Abstract
Introduction
Hallux valgus surgery is one of the most commonly performed operations in Orthopaedics. Multiple surgical techniques have been described including arthrodesis, osteotomies and soft tissue procedures. The endoscopic-assisted distal soft tissue procedure is one of the minimally invasive surgical options with a good long-term outcome. The rehabilitation protocol for this soft tissue procedure consists of 6-weeks of non-weight bearing walking. This prolonged period of non-weight-bearing walking may ensure a good stabilization of the alignment but is difficult for the patient from a social-economical perspective. In addition, earlier mobilisation has other theoretical advantages including less atrophy and better range of motion. The objective of this trial is to investigate the effect of an earlier weight-bearing regime at 2-weeks post-surgery.
Methods
Randomised control trial of patients undergoing the endoscopic-assisted distal soft tissue procedure. Allocation and randomization of subjects were performed immediately after completion of surgery to avoid intra-operative biases. The control group underwent the usual protocol of 6-weeks of non-weight-bearing walking while the intervention group underwent 2-weeks of post-operative non-weight-bearing walking. Foot function was measured using the Foot and Ankle Outcome Score (FAOS) at the baseline, 12-week post-surgery and 26-weeks post-surgery. The hallux valgus angle, 1,2 inter-metatarsal angle and tibial sesamoid position were also measured during those time-points.
Results
A total of 51 participants completed the study, 29 in the control group and 22 in the early weight-bearing group. 1 patient form the early weight-bearing group was complicated with hallux varus requiring revision surgery. All the patients had significantly improved radiological angles and foot function in both the control and early weight-bearing group. At the 12-week time point, the radiological angles were the same for both groups but foot function was significantly better in the early weightbearing group.
Discussion
Early postoperative weight-bearing did not lead to pre-mature implant failures or increased recurrence rates. It actually resulted in fewer symptoms like stiffness, lessened pain, better performance in daily activities and a better quality of life.
Conclusion
Early weight-bearing walking at 2-week after distal soft tissue reconstruction of hallux valgus is not only safe, it may help accelerate the rehabilitation process and allow patients to return their usual life faster.
The translational potential of this article: Being a clinical trial, our results are directly translatable to hallux valgus patients. The results of this study show that a shortened non-weight bearing duration after hallux valgus surgery improves foot function at 12 weeks while not affecting recurrence risks.
Keywords: Bunion, Foot, Hallux valgus, Rehabilitation, Surgery
Introduction
Hallux valgus is one of the most common pathologies seen by the orthopaedic surgeon [[1], [2], [3]]. There are multiple surgical procedures with different rehabilitation regimes [[4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18]]. Surgery can be broadly classified into the fusion procedures such as the Lapidus [19], first metatarsal osteotomy procedures like the chevron osteotomy [4,5,20] and soft tissue reconstruction procedures like the McBride [2,11]. Sometimes these procedures can be performed in tandem, sometimes they can be standalone procedures.
The endoscopic/arthroscopic-assisted distal soft tissue procedure is a minimally invasive soft tissue reconstruction surgery with good 10-year outcomes [21]. It is a combination of releasing the contracted lateral soft tissue, a fluoroscopic guided bunionectomy, tightening of the lax medial structures and closure of the 1,2 intermetatarsal space using a distal inter-metatarsal cerclage suture and a proximal 3.5 mm screw between the 1st and 2nd metatarsal.
This endoscopic-assisted distal soft tissue procedure is the default surgery in the author's unit with a typical rehabilitation regime of 6 weeks of non-weight bearing walking (Fig. 1) followed by 6 weeks of heel walking and subsequent resumption of normal full weight-bearing walking at 12 weeks [18]. A 6-week course of non-weight bearing walking is a major problem as many patients find it difficult to take so much time off work for elective surgery, thus many of them defer surgery until the symptoms become unbearable.
Figure 1.
Photo showing a Physiotherapist demonstrating the proper technique of Right-sided non-weight bearing walking using crutches. As shown in the photo, both upper limbs need to be engaged during non-weight bearing walking making routine daily tasks (such as carrying a cup of coffee) difficult.
