misinformed based on a study by Kouzy et al.2 The sample size was calculated assuming a degree of absolute precision as 5% and 95% confidence interval as 384. However, it was decided to enrol as many participants as possible in the study over the minimum sample size.
The categorical data were described as number and percentages. The Chi-square test was used as a measure of association. The statistical analysis was carried out using StataCorp. 2013, Stata Statistical Software: Release 13 (StataCorp LP, College Station, TX). The p value of less than 0.05 was taken as statistically significant.
Results
The online survey was conducted from 24 Mar 2020 to 10 Apr 2020. A total of 778 forms were received, out of which 20 forms were incomplete, and hence, data of 758 participants were analysed.
The sociodemographic distribution of the participants is given in Table 1.
Table 1.
Characteristics of study population.
| S no | Characteristic | N, percentage | 95% CI |
|---|---|---|---|
| 1. | Age, years | ||
| <18 | 10 (1.3%) | 0.6%–2.4% | |
| 18-24 | 329 (43.4%) | 39.8%–47.0% | |
| 25-34 | 194 (25.6%) | 22.5%–28.8% | |
| 35-44 | 120 (15.8%) | 13.3%–18.6% | |
| 45-54 | 70 (9.2%) | 7.2%–11.5% | |
| 55-64 | 26 (3.4%) | 2.3%–4.9% | |
| >65 | 9 (1.2%) | 0.5%–2.2% | |
| 2. | Sex | ||
| Female | 291 (38.4%) | 34.9%–41.9% | |
| Male | 467 (61.6%) | 58.0%–65.1% | |
| 3. | Medical students | 255 (33.6%) | 30.2%–37.1% |
| Doctors/practitioners | 503 (66.4%) | 62.8%–69.7% | |
| Nonspecialist | 335 (44.2%) | 40.6%–47.8% | |
| Specialist | 168 (22.1%) | 19.3%–25.3% | |
| 4. | Misinformation received | ||
| Yes | 517 (68.2%) | 64.8%–71.5% | |
| No | 241 (31.8%) | 28.5%–35.2% | |
Sources of information
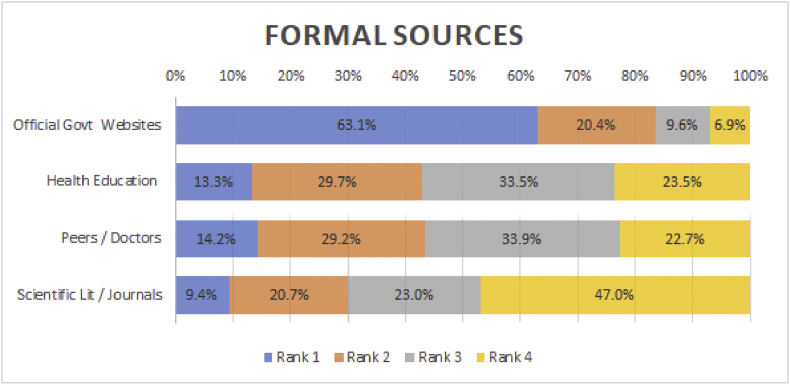
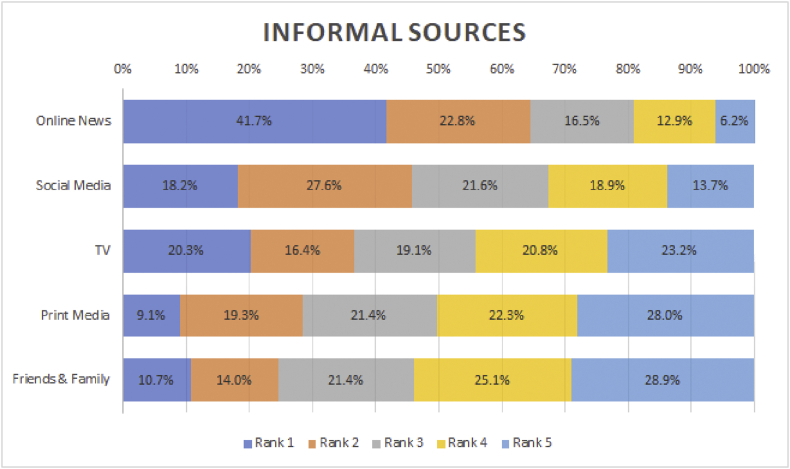
The rankings of formal and informal sources of information are given in Fig. 1 and Fig. 2, respectively. Among formal sources, official government websites were ranked first by 63.1% of respondents, while scientific journals were ranked first only by 9.4% of the respondents. In informal sources, online news was ranked first by 41.7% and second by 22.8%. Social media was the overall second choice, with 45.8% or respondents giving it either first or second rank. Television (TV), print media and friends and families were ranked 3, 4 and 5, respectively.