Prolonged protected weight-bearing theoretically decreases implant failure (such as early loosening of the 3.5 mm positional inter-metatarsal screw at the proximal metatarsal) and recurrence rates [22]. This cautious approach of a 6-week course of non-weight bearing walking (similar to the rehabilitation after foot fracture osteosynthesis) was adopted since the introduction of the endoscopic-assisted distal soft tissue procedure technique in the early 2000s. Aside from being more welcome by patients, the authors believe that early mobilization may help decrease swelling, lessen atrophy, and improve range of motion [23]. From our observation, the long-term outcome for the endoscopic-assisted distal soft tissue reconstruction is good, but some patients complain of swelling and stiffness during the initial few months [21]. This discomfort often resolves after the resumption of normal weight-bearing ambulation at ~4-months post-surgery.
Finding the earliest safe time to allow ambulation formed the basis of this study.
Hypothesis
Early ambulation with heel walking at 2-week will not increase recurrence rates. Early mobilization will decrease post-operative pain and swelling as well as accelerate the rehabilitation.
Methods
This is an open-label randomized controlled trial.
ClinicalTrials.gov ID: NCT03340415 and Ethics approval CREC 2018.202-T.
Subjects were recruited from Aug 2018–July 2019 at in a General Hospital in Hong Kong.
Eligibility
Inclusion criteria
Undergoing the Endoscopic-assisted distal soft tissue procedure for hallux valgus correction [21]. Mentally and legally capable of consent to participate in this study.
Exclusion criteria
Disabilities (both physical and mental) which may impair the adherence of the rehabilitation and those who have concomitantly undergone additional procedures on the same foot.
Intervention
The control group will follow the existing protocol of non-weight bearing walking for 6-weeks before the resumption of partial-weight bearing walking for 6-week then full weight-bearing walking at 12-weeks post-surgery.
The early weight-bearing group will have 2-weeks of non-weight bearing following surgery followed by 10-weeks of partial weight-bearing and resumption of full weight-bearing walking at 12-week post-surgery.
Outcomes
Foot function was measured using the FAOS at the baseline, 12-weeks and 26-weeks [24]. The FAOS consists of 5 subscales ranged from 0 (extreme symptoms) to 100 (no symptoms); the 5 subscales are symptoms, pain, the activity of daily living, recreation (sports) and quality of life. Weight-bearing x-rays of bilateral feet were taken at the baseline, 12-weeks and 26-week intervals. Hallux valgus angle, 1,2 intermetatarsal angle and the tibia sesamoid position was measured and documented.
A sample size of 40 was calculated using the Foot and Ankle Outcome Score (FAOS) [24]. This figure was calculated using the reported minimally clinically important change of 8–10 for the FAOS. Using this figure as a therapeutic effect, a mean difference of 8 with a standard deviation of 15, 40 subjects were required for a 95% power at a level of 0.05 with an effect size of 0.53 (G∗power 3.1.9.4).
Allocation
Participants were randomized into the control or intervention group via using a computer-generated number immediately after the surgery (in the recovery room) to reduce intra-operative surgeon bias. We were unable to blind the participant or assessors.
All data were analyzed using SPSS 25 (IBM, USA) and Excel 2016 (Microsoft, USA). Independent sample t-tests were used to calculate the HVA, 1,2 IMA, tibial sesamoid position and the 5 FAOS subscale comparison at baseline, 12-weeks and 26-weeks.