Fig. 1.
Formal sources of information.
Fig. 2.
Informal sources of information.
When data were analysed groupwise, more practitioners preferred the official Government/WHO site as their first choice than medical students (p = 0.03). Similarly, for informal sources, specialists preferred online news than undergraduate students, while students preferred family and friends as the first choice more often than the other two groups, specialists and nonspecialists (p = 0.007).
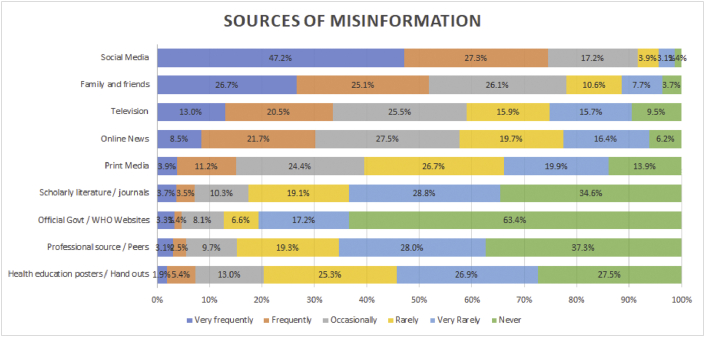
Sources of misinformation
Of all, 68.2% (95% CI: 64.8%–71.5%) respondents gave answers in affirmative for receiving misinformation. There was no statistical difference in any group as per prevalence of misinformation. However, the prevalence was higher in the student's group (72.7% vs 65.7% in nonspecialist and 66.1% in the specialist group [p = 0.01]). The sources of misinformation are given in Fig. 3. ‘Social media’ and ‘family and friends’ were ranked first and second, respectively, as sources of misinformation by majority of respondents (47.2% and 26.7%, respectively). There were no statistically significant intergroup differences in any of the sources of misinformation.
Fig. 3.
Sources of misinformation. WHO, World Health Organization.
There was an open-ended questionnaire about providing examples of misinformation that they received. Most of the misinformation was about various treatment options of COVID-19, followed by vaccination, spread and killing of viruses. Few respondents mentioned “kafoor/laung/elaichi (camphor, cloves and cardamom) as a cure for COVID-19 being propagated on TV”. Another respondent wrote “Vibrations can kill viruses”. Some respondents reported receiving misinformation about a “Breath holding test” as a self-diagnostic test of COVID-19.
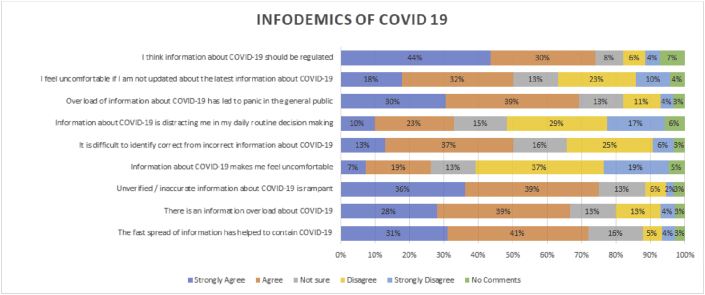
Questions about infodemics
Questions about the infodemics of COVID-19 were part of the survey instrument. The responses gathered in Likert scale are depicted in Fig. 4. Sixty-seven percent and 75% of all respondents either agree or strongly agree about information overload and inaccurate information, respectively. Fifty percent of the respondents agree/strongly agree that it is difficult to differentiate correct from incorrect information. Twenty-six percent and 33% agree/strongly agree that information about COVID-19 makes them feel uncomfortable and distracts routine decision-making, respectively. However, 50% also feel uncomfortable when not updated about information on COVID-19. For utility of information, 72% agree that spread of information helped to contain COVID-19. At the same time, 74% participants feel that information about COVID-19 should be regulated.