Results
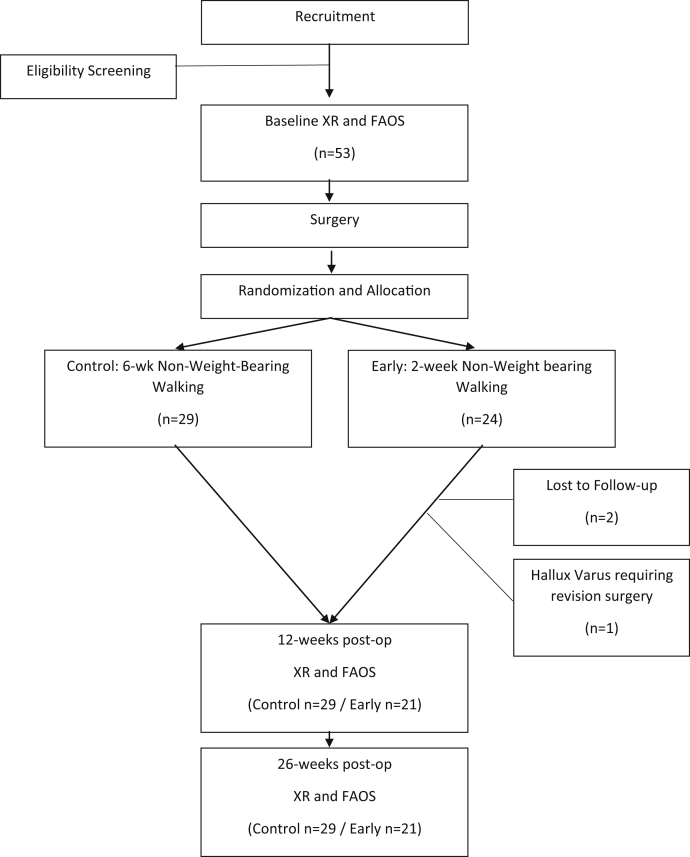
53 patients were recruited; 29 were randomized into the control group while 24 were randomized into the early weight-bearing group (Fig. 2). 2 participants, both from the early weight-bearing group, were lost to follow-up. 1 participant in the early 2-week weight-bearing group was complicated with hallux varus and required revision surgery at 2-week after the index operation. 51 participants completed the 26-week follow-up. 46 were females and 5 were males, 23 Left feet and 18 right feet were operated on. Comparable radiological angles was seen between the 2 groups at all the time points (Table 1). Both groups of participants had significant improvement between the pre-operative radiographs and 26-week radiographs. This radiological improvement also translated to clinical improvement as evidenced by the significant improvement in foot function score from baseline to 26-week in both groups (Table 2) (Fig. 3). Comparison of the Control and Early weight-bearing group showed no difference at the baseline (Fig. 4) and final 26-week score (Fig. 5).
Figure 2.
CONSORT diagram.
Table 1.
Table showing no significant radiological difference between the 2 groups at the baseline, 12-week and 26-week time-points.
| Radiological measurements | 0-week |
12-week |
26-week |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 6-week NWB | 2-week NWB | P-value | 6-week NWB | 2-week NWB | P-value | 6-week NWB | 2-week NWB | P-value | |
| Hallux Valgus Angle | 35.6 ± 7.1 | 37.4 ± 8.0 | 0.89 | 8.8 ± 5.2 | 7.2 ± 4.8 | 0.49 | 11.6 ± 7.6 | 10.5 ± 6.2 | 0.35 |
| 1,2 Intermetatarsal angle | 14.0 ± 3.0 | 16.4 ± 3.7 | 0.35 | 6.2 ± 1.9 | 7.2 ± 2.2 | 0.78 | 7.7 ± 2.7 | 7.3 ± 2.4 | 0.35 |
| Tibial Sesamoid position | 5.55 ± 1.2 | 5.6 ± 1.1 | 0.90 | 2.6 ± 1.2 | 3.0 ± 0.9 | 0.10 | 2.9 ± 1.3 | 3.0 ± 1.0 | 0.46 |
P-values are represented as italics.
Table 2.
Table showing significant improvement in the foot function score in both groups at 26-weeks compared to the pre-operative baseline. The Foot and Ankle Outcome Score (FAOS) is splint into 5 categories with a range from 0 to 100, a score of 100 = asymptomatic while 0 = severe problems.
| Foot and Ankle Outcome Score | Control 6-wk NWB |
Early 2-wk NWB |
||||
|---|---|---|---|---|---|---|
| Baseline | Final | P-value | Baseline | Final | P-value | |
| Symptoms | 58.3 | 81.9 | ∗0.00 | 47.5 | 80.5 | ∗0.00 |
| Pain | 44.0 | 82.2 | ∗0.00 | 47.5 | 85.5 | ∗0.00 |
| ADL | 59.7 | 84.3 | ∗0.00 | 53.0 | 86.0 | ∗0.00 |
| Sport | 52.1 | 76.7 | ∗0.00 | 39.8 | 77.6 | ∗0.01 |
| QOL | 41.2 | 82.4 | ∗0.00 | 31.1 | 81.4 | ∗0.00 |
P-values are represented as italics.
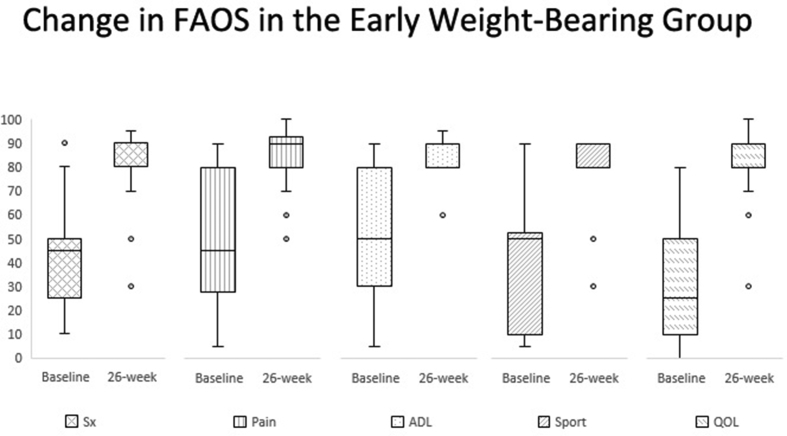
Figure 3.
Significant improvement in the Foot and Ankle Outcome Score was noticed at the 26-week mark from the baseline in the early-weight bearing group.
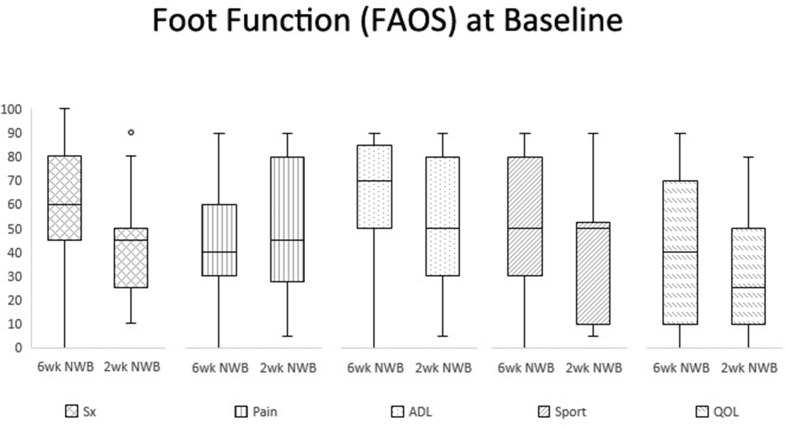
Figure 4.
Both groups had similar baseline Foot and Ankle Outcomes Scores (FAOS).
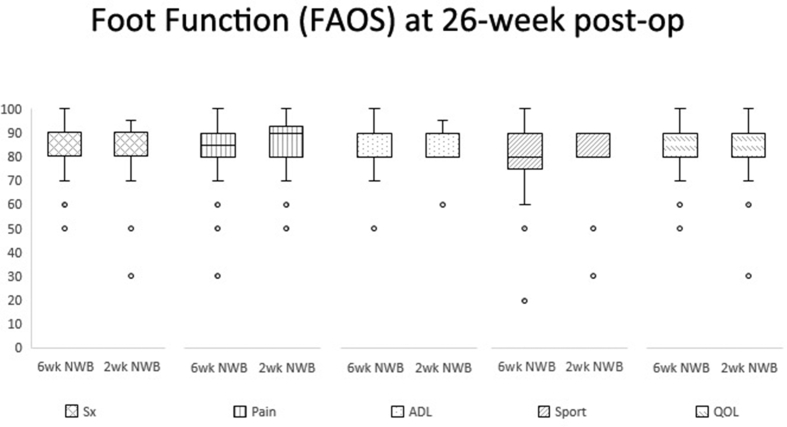
Figure 5.
This figure shows that both groups had a similarly good 26-week foot function after undergoing the endoscopic-assisted distal soft tissue procedure.
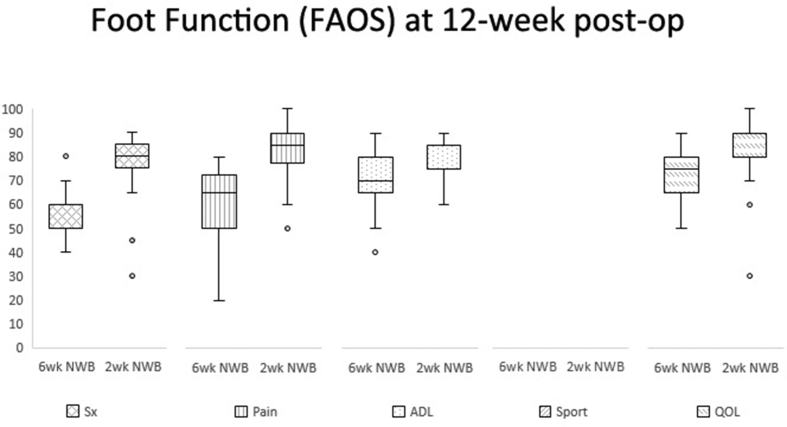
However, there were significant differences in foot function during the assessment at the 12-week mark in all the subscales (except for Sporting activities which was not recorded since most patients have not yet resumed sports) (Table 3). The accelerated 2-week weight-bearing group had significantly better symptoms, less pain, better general function and improved quality of life at the 12-week interval. None of the participants returned to sporting activities at 12-weeks thus the FAOS Sport subscale was not included in the 12-week outcome assessment (Fig. 6).