Fig. 4.
Infodemics of COVID-19.
There were no differences in distribution of answers of the subgroups except for nonspecialists who felt that information about COVID-19 distracted them from their routine work compared with other groups (p = 0.02). Both specialists and nonspecialists felt that lack of updated information about COVID-19 made them feel uncomfortable as compared with students (p < 0.001).
Discussion
It has often been said – ‘Information is power’, but is more information more power? What is misinformation then? This would not have been a question linked to the medical profession, but add to it COVID-19, and the whole context changes! In the era of technology and social media, both information and misinformation flow faster and wider than ever before, much like SARS CoV 2. The pandemic of COVID-19 has led to an infodemic, with healthcare professionals searching the Internet for more and more information regarding the etiological agent, the clinical features of disease, its management and the public health measures to be undertaken to control the spread of the epidemic.4
Although the medical profession has been part of this infodemic perhaps as much as the pandemic itself, there is scarcity of scientific literature which has documented these trends especially in India. The present study attempts to survey them to have a better understanding of information-gathering behaviour of the medical community. To the best of our knowledge, this is the largest study on infodemics among the medical profession in India.
Information
The sources of information were divided into formal and informal. This is because of the thought process that although each type of source is complementary to each other, it does not usually replace the other.
In the formal sources, official government websites are the preferred mode for a large majority of our study population (Fig. 1). Arguably, the response of the official and government information portals has been rapid and has kept pace with frequent and accurate information. At the national level, various official government portals led by the Ministry of Health and Family Welfare, Govt of India, are providing up-to-date and current information on their websites and social media channels. Internationally too, various portals led by the WHO and Centers for Disease Control and Prevention (CDC) are providing credible information.5
Hernandez-García et al. studied the available information on the Internet about COVID-19 and its adherence to the standard guidelines available on official websites of the WHO and CDC.6 They found that various aspects of preventive measures advocated by the WHO or CDC were found in only 32.5–81.3% of the studied web links on the Internet. They suggested that official sources of regional/national governments should provide correct information about COVID-19 that conforms to the standard guidelines issued by the WHO/CDC and provide links to the same on other popular websites on the Internet.6
The role of scientific journals requires a closer look. Despite the majority of the respondents being doctors, only 9% ranked it on top. This is despite the fact that many journals have fast-tracked publications related to COVID-19 and made them open access. It was reported that at least 54 academic articles about COVID-19 were published by 30 Jan 2020 itself.7 The reasons for poor acceptability of medical journals as an information source are not well understood. We tried to search for data related to professional reading habits of medical professionals for India but were unable to get a satisfactory answer. Perhaps, the factors may be many – a perceived difficulty to interpret research articles, ease of availability of information by other channels and maybe even a lack of access.
For informal sources, online news ranked first for most respondents (Fig. 2). This is not surprising with the majority of the study population belonging to a younger age group where primary news sources are online.8 Social media again did not disappoint and was ranked second as a source. Social media has over the years established as a well-recognised source of information exchange.9 Age less than 40 years is associated with a higher usage of social media in the healthcare community.10 Despite the fact that social media has been often implicated for misinformation, it plays an important role in dissemination of information in emergencies and may prove to be a game changer in times of crises.11
Misinformation
With so much information being circulated about COVID-19 on various online social media and news platforms, it is important that it be factually correct and scientifically validated, so as not to cause harm to the recipient or the population. However, this is often not true and circulation of large amounts of inaccurate, unverified and false information is rampant. This problem has been identified in the past, and such information has been classified into misinformation and disinformation. Misinformation refers to false information which is shared without any intention of causing harm, while disinformation is fake information which has been deliberately created and shared to cause harm.12,13 The present study limits itself to misinformation only.