Table 3.
The Foot Function as measured by the Foot and Ankle Outcome Score (FAOS) was similar for both groups at the baseline and at 26-weeks. At the 12-week post-operative follow-up, the FAOS score was significant better in the Early weight-bearing group compared to the Control group.
| Foot and Ankle Outcome Score (FAOS) subscale | 0-week |
12-week |
26-week |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control 6-week NWB |
Early 2-week NWB |
P-value | Control 6-week NWB |
Early 2-week NWB |
P-value | Control 6-week NWB |
Early 2-week NWB |
P-value | |||||||
| Symptoms | 58.3 | 26.1 | 47.5 | 23.9 | 0.136 | 62.1 | 16.1 | 76.9 | 13.6 | ∗0.001 | 81.9 | 11.8 | 80.5 | 15.6 | 0.715 |
| Pain | 44.0 | 23.8 | 47.5 | 28.8 | 0.633 | 66.4 | 19.3 | 78.6 | 11.4 | ∗0.013 | 82.2 | 15.6 | 85.5 | 12.9 | 0.442 |
| ADL | 59.7 | 29.4 | 53.0 | 25.6 | 0.399 | 61.4 | 17.3 | 81.4 | 7.6 | ∗0.000 | 84.3 | 10.6 | 86.0 | 8.2 | 0.555 |
| Sport | 52.1 | 29.7 | 39.8 | 26.7 | 0.132 | n/a | 76.7 | 15.9 | 77.6 | 13.7 | 0.836 | ||||
| QOL | 41.2 | 30.2 | 31.1 | 23.6 | 0.202 | 49.1 | 20.4 | 72.6 | 20.7 | ∗0.000 | 82.4 | 11.2 | 81.4 | 14.9 | 0.790 |
P-values are represented as italics.
Figure 6.
Significantly better FAOS in early weight-bearing was noticed at 12-weeks post-surgery.
Discussion
To date, there are no universal guidelines or standardized protocols for post-operative rehabilitation after hallux valgus surgery. The rehabilitation regime can range from ultra-conservative casting and non-weight bearing walking for 3-months to immediate full weight bearing walking on day 0 of surgery. Rehabilitation differs depending on the procedure performed; the endoscopic-assisted soft tissue procedure examined in this study typically consists of a 6-week non-weight bearing period as proposed by the original authors [25].
This study echoed previous studies in that the endoscopic-assisted distal soft tissue procedure effectively treats hallux valgus deformities [18,21]. Both groups had good radiological and clinical results at 26-weeks follow-up that was significantly better than the pre-operative baseline (Table 1). Early weight-bearing walking at 2-weeks after did not increase implant failure (such as premature breakage/loosening of the 1,2 inter-metatarsal positional screw) or recurrence rates; dispelling one of the major concerns of starting early rehabilitation.
In addition, early weight-bearing had a better function at 12-weeks including fewer symptoms like stiffness, less pain, better performance in activities of daily living and a generally better quality of life [26] (Fig. 6). This suggests that allowing early mobilization is not only convenient for the patient, it also accelerates the overall rehabilitation progress. Although the foot function in the control group eventually catches up, the early weight-bearing group would theoretically be able to enjoy better function 3–4 months earlier.
Limitations
Rehabilitation regimes are different for different surgical procedures. Some arthrodesis and osteotomy procedures are held with small (2 mm) cannulated screws, while others utilize locking plates and arthrodesis nails. The variations in post-operative rehabilitation is large, with some regimes requires post-operative casting while others allow immediate fully weight bearing walking. There is minimal high-quality evidence to suggest the best protocol. As stated in the introduction, the results from this study should only be applied to the patients who have undergone the endoscopic-assisted distal soft tissue procedure [2,18]. The authors believe it can also act as a reference for other soft tissue reconstruction for hallux valgus, but probably cannot be used to guide rehabilitation in patients undergoing an osteotomy or fusion type procedure.