The magnitude of false information about COVID-19 can be estimated from the fact that 68.12% of respondents in the present study identified receiving information they deem to be partially or completely inaccurate. Majority of such inaccurate information has been recognised by the participants to be received from ‘social media’ and ‘family and friends’ (47.2% and 26.7%, respectively) (Fig. 3). Our results are similar to those in the existing literature and understanding on the subject of misinformation. Kouzy et al. studied the magnitude of spread of misinformation about COVID-19 on Twitter.2 Amongst the tweets being shared regarding COVID-19, up to a quarter (24.8%) of all were found to have misinformation and another 17.4% were found to have unverified information regarding COVID-19.2
In the present study, an attempt was made to elicit the sources of inaccurate information implicated in an optional open-ended question. Of all, 70.02% of those who reported receiving inaccurate information named ‘WhatsApp’ as the main source. This is perhaps due to a greater number of users on this platform. Facebook and WhatsApp have significant penetration amongst digital users in India compared with Twitter in accordance with a recent report.14 In addition, it may not be easy to measure the usage of peer-to-peer networks in a scientific manner because of privacy concerns/lack of access as compared with Twitter.
The implications and dangers of misinformation are significant and merit a deeper understanding. The dangers of misinformation are also not limited to social media as identified by Cuan-Baltazar et al. who analysed 110 Internet sources of information in the early days of the pandemic related to COVID-19 and found that the vast majority did not meet standard criterion and validated benchmarks online evaluating health resources.4 Additionally, they recommended government agencies should consider the use of a regulatory mechanism to control false or misleading health information.4
Another insight is provided by a study conducted in South Korea regarding the Middle East Respiratory Syndrome (MERS) epidemic, highlighting the unique role of both traditional and social media. They comment that although traditional media has a positive influence on users acquiring knowledge, it did not translate to behavioural change unlike on social media.15
Misinformation related to health care can have greater implications by delaying appropriate care and affecting the health of the community. Wang et al. investigated published literature on misinformation related to health and its online spread in the pre-COVID-19 era.12 They found an abundance of literature about the spread of misinformation related to infectious diseases and vaccination, more than they did about accurate information.12 They point out the harmful effects of social misinformation on nationwide campaigns such as Measles, Mumps and Rubella (MMR) vaccination in the past. In another recent commentary, the authors go to the extent of warning how misinformation created an “optimal environment for anti-science groups to gain footing and propagate false theories and information”.16
What the respondents felt?
Interesting results were obtained on questions related to COVID-19 (Fig. 4). Most feel that there is too much information about COVID-19 floating in the environment; and unfortunately, a larger percentage felt the same way about misinformation! This is the phenomenon of misinformation following information, something well known since long and only amplified by technology now.12 This is not surprising in the current time of Internet-based communication as in the case of the Ebola epidemic, aptly described by some as fighting multiple epidemics – calling them ‘secondary virtual epidemics’!17
The ability to differentiate between correct and incorrect is not an easy task, especially when information is rapidly changing and evolving. What is more striking is that even amongst medical professionals, almost 50% of the respondents of the present study find it troublesome to sift what is validated and correct. To what degree the common population is able to differentiate technical medical knowledge is only a matter of speculation, but their aptitude is expected to be much lower.
Does this tsunami of information cause anxiety among us? Although the majority does not seem to suggest so, 26% and 33% of our study group agree that information about COVID-19 makes them feel uncomfortable and distracts routine decision-making, respectively. A recent Chinese study exploring mental health of the general population during COVID-19 reports anxiety in up to 28.8% and depression in 16.5% of the population which persists more than four weeks using a validated questionnaire.18 Rao et al. report a similar prevalence of anxiety in the Chinese population (22.6%) during the outbreak, and frequent use of social media was positively associated with high odds of anxiety (odds ratio: 1.72).19 Indian data on the mental health of the population are yet to emerge, but we should be forewarned of an impending mental health epidemic which might follow.