The follow-up in this study is relatively short, although the authors initially believed that the intervention mostly affects the initial 6 postoperative weeks, we believe that there is a slight chance the initial post-operative period may have a more lasting effect. A study with a >5-year follow-up should provide a more accurate long-term prognosis. Nonetheless, our results show that all radiological and clinical parameters were similar at 26-week follow-up, thus we postulate that the trajectory and long-term results of the participants should be somewhat similar.
Conclusion
The results show that it is safe to allow early weight-bearing at 2-week post hallux valgus surgery, and earlier ambulation will reduce post-operative pain and accelerate regain of function. This implies that adopting this accelerated weight-bearing rehabilitation timeframe; patients can quickly resume a productive role in society.
Conflict of Interest
The authors have no conflicts of interest to disclose in relation to this article.
References
- 1.Yucel I., Tenekecioglu Y., Ogut T., Kesmezacar H. Treatment of hallux valgus by modified McBride procedure: a 6-year follow-up. J Orthop Traumatol. 2010;11(2):89–97. doi: 10.1007/s10195-010-0092-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ling S.K.K., Lui T.H. Arthroscopic-assisted correction of hallux valgus deformity. In: Scuderi G.R., Tria A.J., editors. Minimally invasive surgery in orthopedics. Springer International Publishing; 2016. pp. 1–7. [Google Scholar]
- 3.Schwitalle M., Karbowski A., Eckardt A. Hallux valgus in young patients: comparison of soft-tissue realignment and metatarsal osteotomy. Eur J Pediatr Surg. 1998;8(1):42–46. doi: 10.1055/s-2008-1071117. [DOI] [PubMed] [Google Scholar]
- 4.Park Y-b, Lee K-b, Kim S-k, Seon J-k, Lee J-y. Lateral soft-tissue release with medial transarticular or dorsal first web-space approach combined with distal chevron osteotomy for moderate-to-severe hallux valgus. JBJS Essent Surg Tech. 2014;4(4) doi: 10.2106/JBJS.ST.N.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park H.-W., Lee K.-B., Chung J.-Y., Kim M.-S. Comparison of outcomes between proximal and distal chevron osteotomy, both with supplementary lateral soft-tissue release, for severe hallux valgus deformity: a prospective randomised controlled trial. Bone Joint J. 2013;95-B(4):510–516. doi: 10.1302/0301-620X.95B4.30464. [DOI] [PubMed] [Google Scholar]
- 6.Orzechowski W., Dragan S., Romaszkiewicz P., Krawczyk A., Kulej M., Morasiewicz L. Evaluation of follow-up results of McBride operative treatment for hallux valgus deformity. Ortop Traumatol Rehabil. 2008;10(3):261–273. [PubMed] [Google Scholar]
- 7.Mostafa M.F., El-Adl G. Distal soft tissue realignment and proximal metatarsal countersinking osteotomy for moderate to severe hallux valgus. Foot. 2012;22(3):186–193. doi: 10.1016/j.foot.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Mittal D., Raja S., Geary N.P.J. The modified McBride procedure: clinical, radiological, and pedobarographic evaluations. J Foot Ankle Surg. 2006;45(4):235–239. doi: 10.1053/j.jfas.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Mcbride E.D. A conservative operation for bunions. J Bone Jt Surg Am Vol. 2002;84(11) doi: 10.2106/00004623-200211000-00028. [DOI] [PubMed] [Google Scholar]
- 10.Martínez-Nova A., Sánchez-Rodríguez R., Gómez-Martín B., Escamilla Martínez E., Expósito-Arcas A., Novel-Martí V. The effect of adductor tendon transposition in the modified McBride procedure. Foot Ankle Spec. 2008;1(5):275–279. doi: 10.1177/1938640008324406. [DOI] [PubMed] [Google Scholar]