These are ‘fear of missing out’ (FOMO) times, and it is not uncommon to see people trying to keep updated on the latest figures, studies and information about COVID-19.20 In fact, in the present survey, 50% also feel uncomfortable when not updated about information on COVID-19. The FOMO construct typically linked to excessive social media usage as a means of self-gratification has probably spread to include a fear of impending bad news!
Considering the fact that so much misinformation is prevalent, should information about COVID-19 be regulated? An overwhelming majority (74%) of our participants do think so. Already, provisions do exist in the law to fight fake news amidst COVID-19. The Information Technology Act, 2000 and the rules around the Act have the scope to factor in many situations of violations.21 In addition, there is the additional advantage of the provisions of Section 54 of the Disaster Management Act 2005 (DMA) – which deals with false warnings around a disaster leading to panic,22 Sections 505 and 188 of the Indian Penal Code23 and Section 3 of the Epidemic Disease Act 1897.24 Perhaps it is the implementation of the existing provisions of the law that need to be strengthened. Awareness about these laws too should be improved if we need to effectively regulate the misinformation.
Despite the widely held view that information spread during such emergencies needs to be regulated, information itself is an important weapon to fight the spread of such diseases. In fact, 72% of the present survey respondents suggest that spread of information has helped to contain COVID-19. In China, Internet searches and social media data have been reported to correlate with traditional surveillance data and could even predict the outbreak of disease epidemics several days or weeks earlier.25 In the 2009 H1N1 outbreak, a content analysis of more than 2 million tweets reported only 4.5% of tweets as misinformation.26 In their study, they report that H1N1 pandemic–related tweets on Twitter were primarily used to disseminate information from credible sources to the public and a rich source of opinions and experiences. As more data about infodemics of COVID-19 are published, knowledge about the importance of information as compared with misinformation will emerge.
In the present study, nonspecialists felt that information about COVID-19 distracted them from their routine work compared with other groups (p = 0.02). This probably reflects a limited exposure to medical information in this group, leading to an increased anxiety about the disease. Perhaps the consideration that they will be the first to attend to such patients in an unprotected way in the early phase of disease might also play a role.
Both specialists and nonspecialists felt that lack of updated information about COVID-19 made them feel uncomfortable as compared with students (p < 0.001). This might reflect an understanding that they would need to actually attend to COVID-19 patients compared with the students and therefore need to be updated. In addition, they are often information providers to their patients and community for which there is a natural obligation to keep abreast of the latest developments.
Limitations of the study
Admittedly, there are a few limitations of the present study. The study was conducted among a literate and specified population who has access to Internet connection. Hence, generalisability of the study is limited. Sampling bias may have occurred owing to the snowballing technique; however, it is the most commonly used sampling technique in online surveys. An inherent problem of any survey-based study is the difficulty in validating the responses. There is an assumption that the respondent has answered to the best of his/her knowledge which may itself be inaccurate at times. Thus, the interpretation of misinformation by the respondents may not be very accurate especially in the case of medical students.
Conclusion and recommendations
To conclude, the present study sheds light on the infodemics of COVID-19 amongst healthcare professionals in India. The most common sources of information about COVID-19 were government websites and online sources. Misinformation is rampant even amongst doctors. The present study highlights social media as an important source of misinformation and perhaps needs better regulation. Many of the healthcare workers find it difficult to differentiate between authentic and nonauthentic information. Nevertheless, most respondents felt that rapid spread of information helped in controlling the spread.
Therefore, we have a deluge of information and misinformation and multiple channels of communications happening in a global medical emergency. It cannot be emphasised more that fast and accurate information is very much an essential part of the battle against COVID-19. The restriction of information flow may be counter-productive. The challenge is to then manage this flow of information so that it can be an effective weapon against SARS-CoV2. For the medical community, this should be met at both individual and institutional levels.
All medical doctors have a role to screen the information that they have received before further posting it. It is imperative that they are trained for identifying to separate the wheat from the chaff when faced with suspected inaccurate information. In the current infodemic, social media has emerged as a double-edged sword. This is a fight for the attention span of the recipient of information and needs to be tailored accordingly. The information should be easy to understand, verifiable information and credible. A lack of information leaves a vacuum, and misinformation soon takes over. It is essential not to fall prey to a misinformation campaign and hit the share button. Social media networks themselves have mechanisms to halt such campaigns, but more often than not, it is too late by the time they are detected.27
At an institutional level, the medical community needs to look at these results carefully and adapt itself to these new paradigms. There is a need to develop information ethics in disaster situations, epidemics and pandemics incorporating the way information spreads fast and easy. Standards/benchmarks need to be set to encourage the spread of accurate medical information and mitigate the spread of misinformation. Experts in crisis communication should work in the affected places and help draft information which is relevant to the area. Best practices need to be shared globally. The WHO has published guidelines on ‘Communicating risk in public health emergencies’ which provide evidence-based guidance on how risk communication should be practised in an emergency and suggested capacity building process for the same.28 Similarly, the Crisis and Emergency Risk Communication (CERC) manual by the CDC provides a framework and best practices for anyone who communicates on behalf of an organisation responding to a public health emergency and provides steps of the communication process in such a scenario.29 There is perhaps a need to develop a special module suited to our country which may be a part of the curriculum of all healthcare workers so that they become a ready resource subsequently as an important part of information management.
The importance of communications during such health emergencies has been succinctly put forth in a Tweet by Dr. Heidi Tworek, an assistant professor of international history at the University of British Columbia, Vancouver, Canada, who remarks “Communications in a public health crisis are as crucial as medical intervention. In fact, communications policies ARE a medical intervention.”30 The medical profession needs to evolve. Much like Web 2.0, this is ‘Public Health 2.0’!
Disclosure of competing interest
The authors have none to declare.
References
- 1.Munich Security Conference [Internet] https://www.who.int/dg/speeches/detail/munich-security-conference [cited 2020 Apr 19]. Available from:
- 2.Kouzy R., Abi Jaoude J., Kraitem A. Coronavirus goes viral: quantifying the COVID-19 misinformation epidemic on twitter. Cureus. 2020;12 doi: 10.7759/cureus.7255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larson H.J. Blocking information on COVID-19 can fuel the spread of misinformation. Nature. 2020;580:306. doi: 10.1038/d41586-020-00920-w. [DOI] [PubMed] [Google Scholar]
- 4.Cuan-Baltazar J.Y., Muñoz-Perez M.J., Robledo-Vega C., Pérez-Zepeda M.F., Soto-Vega E. Misinformation of COVID-19 on the Internet: Infodemiology Study. JMIR Public Heal Surveill [Internet] 2020;vol. 6(2) doi: 10.2196/18444. http://www.ncbi.nlm.nih.gov/pubmed/32250960 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zarocostas J. How to fight an infodemic. Lancet (London, England) 2020;395:676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernández-García I., Giménez-Júlvez T. Assessment of health information about the prevention of COVID-19 on the Internet. JMIR Public Heal Surveill. 2020;6 doi: 10.2196/18717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stoye E. China coronavirus: how many papers have been published. Nature. 2020;30:2020. doi: 10.1038/d41586-020-00253-8. [DOI] [PubMed] [Google Scholar]
- 8.Westlund O., Färdigh M.A. Accessing the news in an age of mobile media: tracing displacing and complementary effects of mobile news on newspapers and online news. Mobile Media Commun. 2015;3:53–74. [Google Scholar]