- 11.Lee H.-J., Chung J.-W., Chu I.-T., Kim Y.-C. Comparison of distal chevron osteotomy with and without lateral soft tissue release for the treatment of hallux valgus. Foot Ankle Int. 2010;31(4):291–295. doi: 10.3113/FAI.2010.0291. [DOI] [PubMed] [Google Scholar]
- 12.Huang E.H., Charlton T.P., Ajayi S., Thordarson D.B. Effect of various hallux valgus reconstruction on sesamoid location: a radiographic study. Foot Ankle Int. 2013;34(1):99–103. doi: 10.1177/1071100712464356. [DOI] [PubMed] [Google Scholar]
- 13.Harris N.J., Scott B., Smith T.W. A further modification to the McBride procedure for hallux valgus using the acufex tag system to reattach the adductor hallucis. Foot Ankle Int. 1997;18(1):57–58. doi: 10.1177/107110079701800113. [DOI] [PubMed] [Google Scholar]
- 14.Gould J.S., Ali S., Fowler R., Fleisig G.S. Anchor enhanced capsulorraphy in bunionectomies using an L-shaped capsulotomy. Foot Ankle Int. 2003;24(1):61–66. doi: 10.1177/107110070302400110. [DOI] [PubMed] [Google Scholar]
- 15.Arbab D., Wingenfeld C., Frank D., Bouillon B., König D.P. [Distal soft-tissue procedure in hallux valgus deformity] Operat Orthop Traumatol. 2016;28(2):128–137. doi: 10.1007/s00064-015-0406-8. [DOI] [PubMed] [Google Scholar]
- 16.Ling S.K.K., Lui T.H., Yung P.S.H. Arthroscopic lateral soft tissue release for hallux valgus. J Foot Ankle Surg. 2020;59(1):210–212. doi: 10.1053/j.jfas.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Ling S.K.K., Lui T.H. 2016. Arthroscopic-assisted correction of hallux valgus deformity; pp. 803–809. [DOI] [PubMed] [Google Scholar]
- 18.Lui T.H., Ling S.K.K., Yuen S.C.P. Endoscopic-assisted correction of hallux valgus deformity. Sports Med Arthrosc Rev. 2016;24(1):e8–e13. doi: 10.1097/JSA.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 19.Li S., Myerson M.S. Evolution of thinking of the Lapidus procedure and fixation. Foot Ankle Clin. 2020;25(1):109–126. doi: 10.1016/j.fcl.2019.11.001. [DOI] [PubMed] [Google Scholar]
- 20.Lenz C.G., Niehaus R., Knych I., Eid K., Borbas P. Scarf osteotomy for hallux valgus deformity: radiological outcome, metatarsal length and early complications in 118 feet. Foot Ankle Surg. 2020 doi: 10.1016/j.fas.2020.01.002. In press. [DOI] [PubMed] [Google Scholar]
- 21.Ling S.K.K., Lui T.H. Endoscopy-assisted hallux valgus correction provides sustainable long-term >10-Year outcomes. Arthrosc J Arthrosc Relat Surg. 2018;34(6):1958–1963. doi: 10.1016/j.arthro.2017.12.017. [DOI] [PubMed] [Google Scholar]
- 22.Williamson M., Iliopoulos E., Jain A., Ebied W., Trompeter A. Immediate weight bearing after plate fixation of fractures of the tibial plateau. Injury. 2018;49(10):1886–1890. doi: 10.1016/j.injury.2018.06.039. [DOI] [PubMed] [Google Scholar]
- 23.Chua M.J., Hart A.J., Mittal R., Harris I.A., Xuan W., Naylor J.M. Early mobilisation after total hip or knee arthroplasty: a multicentre prospective observational study. PloS One. 2017;12(6) doi: 10.1371/journal.pone.0179820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ling S.K.K., Chan V., Ho K., Ling F., Lui T.H. Reliability and validity analysis of the open-source Chinese foot and Ankle outcome score (FAOS) Foot. 2017;35:48–51. doi: 10.1016/j.foot.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Lui T.H., Ng S., Chan K.B. Endoscopic distal soft tissue procedure in hallux valgus surgery. Arthrosc J Arthrosc Relat Surg. 2005;21(11):1403. doi: 10.1016/j.arthro.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 26.Schuh R., Hofstaetter S.G., Adams S.B., Jr., Pichler F., Kristen K.H., Trnka H.J. Rehabilitation after hallux valgus surgery: importance of physical therapy to restore weight bearing of the first ray during the stance phase. Phys Ther. 2009;89(9):934–945. doi: 10.2522/ptj.20080375. [DOI] [PubMed] [Google Scholar]