- 9.Rolls K., Hansen M., Jackson D., Elliott D. How health care professionals use social media to create virtual communities: an integrative review. J Med Internet Res. 2016;18:e166. doi: 10.2196/jmir.5312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Surani Z., Hirani R., Elias A. Social media usage among health care providers. BMC Res Notes. 2017;10:654. doi: 10.1186/s13104-017-2993-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muniz-Rodriguez K., Ofori S.K., Bayliss L.C. Social media use in emergency response to natural disasters: a systematic review with a public health perspective. Disaster Med Public Health Prep. 2020;14:139–149. doi: 10.1017/dmp.2020.3. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y., McKee M., Torbica A., Stuckler D. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med. 2019;240:112552. doi: 10.1016/j.socscimed.2019.112552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thai M.T., Wu W., Xiong H. CRC Press; 2016. Big Data in Complex and Social Networks. [Google Scholar]
- 14.India: Social Media Penetration Statista [Internet] 2020 https://www.statista.com/statistics/284436/india-social-network-penetration/ [cited 2020 Apr 19]. Available from: [Google Scholar]
- 15.Seo M. Amplifying panic and facilitating prevention: multifaceted effects of traditional and social media use during the 2015 MERS crisis in South Korea. J Mass Commun Q. 2019 [Google Scholar]
- 16.Mian A., Khan S. Coronavirus: the spread of misinformation. BMC Med. 2020;18:1–2. doi: 10.1186/s12916-020-01556-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allgaier J., Svalastog A.L. The communication aspects of the Ebola virus disease outbreak in Western Africa--do we need to counter one, two, or many epidemics? Croat Med J. 2015;56:496. doi: 10.3325/cmj.2015.56.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang C., Pan R., Wan X. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao J., Zheng P., Jia Y. 2020. Mental Health Problems and Social Media Exposure during COVID-19 Outbreak. Available SSRN 3541120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Casale S., Flett G.L. Interpersonally-based fears during the COVID-19 pandemic: reflections on the fear of missing out and the fear of not mattering constructs. Clin Neuropsychiatr. 2020;17:88–93. doi: 10.36131/CN20200211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Information Technology Act Ministry of Electronics and Information Technology, Government of India [Internet] 2000. https://meity.gov.in/content/information-technology-act-2000 [cited 2020 Apr 19]. Available from:
- 22.The Disaster Management Act 2005. https://www.ndmindia.nic.in/images/The Disaster Management Act, 2005.pdf [Internet]. Available from:
- 23.Indian Penal Code [Internet] http://legislative.gov.in/sites/default/files/A1860-45.pdf [cited 2020 Apr 20]. Available from:
- 24.The Epidemic Diseases Act 1897. https://indiacode.nic.in/bitstream/123456789/10469/1/the_epidemic_diseases_act%2C_1897.pdf [Internet]. [cited 2020 Apr 20]. Available from:
- 25.Li C., Chen L.J., Chen X., Zhang M., Pang C.P., Chen H. Retrospective analysis of the possibility of predicting the COVID-19 outbreak from Internet searches and social media data, China, 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.10.2000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chew C., Eysenbach G. Pandemics in the age of Twitter: content analysis of tweets during the 2009 H1N1 outbreak. PloS One. 2010;5 doi: 10.1371/journal.pone.0014118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brennen J.S., Simon F.M., Howard P.N., Nielsen R.K. 2020. Types, Sources, and Claims of COVID-19 Misinformation. [Google Scholar]
- 28.Communicating Risk in Public Health Emergencies A WHO Guideline for Emergency Risk Communication (ERC) Policy and Practice. [PubMed]
- 29.CERC Manual, Crisis & Emergency Risk Communication (CERC) https://emergency.cdc.gov/cerc/manual/index.asp [Internet]. [cited 2020 Apr 19]. Available from:
- 30.Heidi Tworek on Twitter . Fact, Communications Policies ARE a Medical Intervention. We Can do Much Better So Here Goes: (1/25)”/Twitter [Internet] 2019. A thread: communications in a public health crisis are as crucial as medical intervention.https://twitter.com/HeidiTworek/status/1240340632666701824 [cited 2020 Apr 19]. Available from: [Google Scholar]